Based on the Kano model, the reality of innovation is that features that once were a “delighter” (remember the first power windows in cars?) over time in the eyes of the consumer become “table stakes”.
The same holds true for telehealth — in the 1990s and 2000s academic medical centers used telehealth to provide easier access to their specialty care services to rural populations. More health systems jumped on board in the 2010s and the Covid-19 health crisis catapulted all of us into the telehealth age.
But many healthcare leaders dismissed telehealth merely as a “stop gap” measure for Covid, not as the critical delighter for the modern healthcare consumers that it has evolved to.
As the industry (and its leaders) are now chasing the sweet temptations (and value) of AI, it is important that Healthcare CEOs turn their attention to the “value at hand” vs. giving in to the seduction of a new technology and the pressure of “me too” adoption.
In the eyes of many healthcare consumers, Telehealth is no longer merely a “delighter” — it has become table stakes and in this Telehealth Tuesday article I lay out the three things CEOs should and should not be doing.
Side note: Telehealth is not just about live video visits. It includes various forms of virtual care services and in totality they are becoming more and more critical to drive patient engagement and health outcomes.
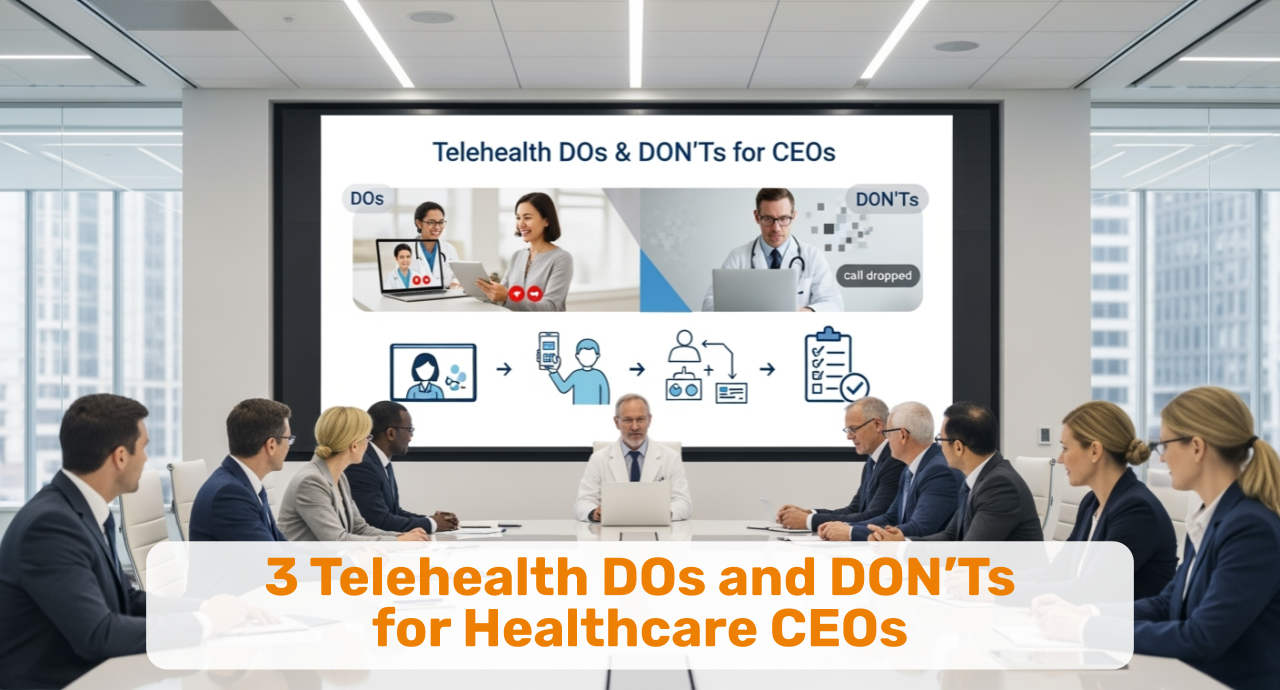
DO treat Telehealth as an alternative care delivery modality.
One of the most important mindset shifts for healthcare leaders is to fully embrace that telehealth is unlike any other organizational change they have experienced or led in the past. In its effect on the organization, even the digitization of the medical record pales in comparison.
The good news is that telehealth, by far, does not have to be in any shape or form as painful as the introduction and integration of an EHR system. Because first and foremost telehealth is NOT about the integration of a technology.
Side note: The purpose of early EHRs was to maximize billing charges. The purpose of telehealth used correctly is to facilitate an extraordinary patient-clinician experience. Big difference!
First and foremost, telehealth is about improving, expanding the delivery of care.
At its essence, telehealth is simply delivering care at a distance. It is a clinical tool that clinicians can use at their discretion. And it’s about building and integrating a parallel set of care delivery processes that uses communications technology — as a tool.
DO think of Telehealth as a multidisciplinary effort
Secondly, once Telehealth is understood as a new care delivery modality — complementary to in-person care — it becomes obvious that EVERYONE in the organization will need to be involved. From scheduling to billing, from nursing to prescriptions, from the helpdesk to compliance and marketing.
To build a set of successful Telehealth processes, it takes everyone in your organization to participate in the effort, including the definition of new workflows, such as the 7 new telehealth workflows for video visits that include scheduling, onboarding, rooming, the visit, post visit, follow-up and billing.
