“Real knowledge is to know the extent of one’s ignorance” – Confucius
If your organization is like many healthcare organizations, you are probably either contemplating to do something about telehealth, might have dipped your toe into telehealth (by using a telestroke service offering telehealth to your patients through a telehealth service provider such as amwell, Teladoc, MDLive, Doctor on Demand, etc.), or you may have even launched a few telehealth services on your own.
After all, how hard can it be, right? A camera and a computer or an iPad on a cart and you are ready to go. Telehealth is just like Telecommunications – install and configure a piece of technology and you’re good to go.
Well, only that it is not that simple.
Yes, adding an external telehealth service provider is easy to do, since (except for marketing the new service on your website) the new service in most cases does not really integrate with the way you currently deliver healthcare. Adding telestroke in the ER will probably also go over smoothly in most cases, because it is confined to one location and as a specialty, emergency physicians are highly open to change (but only if the telestroke provider provides reliable technology and trains the right people effectively).
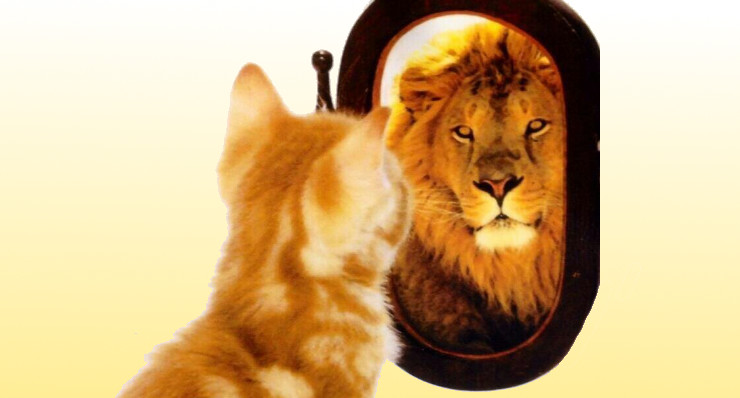
But if you or your organization’s leadership) thinks, that some technology and a little bit of training is all you need to know to successfully integrate telehealth into your practice, your clinic, your hospital, than you (or they) are wrong. In fact, you may have fallen fallen prey to the Dunning-Kruger effect.
The Dunning-Kruger effect lets people with limited experience in a subject matter mistakenly overestimate their ability. Have you ever seen an artist, an athlete, or a professional do something and said to yourself: I could do that! Then you might have succumbed to the same effect. If you think about it, it’s really what today’s reality TV shows are playing at: showing dancers, models, chefs (and bachelors) doing “their thing”, leaving you, the viewer, to believe “I could do better than that”. Only until you realize how much effort and training and knowledge really goes into a great performance (maybe with exception of the bachelors).
The same applies to telehealth. Historically, telehealth has been about the technology which up until recently was very expensive, hard to keep fine tuned so it would function reliably and definitely requiring “a man (or woman) behind the curtain” to make the magic of a video conference work. Not only was the technology very expensive, it was also quite hard to use and one had to tinker with the technology (and the training of the users) to get some adequate user experience out of it. Which is why many early telehealth projects were only staffed by “true believers”, the early adopters who were determined to make it work.
But telehealth, is really not about the technology. Telehealth is about “delivering care at a distance”. Which makes it a clinical service, not a technology. Allow me to repeat that, because it is easily overlooked: telehealth is a clinical service. Telehealth is a way by which healthcare is delivered and how medicine is practiced. As such, it must be driven by clinical goals as well as by organizational goals, but definitely not be driven by the technology.
Exacerbating the problem is also that – in compensation for the lack of capable resources – organizations often rely on technology vendors to help them implement the technology. But with only a few exceptions, vendors have very little understanding or appreciation how healthcare delivery really works and do not really understand how providers and allied health staff think. Actually many venture-funded telehealth companies are falling for their own Dunning-Kruger effect, thinking that since they’ve been “users” of the healthcare system, they know how it works and how they can fix it.
In my engagement with healthcare systems, I focus only 10-15% of my time on technology. The rest I spend on workflow redesign, on developing processes and policies, and, most of all, managing the organizational change by identifying and engaging clinical leaders and executives to lead the change.
Obviously the easy solution to compensate for the Dunning-Kruger effect is to hire telehealth implementation experts. But you can also try this “homemade” telehealth dream team recipe:



Take one business analyst (ideally a certified CBAB) experienced in clinical workflow design and Lean Six Sigma and pair them with one project manager (ideally a certified PMP) experienced in healthcare service projects (not just IT projects), add a part (¼ to ½) of an IT guy (or gal) to the mix and you have a pretty good team to at least get most telehealth services off the ground. To round out the team, you’ll also need a ⅙ of a finance person (to build your financial business cases) and about ⅓ of a marketing person (to advertise the new services internally and externally). Have the team be accountable to a C-suite executive (to lead the organizational change management) and you will successfully overcome the Dunning-Kruger effect.
Or you can outsource your telehealth launch and optimization to experts like us and get excellent results on the first go in days vs. weeks or months.
Has your organization fallen prey to the Dunning-Kruger effect? When did you realize it and how did you overcome it? Share your stories below.








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.








Leave A Comment