The Rural Health Transformation Program holds the promise to fundamentally reshape rural healthcare delivery — for decades, if done right. States across the country have identified numerous innovative initiatives such as AI-powered diagnostics, remote monitoring systems, telehealth networks that connect specialists to underserved communities.
The technology exists. The funding is available. The question isn’t whether rural healthcare can be transformed, it’s how to drive lasting transformation that outlasts grant cycles and vendor contracts.
Because money alone won’t transform rural health.
We’ve seen this story before. Well-funded initiatives that deliver shiny new technology platforms, only to watch utilization rates hover in single digits. Digital health solutions that sit unused. AI tools that gather dust. Remote monitoring programs that clinicians actively avoid.
The missing piece isn’t better technology or bigger budgets. It’s clinician engagement.
Resistance is not Futile — It’s Justified
Before we label clinicians as “change-averse” or “techno-phobic”, we need to understand something fundamental: their hesitation to embrace change is often completely justified.
Unlike in other industries where a failed software rollout means lost productivity or frustrated customers, healthcare stakes are life and death. When clinicians resist new technology, they’re not being stubborn — they’re being responsible stewards of patient safety.
A financial advisor can afford to learn a new portfolio management system on the job. A physician treating a stroke patient at 2 AM cannot afford to fumble through an unfamiliar AI-driven decision-making interface.
Yet our industry must evolve. Rural healthcare faces unprecedented challenges: clinician shortages, specialty access gaps, financial pressures, and geographic barriers that won’t solve themselves. The digital health innovations funded through RHTP programs genuinely can save lives and preserve rural healthcare access—if clinicians actually use them.
The Transformation Challenges
This creates an urgent challenge for RHTP recipients: how do you rapidly deploy transformative technology while respecting the legitimate concerns of highly-skilled professionals who hold patients’ lives and wellbeing in their hands?
The answer isn’t more funding, better technology, or vendor promises. It’s systematic change management that treats clinicians as the keystone of transformation — the single most critical element that determines whether your RHTP investment succeeds or fails.
The LEAD Framework: Turning Investment into Impact
After 15+ years implementing digital health programs across 100+ rural healthcare projects and spending 12 years studying physician culture at the Mayo Clinic, I’ve developed a proven methodology for transforming clinician skeptics into innovation champions.
The LEAD Framework addresses the unique psychology and professional concerns that drive healthcare provider behavior:
L – Leadership Alignment with Patient Care and Clinical Goals
Establish clear vision & unwavering commitment from the top
RHTP success requires more than executive approval — it demands visible, consistent leadership commitment. When medical directors personally champion digital health initiatives and administrative leaders consistently reinforce the strategic importance, clinicians understand this isn’t another “pilot program” that will disappear in six months.
But leadership alignment goes deeper than endorsement. Effective leaders articulate why digital health innovation matters to the organization’s mission, where it fits within the broader strategic vision, and how it supports quality, access, and equity goals.
They answer critical questions like “Why should our organization excel at virtual care?” and “What does our long-term digital health strategy look like?”
Without this mindset, clinician resistance merely becomes tolerated rather than addressed which leads to immediate failure once attention wanes.
Leaders must consistently communicate the strategic imperative while providing the resources and support necessary for success. When clinicians see sustained leadership commitment, not just a budget allocation or RHTP funding grab, they recognize this transformation is both serious and permanent.
E – Experience Design with Clinicians, for Clinicians
Create workflows that enhance, not burden, clinical practice
Most technology failures stem from poor workflow design, not poor technology. Before selecting any RHTP-funded solution, map out the complete clinician experience: How does this fit into existing processes? What administrative burden does it remove? How does it help them practice at the top of their license?
Effective experience design mirrors the structure clinicians already understand. Break digital health delivery into discrete, manageable workflows: scheduling, patient preparation, the clinical encounter itself, and post-visit follow-up. Just as support staff handle in-person patient rooming and technical setup, they should manage virtual “rooming” and technology troubleshooting.
