The purpose of managing the performance of your telehealth services is to ensure that you are getting the most value out of your investment into launching, optimizing, growing, and expanding your various virtual care offerings, including video visits, tele exams, remote physiological monitoring, secure messaging, digital therapeutics, etc..
In the right hands, Telehealth is a Swiss Army Knife, a Magic Wand to achieve a healthcare care organization’s most critical strategic goals.
Telehealth can improve the quality of your care and care outcomes. Telehealth can open the door to a whole new world of services and a reimagined service experience. Telehealth can attract and retain talented people (clinicians, nurses, and other staff), while reducing burnout and attrition. Telehealth can improve finances through expanded markets, improved clinician productivity, and reduced penalties. Telehealth offers numerous opportunities for geographic, financial, and capacity growth. And Telehealth can help organizations to offer great value to the communities they serve.
Given the aggressive entrance of outside care providers (such as Amazon, CVS, Walmart), it is now crucial for every healthcare organization to invest in winning the race toward becoming the provider that offers the best digital experience, because that is what the ever increasing majority of modern healthcare consumers expect and what also can achieve better health outcomes.
But, in order to achieve all of those successes, the execution of telehealth services must be nearly flawless. Any tool, no matter how great or valuable, will provide the desired benefits only when it is consistently used correctly.
To simply deploy telehealth is by far not sufficient. Buying a piano does not make you a musician. Acquiring a wood lathe does not make you a carpenter. You must learn and practice how to use the tool appropriately. Follow the rules. Implement best practices. Learn the techniques. Follow the process.
In the world of telehealth that includes workflows, policies, operational support, technical support, training, marketing, technology, etc.
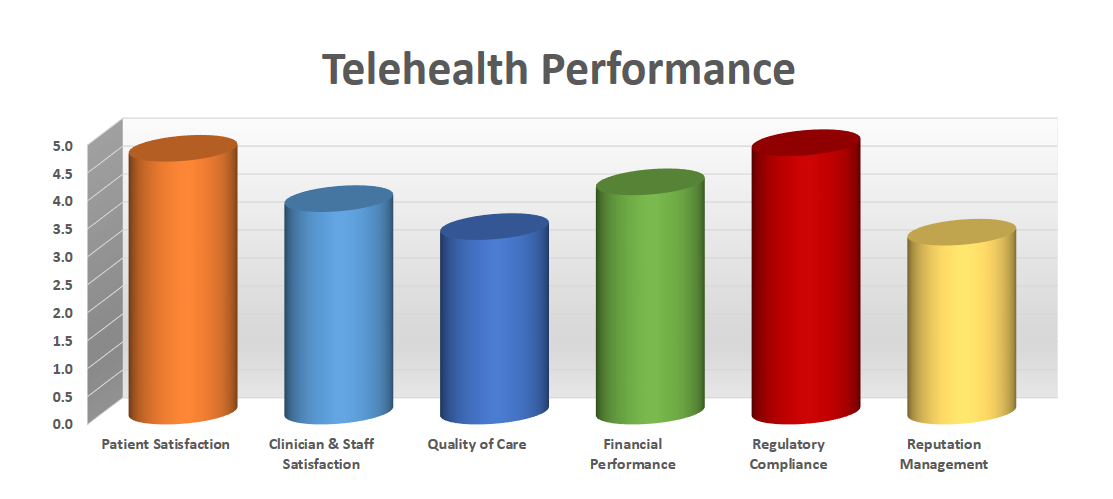
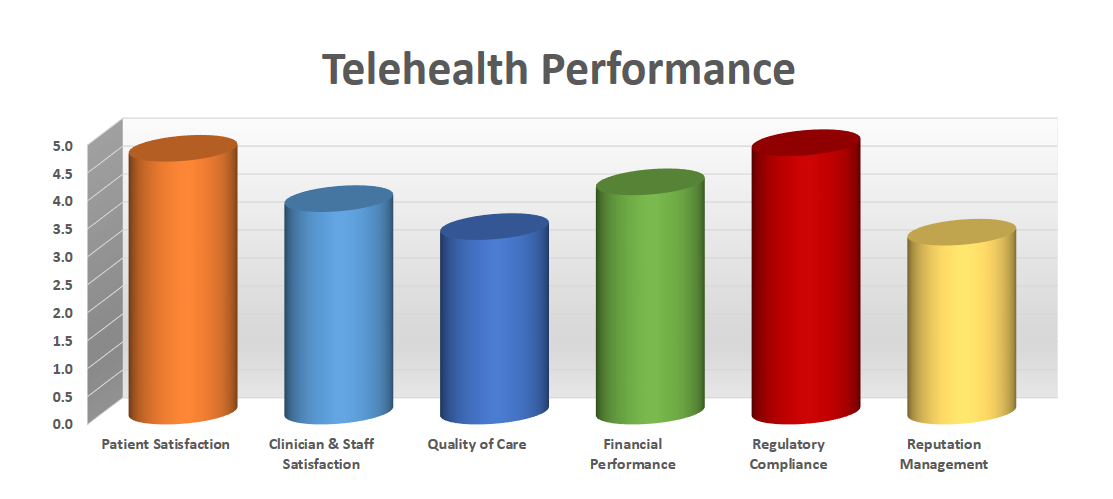
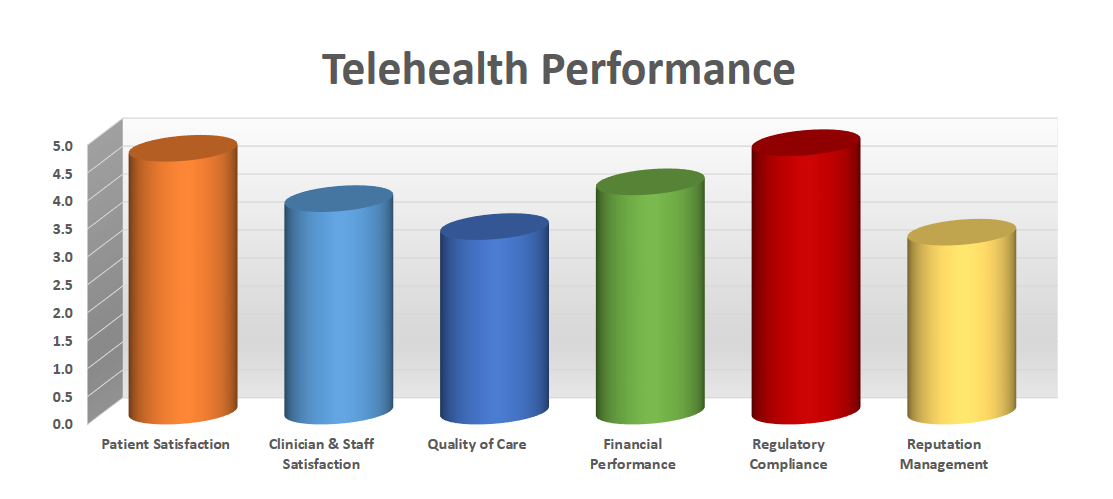
The Six Attributes of Telehealth Performance
To guide the management of telehealth performance, each telehealth program should have its own associated telehealth strategy that defines and ranks the organization’s strategic telehealth priorities.
Based on the maturity level of the organization’s telehealth program, the importance and rank order of the following attributes will vary.
Here are six attributes of telehealth performance:
- Patient Satisfaction
- Clinician & Staff Satisfaction
- Quality of Care
- Financial Performance
- Regulatory Compliance
- Reputation
