“Real knowledge is to know the extent of one’s ignorance” – Confucius
The Covid-19 health crisis catapulted everyone into the world of telehealth — and seemingly overnight, thousands of healthcare administrators became telehealth experts. Along with tens of thousands of clinicians whose subpar experience with telehealth became a self-fulfilling prophecy: “See, I knew that telehealth does not compare to in-person care.”
Similarly patients either fell completely in love with the idea of never ever having to set foot into a clinical waiting room or they had a dismal experience turning them off the idea of telehealth.
In 2023, three years after the stay-at-home mandate, most, if not all healthcare delivery organizations are still doing some form of telehealth. Though its low-percentage use is still far off from what’s clinically feasible and patient-desirable. And in that gap lies an unfulfilled potential, desired by modern healthcare consumers, that outside forces such as Amazon Care, Walmart Health, and many others are aiming to serve with a “virtual first” approach to healthcare — which, by the way, will inevitably be the norm by the end of the decade.
The question that healthcare leaders and clinicians have to ask themselves is: Are we delivering care at a distance in the best possible way, creating the best possible experience for providers and patients alike, achieving the best possible health outcomes?
Or are they satisfied with an “as good as it gets” approach that barely evolved from the haphazard “here’s a webcam and a video chat license” approach in March 2020?
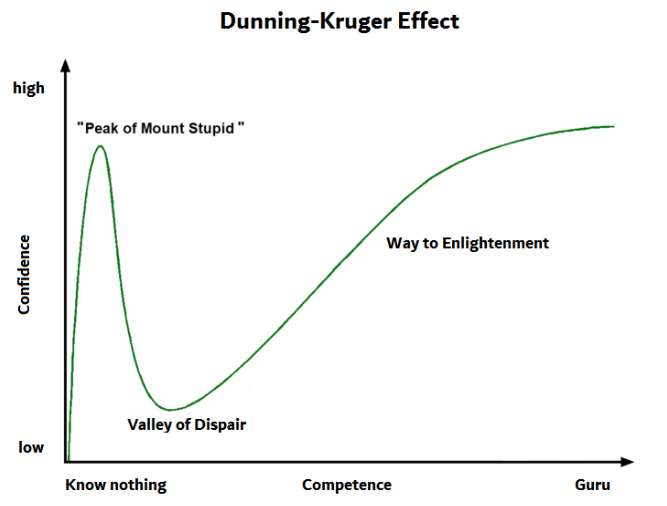
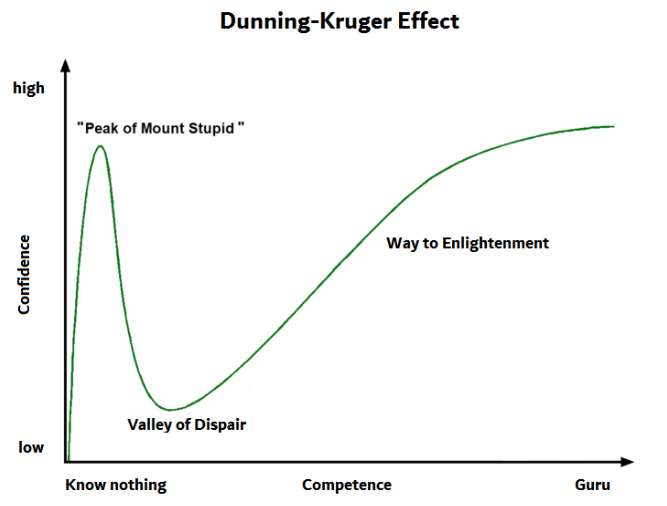
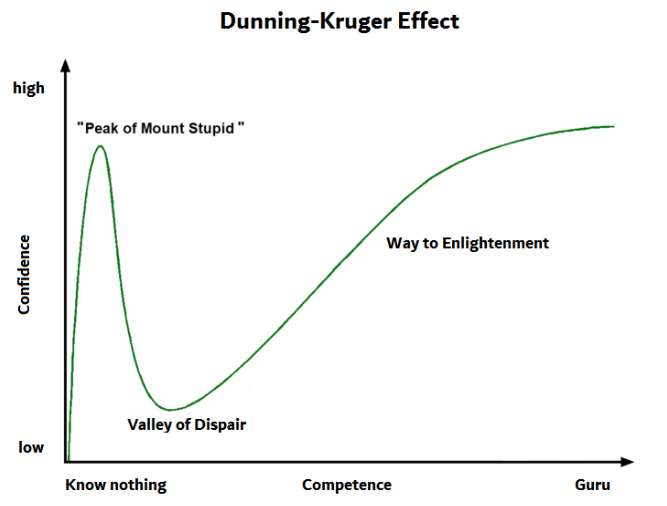
The Dunning Kruger Effect
The Dunning-Kruger effect is a cognitive bias that refers to the tendency for people to overestimate their knowledge of a new domain that they just started learning about. It’s confidence without the experience (a.k.a., arrogance).
It describes how healthcare professionals who are new to telehealth have vast blind spots, where they don’t even know what they don’t know. They are blind to the multiple facets and nuances of telehealth, to its many simple but not easy or simplistic techniques that increase telehealth’s efficacy.
