In the mid 2000s I designed and built a highly energy-efficient home in Minnesota that had no furnace and was off-the-grid, off-the well. The house’s two sole sources of heat were a passive solar design (soaking up that sunshine and storing it in the slate tile floor) and a masonry stove.



The masonry stove, built by a British stone mason who lived in the area, provides over 2,000 lbs. of stone mass that, once heated up by a fire, will keep the house warm for hours, similar to a European tile stove.
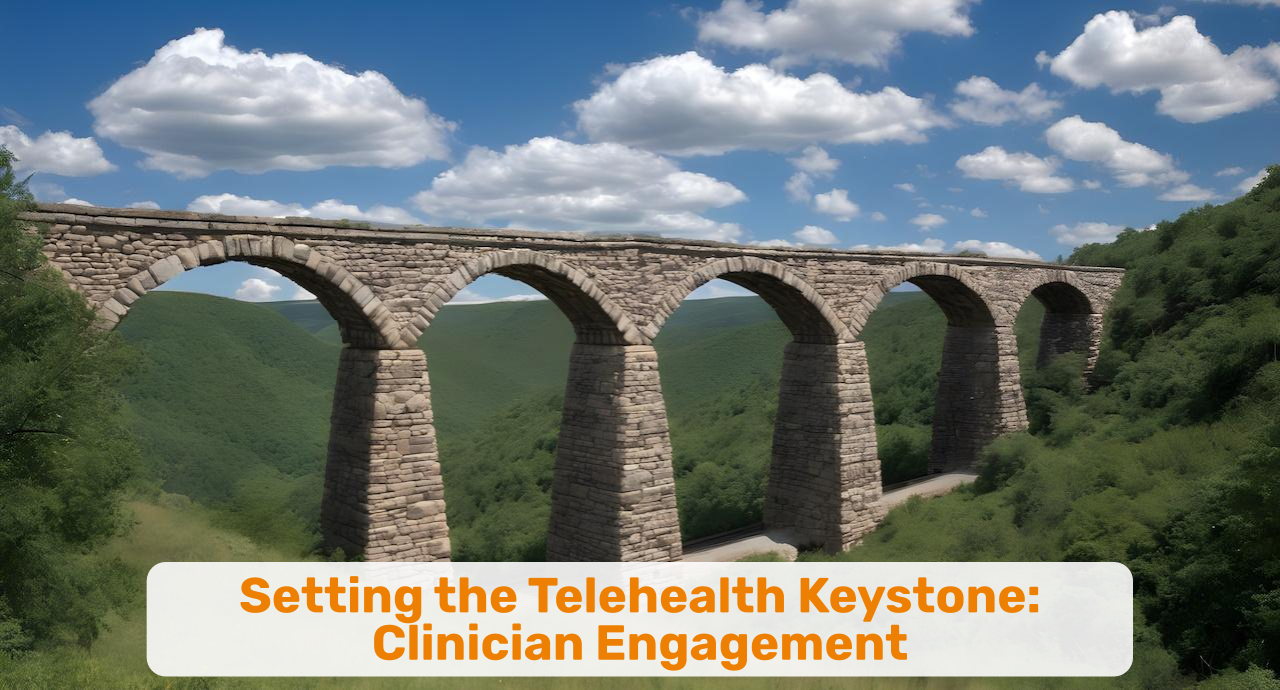
Built into the masterful design were two arches to match the arched doors of the firebox and of the baking oven. The highlighted stones in the center are the “keystone” that hold the arch together without much support — as seen in ancient arched stone bridges.
The keystone is the single most critical element in the arch – as all the pressure from both sides rests on the keystone that provides the strength and structure to hold the arch together.
In my over 15 years of implementing telehealth programs at dozens of organizations across numerous use cases, one element stands out as the singular most important success factor: the clinicians’ acceptance of telehealth as a feasible care delivery modality. This is telehealth’s keystone.
Clinician Engagement = Patient Engagement
Ultimately healthcare’s goal is to heal patients, to enable them a life mostly free of sickness. With many chronic diseases being exacerbated by lifestyle choices that even medications or other interventions can only cure partially, it has become imperative to involve patients in their care, to engage them, or even to “activate” them to take an active role in their personal journey to wellness.
But that can only happen when the clinicians providing care are engaged in their job — and most of them are.
At least when it comes to in-person care.
But once you switch to “virtual care” modalities, many clinicians, still, seem to be less engaged, less at ease. A bit like a fish out of water, out of their element, outside their comfort zone.
Yet on the other hand thousands of clinicians are delivering effective care every single day. In the classical healthcare environment those using telehealth are mostly behavioral health providers. But primary care and specialty care are provided on a daily basis by hordes of telehealth-only clinicians employed by the likes of Teladoc, AmWell, Amazon Clinic, etc.
So what is keeping video visit adoption rates in the single digit percentage of overall visits, when patients interest and desire for convenient virtual access to care is north of 70, 80% in survey after survey?
Clinician Engagement — a declared interest in and support of delivering care in a hybrid environment that uses both in-person and virtual care delivery.
From my first-hand observation, many clinicians are — consciously or unconsciously — hesitant to fully embrace virtual care as a viable care delivery alternative to in-person care.
Most of the time their reticence is veiled, hiding behind more “red herring”-like reasons such as “lower reimbursement” (not true in most cases and a video visit still bills higher than “no visit”) and the notion that “my patients are not interested” (which becomes a self-fulfilling prophecy when you never offer telehealth to your patients or try to talk them out of it).
Over the years through my direct work with clinicians I have contributed to the “conversion” of dozens of clinicians. From my perspective, it was merely a lack of training tailored to the learning style and mindset of clinicians.
Nobody likes to “look foolish” or make mistakes — and telehealth, when the processes and the technology are not properly deployed, is full of booby traps and sand bunkers that can easily trip up even the most experienced clinician.
A Guide to Chiseling and Setting the perfect Keystone of Extraordinary Virtual Care Delivery
Over the next weeks, I’ll be revisiting some of the concepts I’ve written about before, that will enable you and your organization to engage more clinicians in accepting and actively employing virtual care modalities to care for their patients.