DO leverage Telehealth to achieve your strategic objectives
Thirdly, in working with numerous healthcare leaders over the past decade, they all gained a key insight: that telehealth is a tactical tool that astute leaders can use to advance virtually ALL of their strategic objectives.
Today’s healthcare organizations typically structure their telehealth strategy around the six common pillars of service, quality, people, finance, growth, and community.
Telehealth offers numerous opportunities to create strategic success through better access, better outcomes, expanded geographic reach, reduced no shows, reduced stigma, increased patient engagement, reduced burnout, and more.
For more information see the “Seven Pillars of Telehealth Value”.
DON’T mistake Telehealth for a fad or stop-gap measure.
Telehealth, when it first came into widespread use in 2020 at the beginning of the Covid-19 health crisis, was seen by many as a stop-gap measure; an inferior method to delivering care that was still better than the alternative of no care.
Many organizations were not prepared for a large-scale use of telehealth and struggled to deliver quality experiences for patients and clinicians. Most so-called “telehealth” visits were conducted over the phone vs. the benefit of high-quality live video. Others, who had used telehealth prior to the start of the pandemic, quickly scaled their ability, some up to 5,000 virtual care visits a day.
By now it’s clear that Telehealth is here to stay. The toothpaste is not going back into the tube. The cat is out of the bag. The train has left the station. You get the idea.
Aside from numerous telehealth-only service providers (often lavishly promoted to patients by the patients’ health insurance), many services that initially focused on targeting self-insured employers are now switching to a “virtual first” model en masse.
Amazon is now offering virtual first visits through its acquisition of One Medical. Teladoc is heavily promoting its virtual visit service. And while Walmart, Walgreens, and other industry juggernauts have tried and failed, venture capital-funded startups targeting men’s health, women’s health, and weightloss are offering direct-to-consumer virtual only services that offer convenience and speed.
And who are those companies targeting? Your patients!
In addition, the aforementioned Modern Healthcare Consumer will not only be delighted by the availability of telehealth options — they’ll be expecting and demanding them very soon — from your clinicians!
DON’T think that Technology is the solution
In the midst of the complexity to embrace telehealth — what about reimbursement? what about digital literacy? what about clinical efficacy? — it can be tempting to look for a silver bullet, to look for technology as a solution to the multitude of problems.
In “9 out of 10 cases” your IT department will or already has urged you to use your EHR’s embedded video solution. That may be a bad idea and you really should involve clinicians and patient representatives to select a solution that offers a great user experience — and not simply the benefit of one less vendor contract to administer.
Side Note: There is no need for integration between video visits and the EHR. There is no need for interoperability either.
Remember: You are in the business of delivering care. Telehealth is the delivery of care at a distance. So why would you not use the best solution available to enable the clinicians to deliver their extraordinary care at a distance?
Alas, while good, user-friendly, reliable, secure technology is essential to a great telehealth experience, it is only a small piece of the overall puzzle.
Much of the performance of telehealth and the experience of clinicians and patients depends on the not-so-technical workflows, policies, training, and support.
Many superb telehealth solutions can greatly help with the workflow and minimize the need for training and support. Still, they cannot cover all workflows, policies, and technology needs.
After all, telehealth is not about the technology.
DON’T believe patients don’t want telehealth.
Based on our experience, the statement that “my patients don’t really want telehealth” stems from a multitude of factors and has a number of root causes.
The most common is that it is a statement made by clinicians who for different reasons may not feel comfortable using video to care for their patients. It is most likely that they were never properly oriented as to how to use this novel care delivery modality.
Most every clinician learned in their training the “bedside manners” of interacting effectively with patients and family members. But when Covid hit, nobody took the time to explain how to master the “webside manners” — how to powerfully communicate with patients over video.
Nobody likes to look foolish, the least of all doctors. Thus many (consciously or unconsciously) try to avoid telehealth and rationalize away the need for an interest in video televisits. Besides, if the clinician feels awkward or frustrated with the technology, patients will not have a good experience. That does not mean that they don’t want telehealth. It just means they don’t want telehealth with that clinician.
On the other hand, in many rural areas, connectivity and the availability of suitable technology can be a challenge. But the challenge of access to technology, “internet minutes” and digital literacy is not limited to rural areas. Many health centers in urban locations are reporting similar challenges, despite a seemingly better infrastructure.
Applying the DOs and DON’Ts
With telehealth being here to stay, here are the six most effective ways for any healthcare leaders to ensure that their clinicians and their patients are getting the most value out of telehealth:
-
Provide Webside Manners and Virtual Exam Training for all clinicians.
-
Invest in the design and training of the seven critical telehealth workflows.
-
Create and communicate a Telehealth Vision that inspires and excites to make it clear that telehealth is not going away.
-
Create a set of strategic telehealth objectives that will help you to achieve your overall strategic objectives.
-
Assemble a multi-disciplinary telehealth steering team to direct and guide the activities to fully integrate telehealth into your care delivery system.
-
Engage all clinicians in rethinking care delivery in a hybrid care environment.
Finally, DO reach out to me if you need assistance with any of these activities. We can provide proven toolkits, assessments, templates, training, and mentoring. You DON’T have to figure this out all by yourself.








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.