The future is already here; it’s just not very evenly distributed. — William Gibson
In this final installment of the 3-part series on ending the confusion around the digital health terminology (the previous two parts focused on Telehealth and on Connected Health, we are completing the Digital Health taxonomy by adding the two missing domains of Health IT and Precision Medicine.
As I’ve mentioned before, it’s not important that you use these definitions or this taxonomy, but it is important that you clearly define what the terms you are using mean in your organization. Because using the terms inconsistently or without a commonly understood and agreed-on definition will lead to miscommunication which causes confusion leading to a resistance to change.
Without further “philosophical ado”, let me now describe the domains of Health IT and Precision Medicine — that together with Connected Health form the three main branches of the Digital Health Taxonomy.
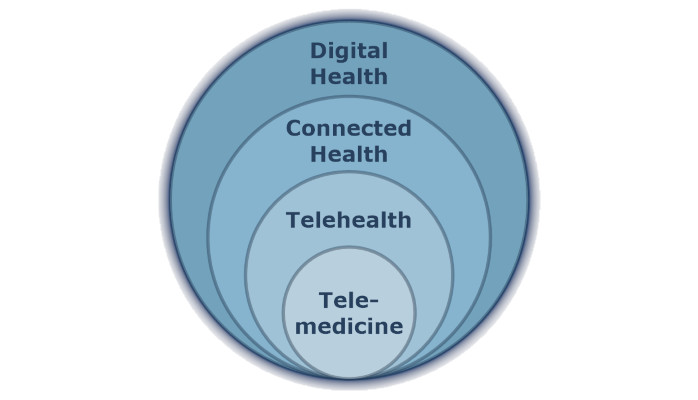
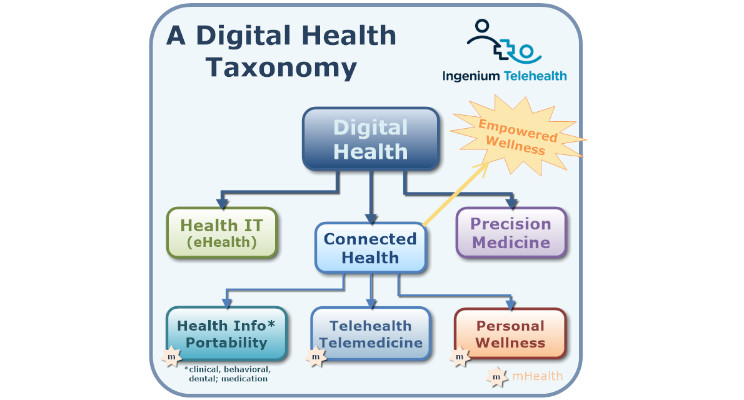
Digital Health
The topmost layer of the Digital Health Taxonomy combines three very different areas in medicine: Connected Health, Precision Medicine, and Health IT.
Whereas Connected Health concerns the delivery of care, Precision Medicine enables care that is precise and personalized to the unique needs of a single patient or a group of patients with similar needs. And Health IT provides the underlying, omnipresent set of technologies that actually make healthcare work.