The clinician’s role should remain laser-focused on clinical care, not technical problem-solving. When a rural physician conducts a virtual stroke consultation at 2 AM, they shouldn’t be wrestling with platform glitches or walking patients through login procedures. Design with clinicians as partners, not end-users. Involve them in technology selection decisions, as this isn’t an IT decision alone. Their workflow insights often reveal implementation challenges that vendors never mention.
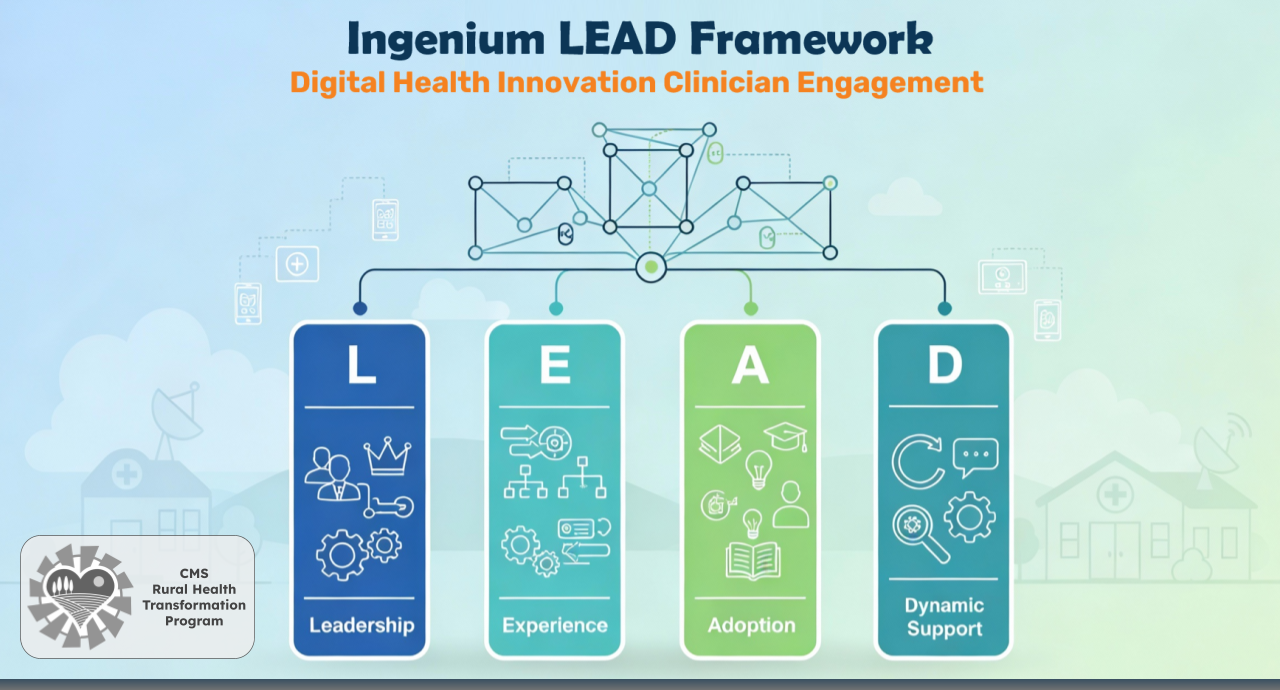
