Remote Physiological Monitoring (RPM) has proven clinical and financial potential, but many programs stall or even fail after the initial rollout.
The difference between RPM that exists and RPM that delivers value comes down to design — how referrals start, how patients are activated, how data informs action, and how clinicians are protected from overload.
High-performing RPM programs are not defined by devices or dashboards. They are built around workflow realism, patient accountability, and decision-grade data that fits clinical practice.
Reminder #1: Technology is only the enabler. Patient care — and influencing patient behavior — is still a human-to-human business.
RPM works best when it is “high-tech enabled high-touch”.
Reminder #2: If you’ve read my previous articles on RPM or seen one of my numerous presentations on RPM, you may recall that we define RPM as
“The continuous or periodic collection, transmission and review of physiological data to inform care decisions.”
The last part is the most important: RPM’s purpose is not to generate revenue and it’s not to promise improvement in chronic conditions. RPM primarily exists to inform care decisions — giving clinicians actionable data and patients the support they need to be well, get well, and stay well.
The RPM Adoption Challenge: Why “Available” Is Not the Same as “Usable”
Across the common chronic conditions of hypertension, CHF, and diabetes programs, the same barriers appear:
-
To patients, RPM referrals feel optional, unclear, or burdensome
-
Patient engagement often drops rapidly after onboarding
-
Clinicians feel flooded with data but short on insight
-
Monitoring work quietly is added already-overloaded care teams
-
The ROI becomes uncertain as participation and scale flatten
Programs that overcome these challenges do so by treating RPM as a care model, not a technology add-on.
A Practical RPM Playbook That Works Across Conditions
1. Make RPM Referrals Easy — and Worth Doing
Successful referrals into RPM increase when RPM is positioned as a clinical tool, not an administrative task.
What works:
-
Clear eligibility criteria tied to specific use cases (e.g., uncontrolled hypertension, recent CHF discharge, insulin titration support), derived from EHR or population health reports.
-
A brief clinician-led explanation to the patient that connects RPM to better control, fewer exacerbations, or earlier intervention
-
Operational handoff to trained and supported technicians after the clinician “sets the why”
When clinicians understand who RPM is for and what problem it solves, referrals become realistic — even in busy clinics.
Before selecting technology, the first question must be: WHY are we doing RPM?
2. Patient Activation Is the Real Leading Indicator
RPM success starts and ends with patient participation. Without consistent readings, there is no clinical value, no intervention, and no sustainable reimbursement.
Effective programs focus on:
-
Expectation-setting at enrollment (“this only works if you participate”)
-
Ongoing support that encourages, praises, trains, reminds, and troubleshoots
-
Accountability loops that address missed readings before disengagement becomes permanent
This approach applies across conditions:
-
Hypertension: normalizing frequent home BP checks
-
CHF: reinforcing daily weight and symptom awareness
-
Diabetes: supporting consistent glucose monitoring tied to treatment decisions
Patient activation is not a soft metric—it predicts outcomes, workload, and ROI.
3. Turn Data Into Decisions and Just-in-Time Interventions, Not Noise
Clinicians do not need more numbers. They need signals that prompt action.
RPM Monitoring nurses also find great value and satisfaction in using the data to coach patients, educate them on the connection between diet and vital signs, between lifestyle choices and how they feel. Just-in-time, not just at a clinic visit.
High-functioning RPM programs (and appropriately selected RPM data management platforms):
-
Emphasize trends over single readings
-
Use monitoring teams to review data daily and escalate only when thresholds or patterns are met
-
Structure alerts so clinicians engage at the point of decision, not data collection
This allows RPM data to inform:
-
Medication titration in hypertension and diabetes
-
Early intervention for fluid overload in CHF
-
Targeted outreach instead of reactive care
The goal is not surveillance — it is clinical clarity and support.