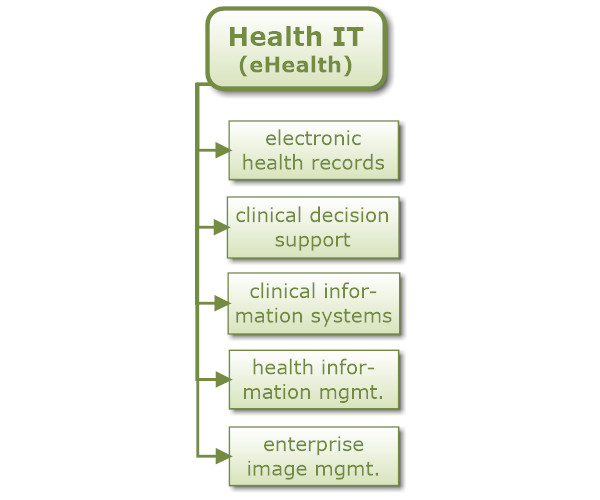
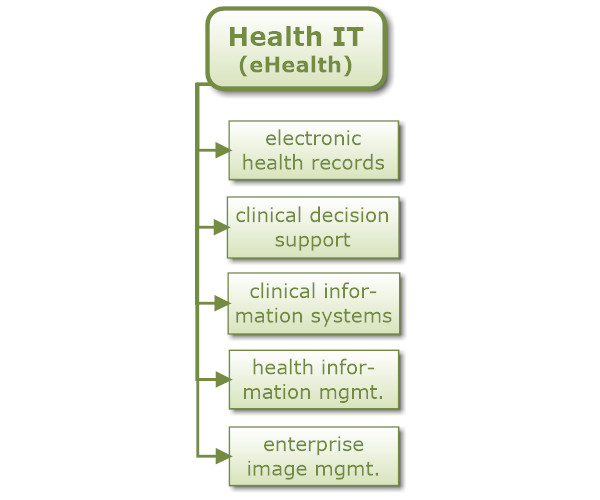
Health IT and eHealth
Health IT thus combines all the various technologies that health care needs these days to deliver care. While one could argue that Health IT encompasses any healthcare technology (including those used in the other areas of the taxonomy), I prefer to use the term in the context of supporting the ongoing operations to deliver care, including electronic health records, clinical decision support, clinical information systems, health information management, enterprise image management, etc.
Another often-used term is eHealth, which I consider to be synonymous to Health IT. With the ‘e’ standing for ‘electronic’, eHealth simply means electronic technology used in healthcare. Many of the technologies included in Health IT were introduced in the 1990s and early 2000s as “eHealth” projects. Since quite a few of those eHealth projects failed to deliver on their promises in the short term (mostly owing to poorly understood user requirements), the term eHealth for many people, including myself, still holds a negative ring to it. Though one could argue that eHealth is the same as Digital Health, I prefer to stay away from using the term eHealth altogether and have settled on using Health IT and Digital Health instead.
Precision Medicine
The final and newest branch in the Digital Health Taxonomy is the new, exciting field of Precision Medicine, which is healthcare tailored to a patient’s unique specific biology.
Too much of healthcare is applied with a broad stroke: mammograms for every woman above 40, prostate exams for every man above 50, statins for everyone with high cholesterol, and beta-blockers for all people with cardiac arrhythmias. Consider this example: if a drug reduces the mortality rate from 8% to 4%, that’s a 50% reduction of mortality. But it also means that the drug didn’t do anything for the other 96%.
That’s not very precise, but wasteful and, as we all know, very costly.
Precision Medicine is largely enabled by the advances in DNA sequencing, yet still kept from its full potential by the limitations of such sequencing. Over the past decades, the human genome project and the increasing affordability of DNA sequencing (from $100M in 2001 to about $1,000 in 2016) have significantly contributed to the progress in the field of precision medicine.
