When I come across a new misconception, I’m always curious as to where this particular misconception originated. Oftentimes it is the result of “lazy thinking”, taking something you already know and applying it to the new circumstances without questioning it or without looking deeper.
This is the case with the second of the six misconceptions about telehealth which is the notion that a single technology solution (or at least one vendor’s solution) is all that is needed to implement telehealth.
This misconceptions stems from healthcare’s (and specifically health IT’s) exprience of using technology in healthcare. There is (or should be) one EMR. There is one PACS system. There is a standard for BI tools, for email, for time keeping, etc. Due to an uncontrolled wild growth in the 1990s of different technology solutions being used that essentially did the same thing, IT departments established strong policies to prevent such an explosion of solutions.
And rightfully so:
- multiple solutions take more time to support
- most solutions do not stand alone but eventually need integration with other applications,
- employee skills with one solution are not transferable
- negotiations for support (or innovative feature requests) from the vendor take more resources if you are using different solutions just to name a few.
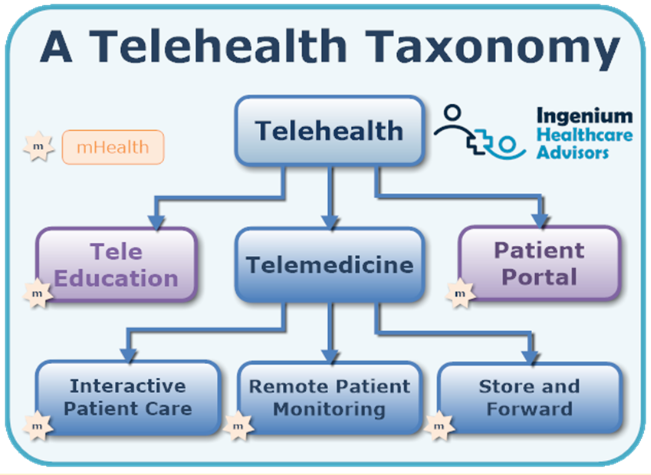
Telehealth, on the other hand, is very different. The definition of telehealth is “the delivery of care at a distance” and just as there are dozens of different ways to deliver care (just think of all the different specialties) there are at least a dozen different ways to practice telehealth. First off, in my definition of telehealth, it not only includes telemedicine “practicing medicine at a distance” but also tele-education and the patient portal – both requiring a different set of solutions to deliver those telehealth services.
Telemedicine further breaks down into interactive patient care, remote physiological (or patient) monitoring, and store & forward.
And within each subset of telemedicine, there are numerous solutions, especialy within the category that most people think off when they think of “telehealth”: live video visits with a physician, where in my assessment at least half a dozen different technologies are justified.
“You are Here”
First off, the location of the patient plays a very important role in the selection of the technology solution. If the patient is in a healthcare environment (e.g., a rural clinic, a skilled nursing facility, an emergency room, etc.) the technology will look very different than if the patient is at home or connecting from their place of work.
In a healthcare environment, healthcare staff has more control over the patient’s experience and it becomes an “internally used” solution, that is optimized for the mindset and workflow of the medical staff vs. that of the patient’s. E.g, for specialty visits in a rural clinic environment I often use a basic, secure video chat solution that would not be optimal for patients accessing it directly (as it would require an install and configuration and a slightly awkward way of connecting with the physician).
A direct-to-patient solution, however, needs to offer a smooth, configuration-less, one-click experience that works on any consumer-grade device such as a smartphone, tablet, laptop, or desktop.
“Timing is Everything”
The next consideration is the timing of the telehealth visit. Is it going to be pre-scheduled, or is it ad hoc, i.e., allowing patients to spontaneously request their visits? Support for consumer-facing ad hoc visits requires a set of sophisticated solutions that include the management of request queues, allocating available physicians to requesting patients, support for electronic handoffs from triage to specialists, etc. – just to name a few.
“To Exam or not Exam, that is the question”
A third dimension that justifies the use of different technologies for different types of telehealth visits is whether the telehealth visit will include the use of exam tools – whether that is a pan-tilt-zoom camera used to precisely assess the patient’s facial drooping in telestroke, exam cameras such as otoscopes, dermascopes, or telescopes (just kidding ;-), or digital stethoscopes to assess patients’ heart and lung sounds. Contrast that with consult-only scenarios such as follow-up visits to review the patient’s test results or televisits in behavioral health.