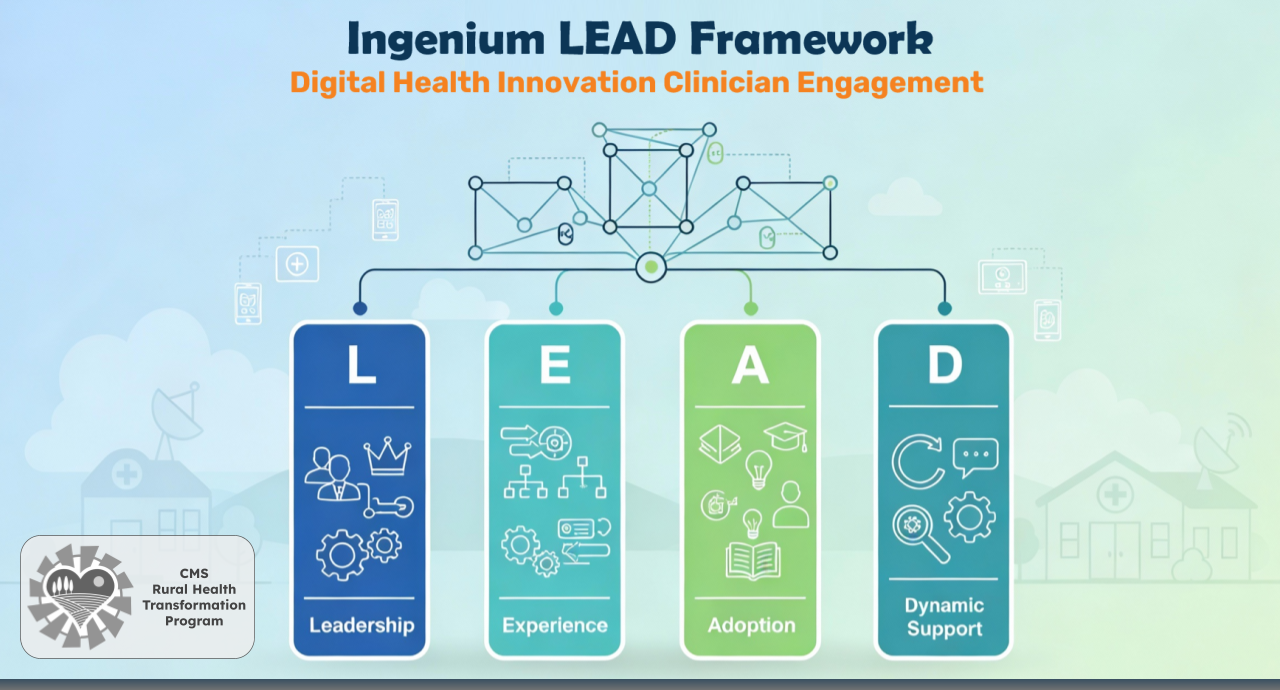
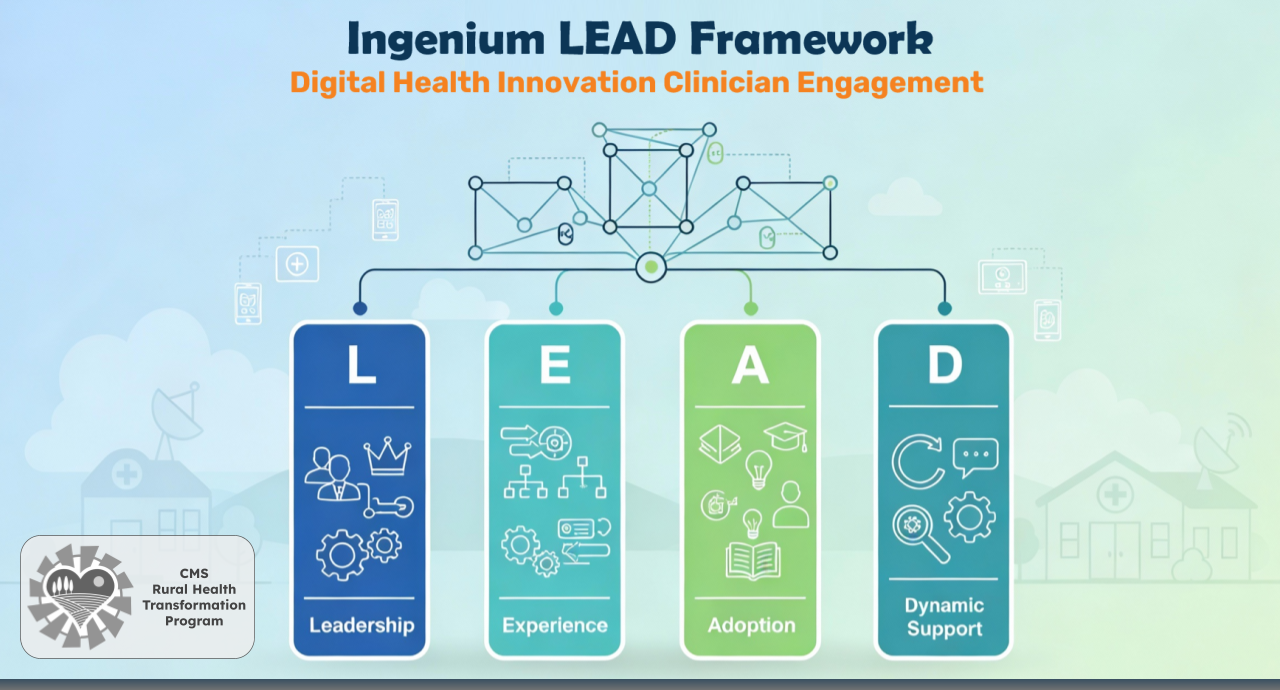
A – Adoption Training
Build competence before expecting confidence
Clinicians are highly skilled professionals who don’t want to appear incompetent. Traditional “feature training” fails because it focuses on button-clicking rather than clinical competence. Effective RHTP training programs simulate real patient scenarios, teach virtual communication skills, and build genuine proficiency, not just familiarity.
