“The bitterness of poor quality remainslong after the sweetness of low price is forgotten.”— Ben Franklin
Selecting your EHR/EMR’s embedded telehealth offering seems to be a straightforward decision: all clinicians already have access to the software and the telehealth functionality is embedded into the EHR and thereby “integrated”.
But I have to ask: haven’t we learned anything in the past 20 years? We now know that EHRs were designed and are really good at capturing care activities to create accurate billing records so that each service can be appropriately and accurately billed.
Where most EMRs have failed clinicians in the past is in the lack of support to facilitate and support the care delivery and care decision making processes. The process for clinicians to capture what they did for the patient is oftentimes cumbersome and runs counter to the paradigms of physicians.
So how can we think that this time around, EHRs will do a better job? Actually most larger EHRs have cobbled together quick solutions over the past years (often using 3rd party vendors) in response to the pressure to also have telehealth functionality. But more often than not, these were shoe-horned in afterthoughts vs. thoughtful integrations.
On the other hand, at least a dozen or so excellent telehealth solutions have been developed by agile, responsive startups over the past 10 years that create beautifully simple and intuitive workflows that allow clinicians to practice on top of their license and, most importantly, create a seamless, easy experience for patients to receive their care via video. These often were developed by physicians for physicians with the sole purpose of creating a great experience for clinicians and patients alike.
But In many organizations the decision to select the technology often falls solely with the IT department and unless some “rogue” physician somehow got a different vendor into the organization, most health IT leaders push strongly towards leveraging the EHRs telehealth functionality. Since clinicians are typically not experienced in the technology selection process, most just shrug their shoulders and accept the decision that was made for them.
Why good CIOs make bad decisions
Now I’m not saying that CIOs are intentionally trying to make physicians’ and patients’ lives harder: “The road to failure is paved with good intentions.”
Rather we need to take a look at the system that gave birth to these decisions. As one of my favorite sayings goes: “Every system is perfectly designed, to get the results it gets.” We need to look at the systems that provided the incentives for CIOs to act this way.
Here are three common themes that drive health IT leaders to making that recommendation of selecting their EHR vendor’s telehealth solution.
1. Being single-mindedly fixated on integration: Integration is a big buzzword and trigger in Health IT circles and I’m very sympathetic to the origins of this relentless pursuit of integration. In many organizations in the 1990s and 2000s there was a wild growth of IT technologies as virtually every department purchased their own solution, grew accustomed to it — and then wanted that solution to be integrated with other solutions, so that data could easily flow in and out.
So Health IT departments spent a lot of time and money on creating interfaces to allow for the integration of these disparate, isolated point solutions. To make things worse, many departments had bought different solutions to solve similar problems. As Health IT cost skyrocketed, healthcare leaders recognized the need for centralized management and support of all technologies and gave IT the mandate to “consolidate” to “integrate” and to reduce the number of vendors and technologies, because in those days of in-house hosted solutions (vs. the cloud-based world we are in now) the ongoing support was quite labor and cost intensive.
Therefore, when health IT leaders are hearing anything about a technology that affects healthcare delivery, the immediate auto-response is to demand that the solution integrate with the EHR (we’ll touch on the actual need for integration another time).
2. Trying to consolidate everything into as few vendors as possible. As illustrated in the brief historical treatise above, the wild growth of vendor relationships and the support of multiple technologies with a multitude of vendors is still back in today’s health IT leaders minds, as they were starting out their careers when that happened.
What is often overlooked is that most vendors have different support call centers for their diverse line of offerings and product team C often does not know anything about product team A. Secondly, in today’s cloud-based SaaS model, technical support of the infrastructure is, aside from keeping a smooth network running, nonexistent. Thirdly, really great innovative leaders are offering far superior support for their products than the entrenched, large EHRs that know quite well about the high cost of switching to another EHR.
Thus to limit solutions to just a few vendors is by far not as advantageous as it was even 10 years ago, so that argument does not hold.
3. Treating telehealth as a commodity tool. But the most egregious mistake for health IT leaders to make is to think of telehealth as some kind of infrastructure commodity like email or the phone system. Whereas in reality these days telehealth is a clinical tool where the workflow experience should be optimized for both users, patients and clinicians.
That mindset may then lead quite naturally to different solutions for telehealth. E.g., one solution for inpatients and rounding on the floor, a different one for patients at home and another different one for a TeleStroke evaluation in the ER.
Why CIOs can get away with it
Here are four observations as to why CIOs are not being called out on selecting a solution that seemingly does not fit the needs of the clinicians and the needs of the patients.