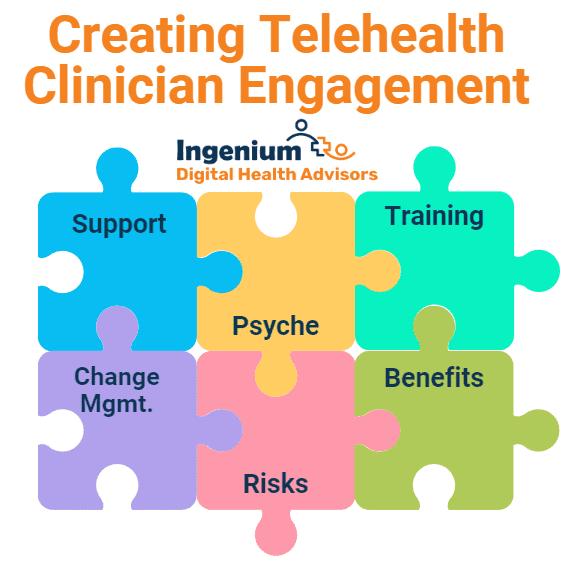
I’ll dive deeper into the psyche of a clinician’s mindset that makes them hesitant to fully embrace telehealth, along with a proven change management approach to lead your clinicians through this transition.
I’ll cover the various training and education offerings that you should provide for your clinicians that build confidence and trust into this different, but highly effective care modality.
I’ll describe the support system that any organization that is doing telehealth should have in place, going well beyond tech support.
I’ll also explore the detrimental effects that are stemming from ignoring this lack of telehealth adoption in your clinic.
And I’ll balance that out with a focus on Telehealth’s benefits for clinicians, including improving recruitment, increasing retention, raising overall satisfaction, combating burnout, and others.
Telehealth is here to stay – it’s no longer an option that can be ignored or hoped for to go away. The next set of articles will help you to get there more easily.
This spring I’ll be attending, moderating, and presenting at 6 conferences (MATRC, NRTRC, ATA, gpTRAC, NACHC CHCO, CalTRC) in four states and online. Let me know if you’d like to meet up in person at one of these events.










To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.