Two years after the Covid-19 health crisis, telehealth is experiencing a renaissance in the sense that many healthcare organizations are now realizing that telehealth is not merely stop gap measure, but a viable virtual care delivery option to meet patients increasing needs and expectations.
Success in Telehealth, however, is not about picking the right technology or fretting about an integration of the telehealth solution with the EHR. Success in telehealth depends mostly on the workflows — and the training of staff on the workflows.
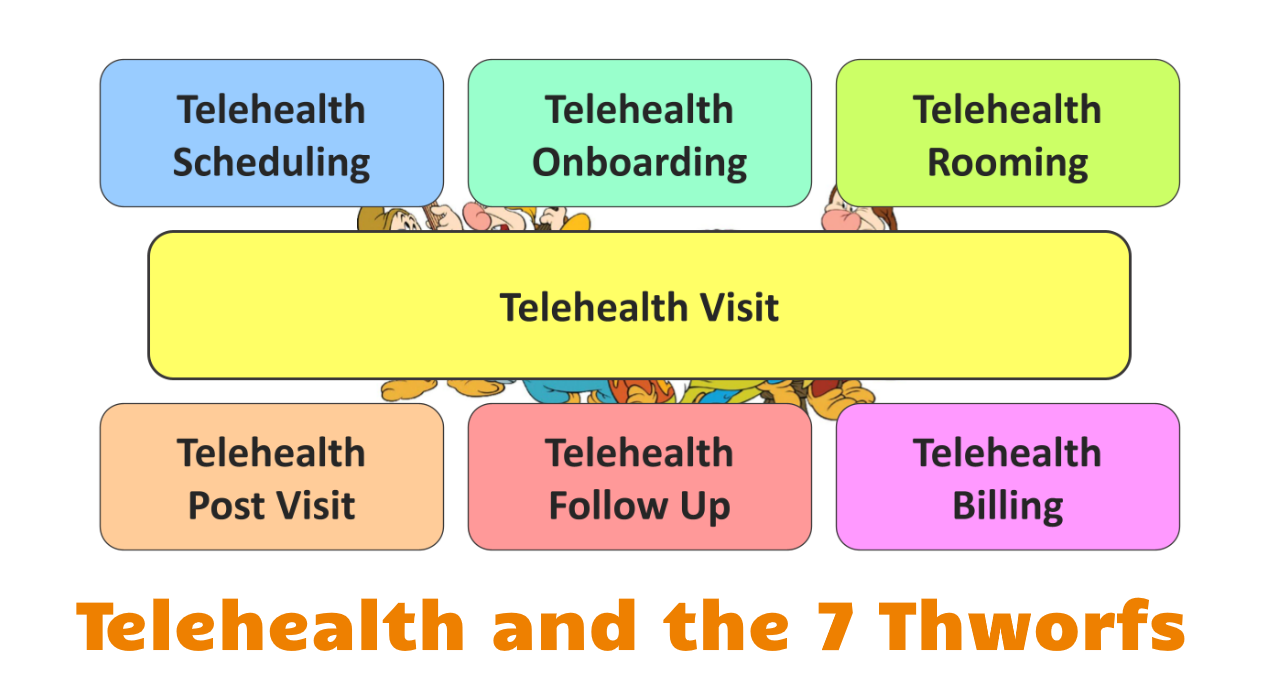
The seven main Telehealth Workflows (or “thworfs” for short) are:
- Telehealth Scheduling
- Telehealth Onboarding
- Telehealth Rooming
- Telehealth Visit
- Telehealth Post Visit
- Telehealth Follow Up
- Telehealth Billing
When designing telehealth-specific workflows for those 7 different areas, it is helpful to keep in mind that the same seven workflows already exist in the traditional “in-person” environment. Creating the same experience, however, when the patient is not in the clinic, is inherently more difficult, which is why the meticulous definition of each step is critical, as it is hard to correct anything that does not go according to plan on the patient’s end.
One more note before we get started: typically, we define telehealth as “delivering care at a distance” . While the seven telehealth workflows apply to a variety of different telehealth modalities, for the purpose of this article we will be focusing on the “live audio/video visit” form of telehealth.
Without further ado, here come the seven Thworfs: Timey, Newbie, Roomy, Vizzy, Posty, Folly and Billy.
1. The Scheduling Thworf (“Timey”)
It is understood that in healthcare virtually every visit has to be scheduled – including for same-day appointments or to accommodate walk-ins by fitting them into the clinician’s schedule.
The definition of a scheduling workflow should in its elementary form clarify (1) how to ensure that a telehealth visit is appropriate and (2) how the appointment on the clinician’s calendar is marked as a telehealth visit.
But even basic telehealth visits come in different flavors – e.g., televisits directly to the patient’s home or site-to-site televisits, where the patient is checking in at a distant site (where she also would have to be “roomed”). For the latter scenario, the scheduling workflow must describe how to block the appointment on the calendar of the site that will be hosting the patient.
Another innovative scheduling scenario involves patients who are calling to cancel or reschedule and offering them a telehealth visit instead.
2. The Onboarding Thworf (“Newbie”)
This workflow is a bit unique to telehealth although in traditional in-person care this would define all the steps to undertake for a new patient.
The same principle also applies to the Telehealth Onboarding Workflow, only that the patient is most likely not going to set foot into the clinic, so any paperwork needs to be completed virtually.
In addition, telehealth onboarding also applies to established (and new) patients that are doing a telehealth visit for the first time.
As the Covid-19 health crisis catapulted everyone into telehealth, we quickly established a “Telehealth TechCheck” protocol, to ensure that patients had the right technology and knew how to use it prior to their telehealth appointment. The details of that TechCheck should also be documented as part of the Onboarding Thworf.
3. The Rooming Thworf (“Roomy”)
The process describing rooming encompasses everything that occurs in the minutes prior the patient’s connection with the clinician. I.e., this typically includes at a minimum the (virtual) check-in process (“hey, I’m here and ready to see my doctor”); the collection of vitals, changes in medications, and recording of the chief complaint; and letting the clinician know that the patient is ready for their visit.
The Rooming Telehealth Workflow should also describe what happens when things don’t go according to plan — e.g., when the patient does not show up (you can call them and try to recover from the no show), or when the patient is having technical difficulties connecting (let’s get our TechCheck expert on the line), etc.
Just like with rooming in the in-person world, any challenges should be resolved as to not impact the clinician’s visit or wasting their time.
4. The Visit Thworf (“Vizzy”)
While this telehealth workflow is at the core of telehealth, it is actually the least interesting (dare I say, boring). If everything was done right in the three preceding workflows (including the Telehealth TechCheck), the visit is almost a none-event — i.e., very close to a typical in-person encounter.
The description of the workflow is typically mainly a user guide for the clinician on how to properly use the telehealth technology — how to start the visit; invite the patient from the waiting room into the visit room; share the screen; send files; text information; collect copays; ask the patient to complete a form; import information shared by the patient into the EHR; etc.