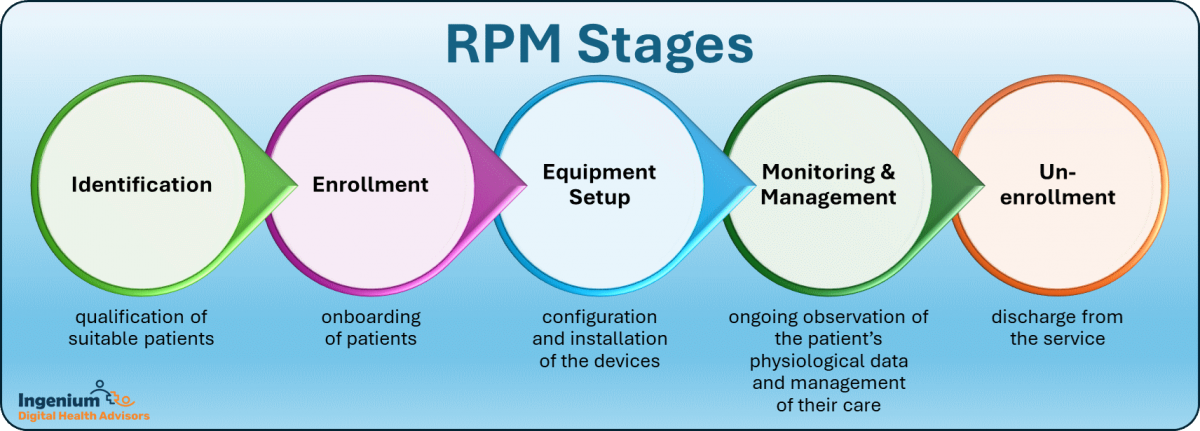
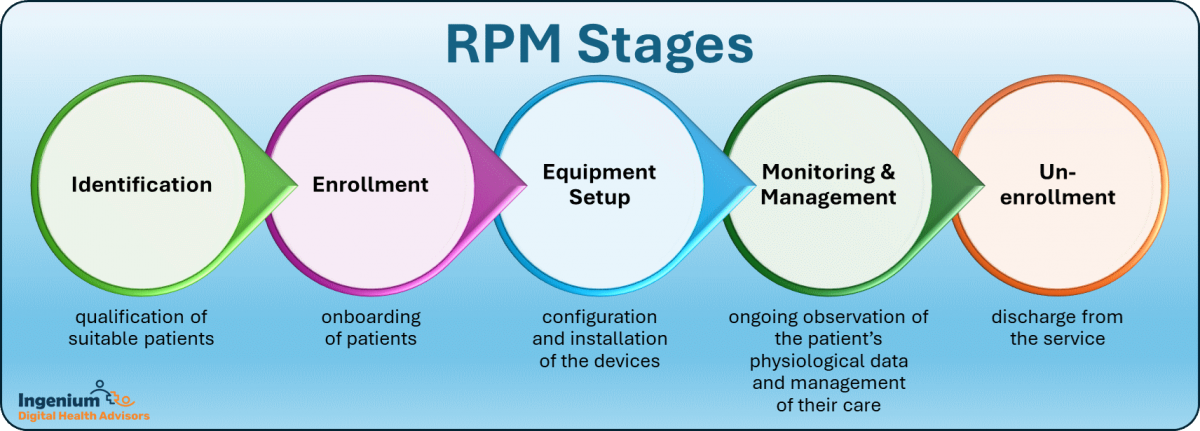
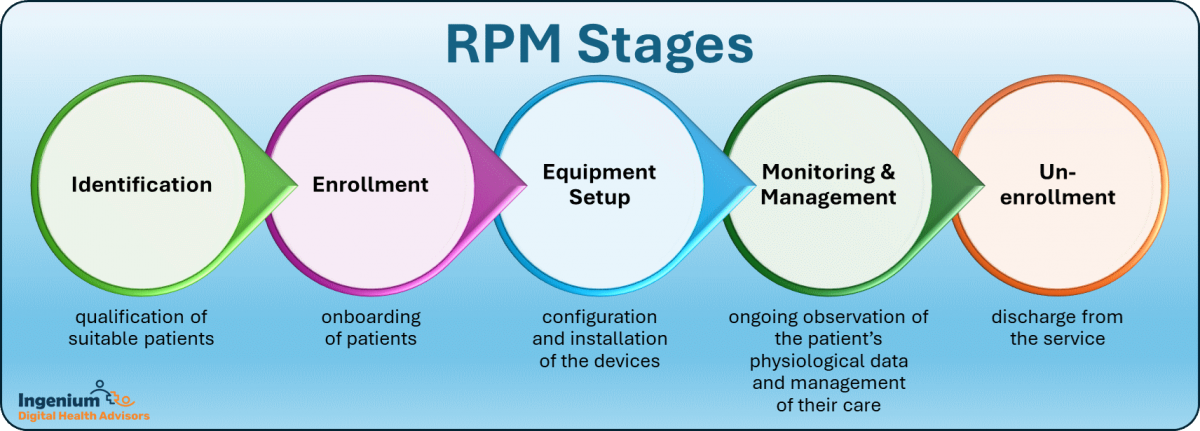
The 5 Stages of RPM. Each Stage requires workflows, templates, forms, procedures, protocols, check lists, etc.