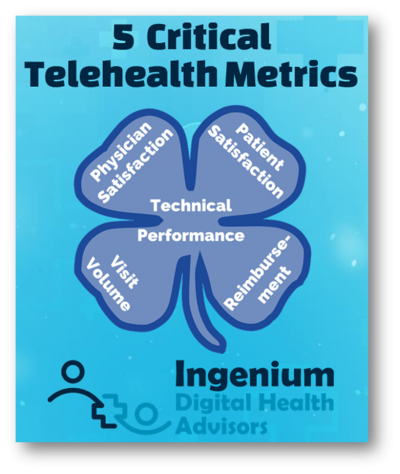
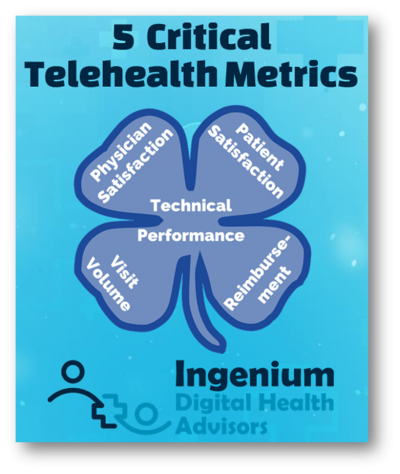
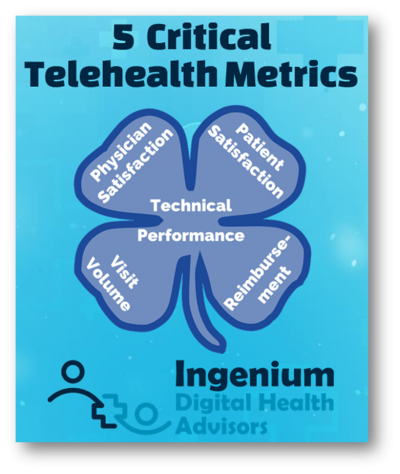
1. Leadership does not measure telehealth success: As the adage goes, “you can’t manage what you don’t measure” and most organization have no metrics, no dashboards in place to evaluate the five core telehealth success metrics such as visit volumes, reimbursement by modality & specialty, physician satisfaction, patient satisfaction, and technical issues.
And it’s not merely about collecting and displaying the data; every collected metric should have an owner, standardized collection and analysis rules, a target, and predefined actions if the target is not met.
2. Physicians don’t know it could be better: Many clinicians got thrown into telehealth because of Covid, and many thought or hoped it would only be temporary. But most physicians never experienced telehealth anywhere else and few are on the receiving end.
In most organizations the training was: here’s a webcam and a video software — Go! There was no orientation on webside manners, no definition of clinical or operational workflows. And even now, as the crisis is coming to an end, very few organizations are making a conscious effort to optimize their existing telehealth services. Mainly because no one is measuring the success (or rather: the dismal performance) of telehealth.
3. Physicians avoid telehealth altogether: With many organizations still working under a fee-for-service model, the payors’ decision at the height of the pandemic to allow for reimbursement for telephonic care was a well-intentioned decision. The lack of a video-compatible technology and connectivity should not have been a hindrance to delivering much needed care, even if it was only over the phone.
But many clinicians saw this as an excuse to abandon video-based telemedicine, which bears quite a few advantages. At the height of the health crisis I came across numerous organizations that were doing 80%, 90% telehealth of which 99% was telephonic. In the long-run this simply cannot be good medicine. Physicians know this and many are pushing towards going back to in-person visits only.
4. Patients just accept it: Patients have a centuries-long history of accepting the doctor’s advice. Even though patients are quickly transitioning to becoming “modern healthcare consumers”, many still defer to “the higher authority” and, because it’s about their health, put up with a lot of things that they would not tolerate in other service settings.
Similar to physicians they also often do not know better, though that is quickly changing as during the Covid-19 health crisis patients have often used multiple different telehealth services and can now compare the experience.
As I wrote about a few weeks ago, patients are now firing their doctors if they cannot offer the expedient convenience that many patients have come to experience through telehealth.
The Solution to Telehealth Woes
To get the most value out of telehealth, it is necessary for leadership to take the helm and set a clear course toward the future, which is Hybrid Care. This does not mean that the requests of health IT leaders should be ignored. But it is time to reverse the decision making process.
2. Use metrics to manage the performance of all Telehealth Services. It is absolutely essential to establish a leadership-driven telehealth performance management system. Without it, your organization is flying in the dark at best.
3. Select the best telehealth solution(s) based on systematically developed requirements. Armed with the knowledge about the desired ideal workflows, shopping for the telehealth solution that is the best fit becomes much easier.
What has your experience with your EMR’s telehealth “feature” been? If you are using it — are you periodically collecting satisfaction data?








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.







Leave A Comment