This week’s Telehealth Tuesday examines how states can maximize their Rural Health Transformation Program telehealth investments through coordinated implementation rather than fragmented, vendor-driven approaches.
The $50 billion Rural Health Transformation Program represents a once-in-a-generation opportunity to transform rural healthcare delivery and outcomes. With significant portions allocated to telehealth initiatives across states, the stakes couldn’t be higher.
But here’s what history has taught us: funding alone doesn’t guarantee success — only systematic implementation does.
The 10/90 Reality of Telehealth Success
After running over 100 successful (and failed!) telehealth projects across dozens of rural healthcare organizations for the last 15 years, one pattern emerges consistently: technology (and the technology vendors) represents only 10% of telehealth success. The other 90% is systematic implementation — clinical workflow design, change management, staff training, sustainability frameworks, just to name a few aspects.
A reliance on vendors and technology creates what I call the “vendor trap”. Healthcare organizations, including state agencies, often approach telehealth as a technology purchase rather than a comprehensive care delivery transformation initiative. Vendors are incentivized to sell solutions, not to ensure successful long-term adoption and overcome clinical skepticism. Meanwhile, rural healthcare organizations (RHOs) are stretched thin operationally and lack specialized telehealth implementation expertise.
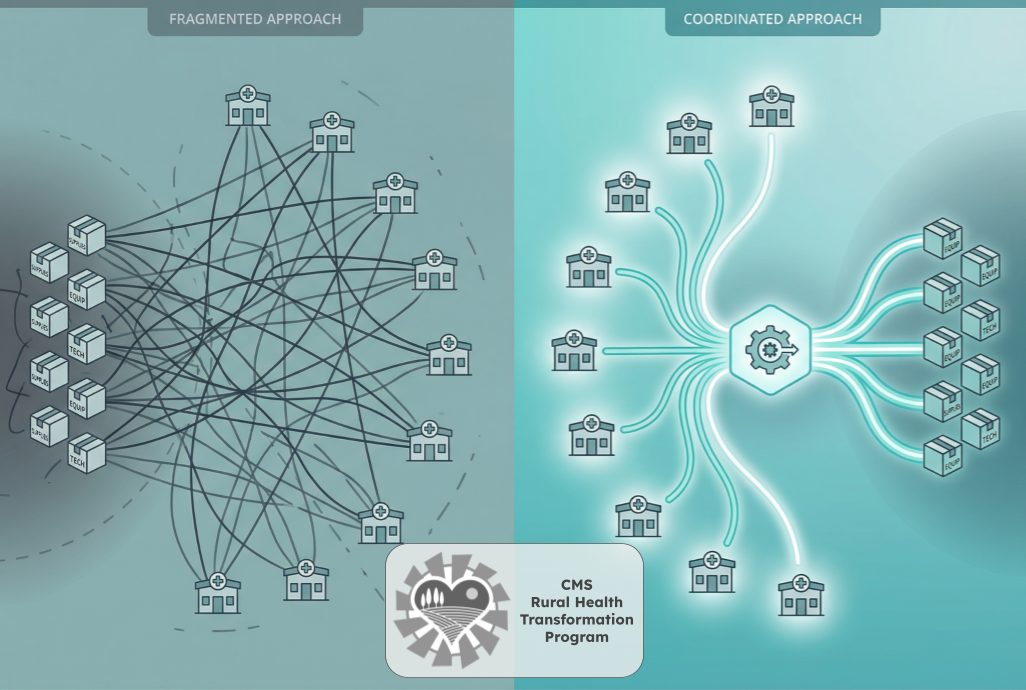
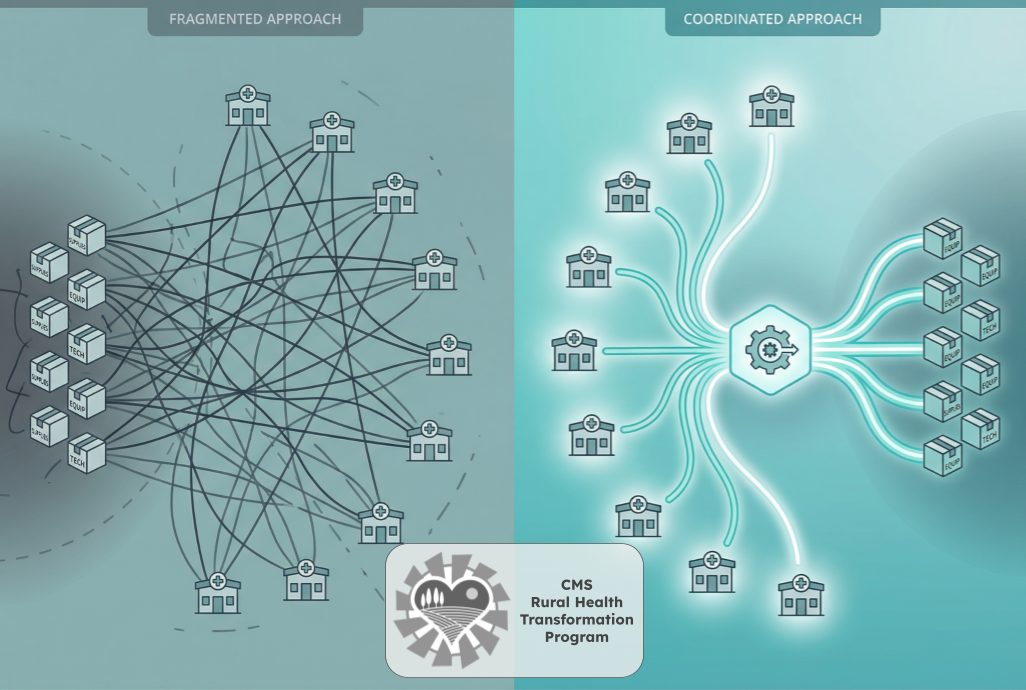
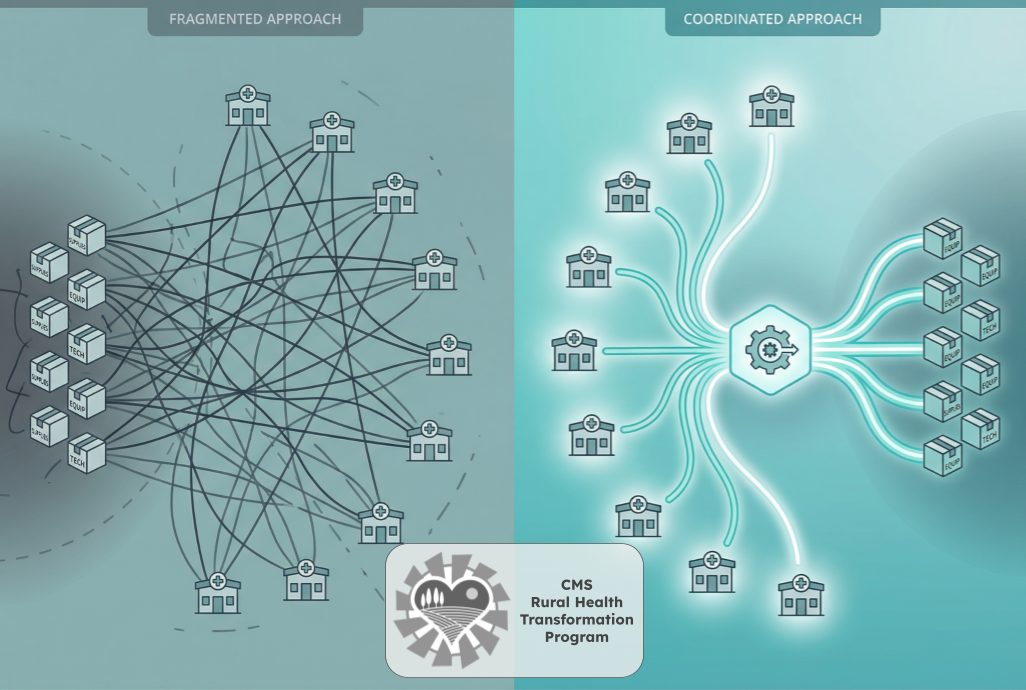
Without coordinated guidance to support telehealth as part of their RHTP initiatives, states risk a fragmented approach where each RHO independently tries to somehow master vendor selection, workflow design, and implementation planning. The result? Duplicated efforts, inconsistent results, wasted resources, and technology purchases that fail to drive meaningful adoption or measurable outcomes.
The RHTP Implementation Challenge
Consider the typical scenario that will play out dozens of times over the next few years: A state receives RHTP funding and distributes allocations to 12-15 interested rural healthcare organizations. Each RHO begins independently evaluating telehealth vendors, conducting demos, developing implementation plans, and designing clinical workflows.
Just looking at the vendors this means the same set of vendors are presenting to 12-15 different organizations, duplicating hundreds of hours of demonstrations and evaluations. Each RHO struggles with the same implementation challenges — workflow integration, staff training, quality metrics, reimbursement optimization — without benefiting from shared learning or coordinated expertise.