5. The Post Visit Thworf (“Posty”)
For the workflows after the clinician and patient part ways, we are differentiating between what happens immediately after the visit (i.e., what typically would happen in an in-person environment after your visit with the clinician is done) vs. what happens in the days or weeks thereafter.
The imminent activities after the visit could include talking to a nurse or clarifying referrals, prescriptions, or tests that were ordered. Another typical post visit activity includes scheduling the next appointment, since this almost always happens right after the visit in the “in-person care world”.
6. The Follow-Up Thworf (“Folly”)
The Telehealth Follow Up Workflow focuses on the activities in the days or weeks following the appointment. Depending on the clinic operations or the specialty typical activities include communication with the patient about test results, sharing of clinical notes, or additional assistance for patients to schedule and conduct any ordered tests.
The best place to start looking for what should be in scope for this thworf is to assess what happens after an in-person visit.
7. The Billing Thworf (“Billy”)
While the workflow for telehealth billing is not really different from the billing for in-person visits, Telehealth Billing should cover guidance an all things related to billing and is the only workflow that is a little bit out of sequence.
At a minimum Telehealth Billing should provide guidance on how to properly document and code a telehealth visit, depending on the type of service provided and the patient’s insurance. While this could be included in the Visit Workflow, it is best left in the Billing Workflow under the ownership of the billing department.
Other areas of interest could define the process for collecting copays or the collection of payments from self-paying patients.
Finally, a good billing workflow also addresses the steps to dispute claims that were rejected (including sources on what is billable and what is not) and guidance on staying on top of the everchanging regulations at the federal and state level as well as with commercial insurances.
Workflow Definition and Training
The most frustrating breakdowns in telehealth can all be traced back to the absence of well-defined workflows and/or a lack of training of all involved. The above list of seven workflows virtually involves every staff member – from schedulers, front-desk people, and case managers to nurses, clinicians, and the folks in IT.
Not only must these workflows be defined to ensure a non-frustrating telehealth experience for clinicians and patients alike, there also must be a well-defined process for training staff (especially new staff) on these processes and protocols.
A chain is only as strong as its weakest link and oftentimes I’ve found that the blatant absence of clearly defined (and communicated) workflows are what leads to a dismal telehealth experience.
In the fairytale of the (German) Brothers Grimm (“Gebrüder Grimm”) the 7 dwarfs are helpful and kind to Snow White and they, ultimately, safe her from peril. Let your team at your organization create your own fairytale of a fairy tale Telehealth experience for all, by making your seven “thworfs” as helpful as possible.
For over 15 years, Christian Milaster has designed telehealth workflows for a living, so if you need assistance, inspiration, guidance or coaching, reach out to learn how his and his team’s expertise can help you to develop an extraordinary telehealth experience.








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.








Leave A Comment