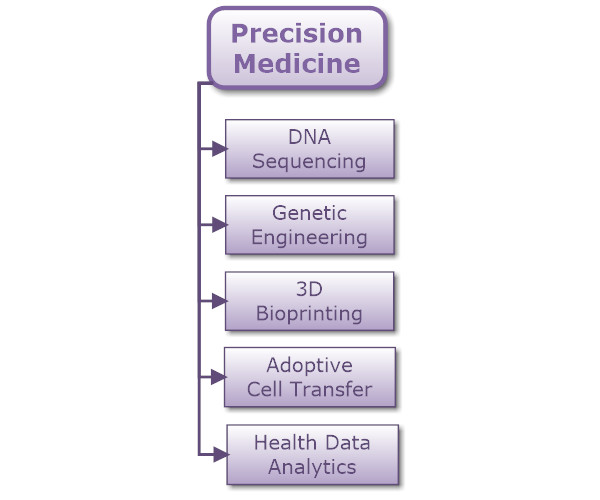
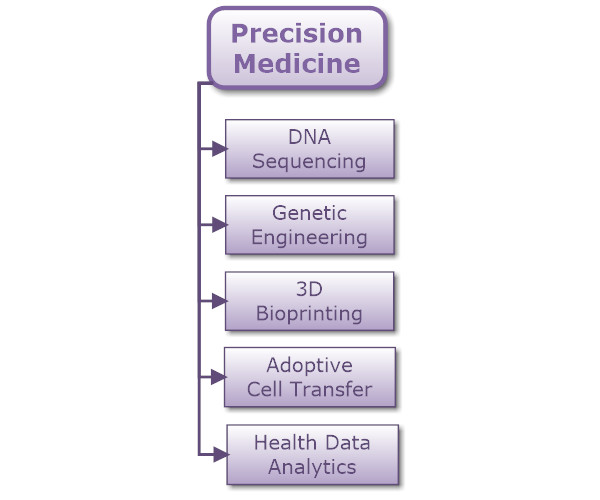
Precision Medicine encompasses many different technologies. For illustrative purposes I’ve included only a handful in the taxonomy:
DNA Sequencing enables the analysis of the human genome to identify specific markers that can indicate a proclivity for a particular disease or an incompatibility with certain drugs.
Genetic Engineering is used to produce improved or novel organisms, e.g., in gene therapy where defective genes are replaced with effective ones.
3D Bioprinting allows the fabrication of custom tissues or organs by stacking layers and layers of living cells. While still in its infancy, and currently mostly used for drug research, bioprinting holds great promise for the custom creation of organs, bones, or other tissue uniquely fitted for a patient.
Adoptive Cell Transfer (ACT) is the transfer of cells originating either from the patient or from another person and thus highly customized to the patient’s unique condition. A rapidly growing field within ACT is the transfer of a patient’s genetically modified cells (T cells) to strengthen a patient’s immune system to help combat cancer — a highly personalized and precise treatment, albeit still in the experimental stages.
Last but not least, Health Data Analytics is technology that differs quite a bit from the others mentioned here (think Sesame Street’s “one of these things is not like the other”), since it also finds its application in other areas, such as population health management, and as such could be considered a technology listed under Health IT. For Precision Medicine, Health Data Analytics makes de-identified data from healthcare operations available for research, cross-referenced with patients’ genetic profiles to find or to validate novel treatments. One recently announced collaboration between a university and a biopharmaceutical company, for example, will look at the correlation between “abnormal anatomical variations of brain structure to the underlying genetic markers of the diseases”.
The term’s predecessor — and a subset of Precision Medicine — is Personalized Medicine. As the name implies, Personalized Medicine focuses on the delivery of care tailored to the unique needs and circumstances of a particular, singular patient. Precision Medicine shares this ambition of individualized care, but aims to find solutions for a broader subset of the population that shares diseases and common traits. This branch of medicine is concerned with finding treatments that more precisely target the causes of certain disease, for example by applying knowledge about the effect of certain genes or a better understanding of the inner workings of cancer cells. With precision medicine a treatment can still apply to tens of thousands of patients, but care can be delivered more selectively, leading to better outcomes, fewer side effects, and ultimately reduced cost.
A Digital Health Taxonomy
Digital Health matters to us all of us since whether we like it or not, we all will come into contact with the healthcare system in one way or the other. And digital health solutions can help us patients and our providers a great deal to help us heal.
The field of Digital Health has shaped healthcare for the past 30 years and will continue to do so at an ever-increasing pace. Just 10 years ago digital health domains such as “Personal Wellness” or “Precision Medicine” didn’t even exist, except in the minds of a few researchers and visionary entrepreneurs.
And I’m sure that when I update this taxonomy in 2025, I’ll have to make room for another branch or two.



How have you defined the various terms in your organization? What does your taxonomy look like?
If you’d like a white paper and a slide deck with all diagrams to use in your organization or committee, please contact me and I’ll be happy to share it with you.








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.






Leave A Comment