4. Keep Programs Engaged Over Time — and Ready to Scale
Sustained RPM programs share three traits:
-
Defined workflows by role: who enrolls, who monitors, who escalates, who intervenes
-
Strong support infrastructure: so clinicians are not troubleshooting devices or chasing readings
-
A small, meaningful set of Key Performance Indicators (KPIs): e.g., enrollment rate, participation, time-to-intervention, and condition-specific outcomes
Programs that validate these elements through proof-of-concept phases are far more likely to scale without losing momentum.
5. Address Provider Hesitation Head-On
Clinician resistance to RPM is rarely philosophical — it is practical (but sometimes also psychological).
Common concerns include:
-
Fear of added workload
-
Concern about “data overwhelm”
-
Doubts about patient follow-through
-
Uncertainty around billing and compliance
-
Skepticism about the financial and clinical return on investment
Each concern has a direct response:
-
Shift monitoring and first-line outreach away from clinicians. RPM is about optimizing for everyone to practice on top of their license.
-
Train clinicians on the RPM management platform so they can review 6 weeks of data in 60 seconds in preparation for their call or consult with the patient.
-
Use clinician-led enrollment to drive patient commitment. This single element is crucial. If the clinician does not believe the patient can, the patient will meet expectations.
-
Standardize documentation and time tracking — it should not be the clinicians job.
-
Tie RPM performance to outcomes providers care about: demonstrate the clinical difference that it makes (and how it pays for itself, and (under most circumstances) then some)
When proper RPM design, training and support reduces uncertainty instead of adding it, adoption follows (re-read that sentence).
6. Where AI Adds Real Value in RPM
The most valuable AI applications in RPM are operational, not flashy. Also, I first saw “predictive analytics” being applied to RPM data in 2017, so that part is truly not novel.
-
Prioritizing which patients need attention today — that’s a good algorithm, not necessarily AI, unless it takes past interventions into account.
-
Suppressing low-value alerts and highlighting true risk — the good old tried-and-true practice of triage.
-
Supporting consistent outreach and escalation decisions — that’s a reminder engine, not AI.
-
Assisting with documentation and time capture — that’s the true value, as in other clinical AI scribe applications
AI should make RPM quieter, clearer, and more scalable — not more complex. And no, it’s not the major selling point for an RPM solution. Workforce burden is!
7. Build Billing Confidence Through Design, Not Hope
RPM billing success depends on operational discipline:
-
Role-based training that includes clinicians, staff, and billing teams to ensure proper automatic capture of time spent.
-
Clear ownership of consent, documentation, and time tracking
-
Monitoring participation thresholds proactively, not retroactively
-
Routine internal audits to reinforce confidence
When billing is embedded into workflow design, providers stop worrying about compliance and focus on care.
The Bottom Line
RPM succeeds when it respects the clinical reality and moves beyond its ‘shiny solution’ moment. Programs that make referrals into RPM easy, activate patients through a personal connection, deliver actionable data, and protect clinician time are the ones that last — and grow.
Across hypertension, CHF, diabetes, and beyond, the lesson is the same: RPM works when it is designed to work for people first, technology second.
Would you like more information on how to launch or optimize your RPM program? There are some free and some paid resources – let me share those with you.








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.