A novel chess player, having learned and mastered the basic rules, vastly underestimates the complexities of the game. A rookie golfer quickly realizes that hitting the golf ball is the easy part.
In March 2023 the long-running flagship telehealth practitioner event, the MATRC Summit, organized annually by the Mid-Atlantic Telehealth Resource Center, noted a first time drop in attendance by as much as 30%. And it was definitely not for a lack of high-caliber speakers, pragmatic workshops, and a great location (plus the ability to attend virtually!).
Similarly, though presumably for other reasons, the 25+ year-old annual event of the American Telemedicine Association (ATA) also has dropped precipitously from the 6,000+ attendees from just 8, 9 years ago (yet the attendance of HLTH in November exceeded 10,000).
I think one of the key contributing factors is an endemic affliction with the Dunning-Kruger effect. Even 20+ years after the pivotal “Crossing the Quality Chasm” report, healthcare still does not have a widespread culture of relentless continuous improvement in all areas of care delivery and few leaders pay attention to the performance of their telehealth services.
Are you a Telehealth Rookie or Telehealth Expert?
The following set of questions is based on my 20 years in telehealth and 15 years in implementing telehealth services — most of which I actually discovered (and developed) in the last 5 years, showing how ignorant I, too, was in the beginning.
- Do you have a standard training program for clinicians to master virtual visits? Can you list the 7+ key elements of excellent “webside” manners?
- Do you have a standard training program for clinicians to conduct efficacious virtual exams without exam tools? Can your clinicians confidently conduct and document a virtual exam that covers 90%+ of an in-person exam?
- Have you defined and documented all of your telehealth workflows? Have your front office/call center staff, nurses, clinicians, and medical billers been trained? Do you differentiate between happy day scenarios and alternate scenarios? Can you name the 7+ telehealth workflows (or at least 5!) that your organization should have defined?
- Do you have a designated telehealth coordinator or director of telehealth? Can you list 5+ justifications for a telehealth coordinator position and list their 7+ typical responsibilities?
- Have you established a cross-functional, multi-disciplinary, clinician-led governance team, charged with ensuring the success of your telehealth services and to oversee its growth?
- Do you have a telehealth strategy and sustainability plan that prioritizes the use of telehealth to achieve your organization’s overall strategic goals?
- What are your 7+ focus areas for the optimization of your telehealth program?
- Do you have a telehealth marketing strategy?
- Do your patients, for the majority of visits, have an easy choice between in person and telehealth visits?
- Do you consider Remote Physiological Monitoring, Digital Therapeutics, and the Patient Portal experience part of your overall Telehealth (or Connected Care/Connected Health) scope?
- Are you periodically assessing your telehealth services’ performance from at latest three different angles? What are your 3+ key performance indicators for telehealth success? Who is collecting & analyzing and who is reviewing the data and acting on it?
My guess is that many organizations cannot equivocally say “yes” to these 20+ questions. And those with the largest blind spots actually will question the relevance of most of these questions: “Why would I want to do that?”
After 15 years in the field, it’s no coincidence that this is my 190th article that I have written on telehealth and digital health with no shortage of topics in sight regarding the various nuances and best practices. And while I do repeat some topics (e.g., this is a rewrite of a 2017 article), I have easily covered over 120 different topics.
There is much to learn and only increased knowledge will move one through the “Valley of Despair” and on the “Way to Enlightenment”.
The Dunning-Kruger Effect in Action
Here is some more food for thought regarding the Dunning-Kruger’s effect on the various players:
The Dunning-Kruger Effect in Clinicians
- Underestimate how much diagnostic and treatment care can actually be provided virtually.
- May be oblivious to different technical capabilities that would make their and their patients experience better, improve patient engagement, and drive better outcomes
- May apply their in-person training without modification to the virtual environment, without consideration of the pitfalls.
The Dunning-Kruger Effect in Healthcare Leaders
- Are simply satisfied with the fact that telehealth is occurring without any insights as to the quality of telehealth, the volume, or the growth potential.
- Listen to the equally affected clinicians who still think that telehealth is bad medicine, because they don’t know how good it could be.
- Think all is well as is and do not realize the potential of telehealth to add to the bottom line by combating burnout, reducing the nursing shortage, or better serving a rural population.
The Dunning-Kruger Effect in Patients
- May overestimate what conditions can be safely and accurately diagnosed and treated remotely.
- May overvalue the clinician’s capability to treat them as good as in person (mainly due to the lack of proper training on the clinician’s part)
- May lack the awareness of the various disparate systems that share information about them and their medical conditions.
Overcoming the Dunning-Kruger Effect
The cost of the Dunning-Kruger effect can be staggering, once an organization understands what could be achieved if telehealth were to be used as efficiently and effectively as possible.
Since Modern Health Consumers may simply opt to seek healthcare elsewhere, where virtual care is well executed, it can take years before healthcare leaders notice a difference — and by then it may very well be too late and those patients and their associated revenue are “lost”.
But the key driver to do better in telehealth should not be fear. It should be an embrace of the exciting premise that most of today’s diagnostic care (which already relies heavily on lab and radiological tests and not on hands-on exams) can easily and effectively be delivered “at a distance”. It should be that telehealth can more easily enable care coordination, ensure continuity of care, and ultimately drive patient activation.








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.