Successful training addresses the unique skill set digital health requires: mastering “webside manners”, conducting virtual physical examinations, diagnosing patients remotely without traditional assessment tools, and managing the unpredictability of technology-mediated care. Rather than generic platform tutorials, create specialty-specific scenarios that reflect real clinical situations your providers encounter.
A rural emergency physician needs different virtual consultation skills than a primary care provider managing diabetes. Training must be practical, hands-on, and directly applicable to their patient population. Confidence comes through competence, and competence develops through deliberate practice in realistic scenarios. Short, targeted sessions that build actual clinical skills will drive adoption far more effectively than lengthy feature demonstrations.
D – Dynamic Support
Provide continuous reinforcement and performance management
Even the most sophisticated RHTP technology becomes shelf-ware without ongoing support systems. Implement performance dashboards that track meaningful indicators: visit volume, patient satisfaction scores, clinician experience ratings, and clinical outcomes. Celebrate early adopters while providing additional support for those struggling with adoption.
Through active performance management create just-in-time coaching opportunities and regular feedback loops that help clinicians continuously refine their digital health capabilities — and vice versa. This isn’t one-and-done training, it’s ongoing professional development. Provide refresher sessions, address emerging concerns, and share best practices across your clinical teams.
Most importantly, listen actively to clinician suggestions and frontline insights. The physicians using your RHTP solutions daily often identify workflow improvements, technical enhancements, and process refinements that vendors and administrators miss. Create formal channels for collecting this feedback and demonstrate responsiveness by implementing viable suggestions. When clinicians see their input driving system improvements, they become partners in optimization rather than passive users.
Support systems should reinforce positive behaviors while removing barriers and obstacles as they become known. When clinicians know they have reliable, ongoing support rather than being abandoned after initial training, they’re more willing to embrace new approaches. Track what’s working, identify what isn’t, and adjust your approach accordingly. Dynamic support turns initial adoption into sustained transformation.
The 90/10 Rule for RHTP Success
Here’s what 15 years of rural health transformation has taught me: technology represents only 10% of RHTP success. Systematic implementation drives the other 90%.
The rural health providers and state teams that spend months evaluating vendor features while giving relatively minimal attention to change management have it backwards. The most important procurement question isn’t “What can this technology do?” but “How will we get our clinicians to embrace this technology?”
Making RHTP Investment Count
As it stands right now, your state’s RHTP funding represents a once-in-a-generation opportunity to truly transform rural healthcare delivery. But transformation requires more than buying better technology — it requires leading clinicians through change in ways that honor their professional concerns while building their confidence with new tools.
The LEAD Framework provides that roadmap. When rural health leaders invest as much energy in clinician engagement as they do in vendor selection, $50 billion becomes more than funding — it becomes genuine investment into lasting transformation.
Are you leading an RHTP implementation in your organization or state? The clinicians who will determine whether patients benefit from your investment are your most important stakeholders — and your greatest transformation opportunity.
To explore how the LEAD Framework can accelerate your organization’s RHTP success, schedule a strategic conversation.








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.