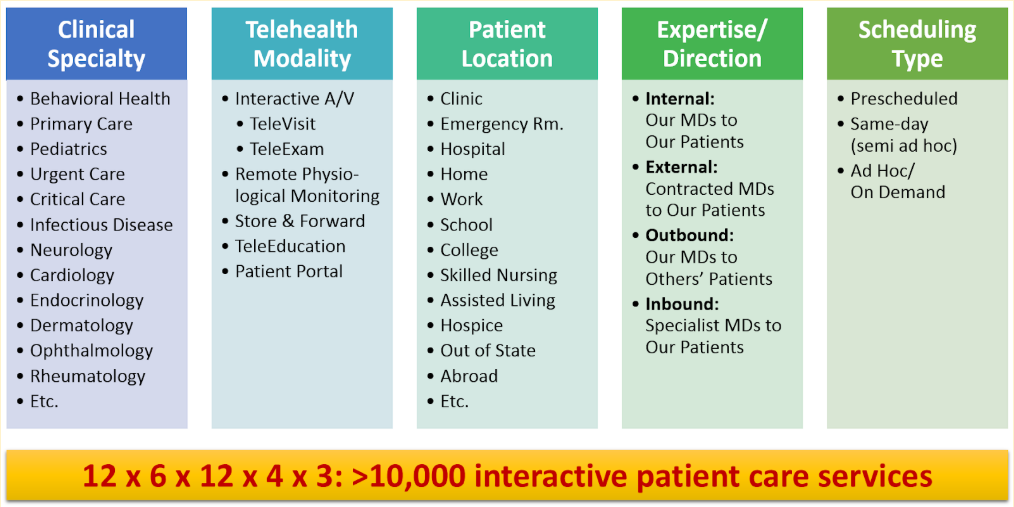
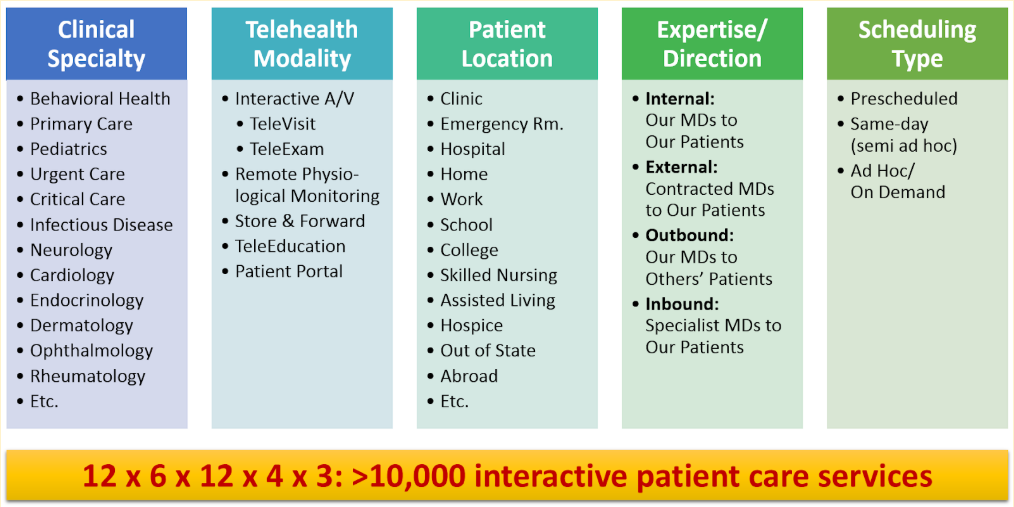
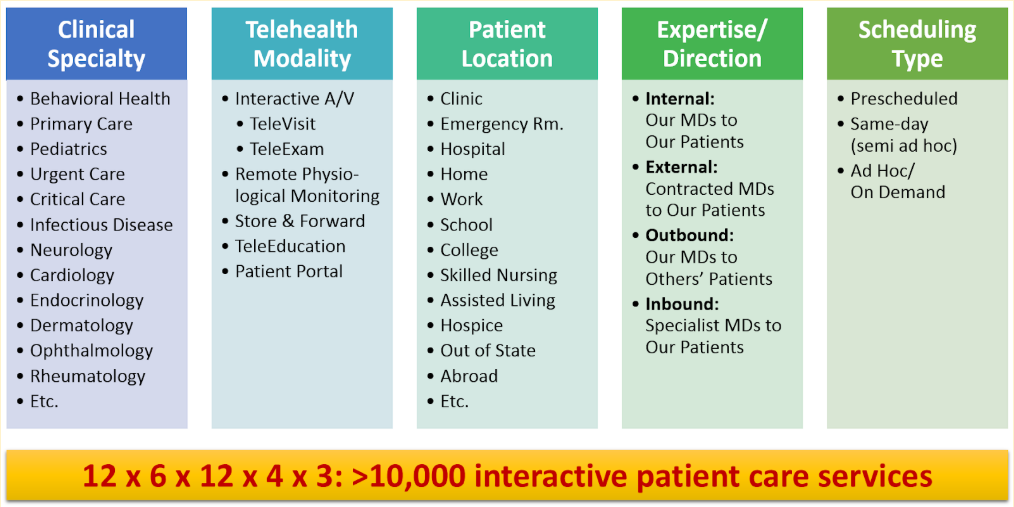
From this exploration of the most common scenarios just in “interactive patient care” the need for allowing and supporting different technologies to practice telehealth is pretty obvious. And even for seemingly similar use cases (e.g., prescheduled behavioral health visits and prescheduled primary care follow-up visits) different technologies may be justified, to create the optimal workflow for a great experience for both, providers and patients.
Not without precedent in healthcare
Historically, different healthcare services, even in common lines such as outpatient services or surgery, require different approaches. Different surgical specialties need different surgical tools – orthopedists may use a bone saw, but vascular surgeons may not. Cardiologists need EKS, but Podiatrists may typical have no use for them.
The same it is with telehealth – the tool, the technology should fit the task on hand.
The tail should not wag the dog.
And one technology cannot support all types of use cases.








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.









Leave A Comment