The timeline is tight: five years, five budget periods, with high federal accountability standards that expect demonstrable results every September of every year. Rural organizations cannot afford to learn through trial and error when proven implementation expertise already exists.
The SORTOS Solution: State-Orchestrated Excellence
The answer lies in creating what we call SORTOS (State-Orchestrated Rural Telehealth Outcomes Success) or SORTÉ (State-Orchestrated Rural Telehealth Excellence) — a coordinated, state-led approach that applies systematic telehealth implementation science across rural healthcare organizations.
This model establishes an interim, dedicated state telehealth implementation team that orchestrates vendor-neutral, outcomes-focused deployment while maintaining local decision-making authority. Think of it as state coordination, powered by experts, yet with local control.
The key benefits include:
-
Ensuring an approach that creates measurable, sustainable outcomes that satisfy CMS accountability requirements
-
Standardizing telehealth services quality through evidence-based templates and proven frameworks (creating a practice-informed accountability)
-
Enabling peer learning and collective implementation success (by leveraging and multiplying the expertise of those (like Ingenium) who have done this before).
-
Eliminating duplicative vendor evaluations through cohort-based demonstrations (though different RHOs can still select the solution that best meets their needs)
-
Creating procurement efficiencies and potential volume discounts for vendor contracts.
A Four-Phase Implementation Blueprint
Here’s a pragmatic, reality based approach that we have employed dozens of times (and are currently using in a very similar way for an engagement in rural West Virginia).
Phase 0: Establish State Team (Jan – Mar 2026 ) Designate a state telehealth implementation director and engage vendor-neutral expert consultants with proven rural telehealth expertise. Design the RHO interest solicitation and selection process. Create mandatory standardized templates for telehealth maturity assessment, strategy framework development, initiative definition, and budget planning.
Phase 1: Engage Partners (Mar – Apr 2026) Solicit interest from RHOs through self-assessments covering current telehealth status, community needs, and clinical, financial, strategic opportunities. Build an implementation team bench by pre-qualifying telehealth implementation experts based on track record, vendor neutrality, and rural healthcare experience with FQHCs, RHCs, CAHs, and behavioral health organizations.
Phase 2: Assess & Select (Apr – Jun 2026) Conduct comprehensive telehealth capabilities and needs assessments at each selected RHO, developing telehealth strategies with service roadmaps and defining specific initiatives with clear metrics, staffing requirements, technology needs, and budget allocations. Form implementation cohorts clustered by region or service type to facilitate peer learning and coordinated vendor evaluation.
Phase 3: Implement at Scale (starting as soon as May 2026) Launch cohorts with coordinated vendor selection processes — SORTOS facilitates demonstrations and evaluations, but each RHO makes final selections and executes their own contracts. At each organization, systematically design workflows and policies, establish training and support systems, launch proof-of-concept initiatives, refine approaches, deploy at scale, and optimize performance through data-driven improvement cycles.
Why Local Control Matters
This approach maintains the autonomy that rural organizations value while providing the coordination and knowledge they need to succeed fast. The state team facilitates vendor demonstrations for cohorts of organizations rather than individual entities, standardizes evaluation criteria, thus paving the way for volume purchasing discussions. However, each RHO retains decision-making authority and contracts independently with their chosen vendors.
The state coordinates and facilitates rather than dictates — and thus builds sustainable capacity through evidence-based approaches that become state assets, peer learning networks that continue beyond RHTP, and proven frameworks that can be replicated across future initiatives.
The Evidence Base
This approach represents distilled wisdom from over 100 successful — and failed — rural telehealth implementations spanning 15 years across dozens of rural FQHCs, rural health clinics, critical access hospitals, health systems, and behavioral health agencies. It’s grounded in systematic implementation science, not vendor marketing promises or theoretical frameworks.
The approach has been validated through initiatives like Washington State’s Rural Telehealth Initiative, which at one point coordinated 46 projects across 18 organizations, demonstrating the power of systematic coordination over fragmented individual efforts.
Get Your Blueprint!
States have a narrow window to establish coordinated implementation approaches before RHTP funding begins flowing to individual organizations. Once RHOs start independent vendor evaluations and implementation planning, the opportunity for systematic coordination diminishes significantly.
The choice is clear: coordinate for success or fragment toward mediocrity. The rural communities served by RHTP deserve the former.
For states interested in exploring the SORTOS/SORTÉ approach, we’ve developed a comprehensive implementation blueprint that details the frameworks, templates, and coordination strategies outlined above. This resource is available as a public service to support impactful use of RHTP funding for rural health transformation.
If you are working with your state’s RHTP team, contact Christian to get a copy of the blueprint.








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.