Managing Patient Satisfaction is key when it comes to telehealth. The virtual nature of the service lends itself easily to comparison shopping because patients now can easily “vote with their mouse” vs. “voting with their feet”. Switching virtual providers is as easy as clicking on a link, and if the experience does not meet patients’ expectations.
Assessing and managing patients’ satisfaction should include an array of aspects from satisfaction with the technical aspects, a review of the clinician’s webside manners, to the coveted net promoter score. For inspiration on other elements, check out our Patient’s Bill of Telehealth Rights.
Managing Clinician & Staff Satisfaction is paramount to telehealth success. As is known from other service industries, a high customer satisfaction (i.e., patient satisfaction) cannot be provided by disgruntled employees.
In an ideal telehealth experience, the technology quickly fades into the background allowing the clinicians to do their core job of practicing medicine. To get to this point, however, training and coaching is needed, as well as a relentless optimization of the technology used. In an ideal telehealth experience every staff member understands their critical job to keep everyone satisfied and ultimately deliver to the patient an all-around great service experience.
Managing the Quality of Care can take on different forms, depending on the aspect of care quality that is important to the organization. It can include adherence to clinical care policies, continuity of care measures related to missed/canceled appointments, compliance with care plan instructions including medication management, etc. The clinicians’ adherence to established best practices applies to telehealth just as much as in the in-person care environment.
For value-based care programs, Quality of Care measures could also include control of key indicators (e.g., A1c values for diabetes management), compliance with vital sign parameters (e.g., blood pressure range for a remote physiological monitoring (RPM) program for hypertension management), or utilization of urgent care, emergency care or hospital services.
Managing the Financial Performance is also crucial, since health care is almost always under financial pressure and telehealth can greatly alleviate financial challenges, due to the geographically-independent nature of telehealth allowing to cast a wider net.
Measures in this domain could first of all include tracking the reimbursement for all telehealth visits, but can also look at indirect measures, such as the reduction in cancellations or no shows or meeting quality goals in the context of value-based arrangements.
Managing Regulatory Compliance is especially important during this time (the Spring of 2023) as the public health emergency is coming to an end and multiple regulations are about to change. Vigilance (and control measures) are needed to ensure that telehealth services are provided within the current regulations.
Finally managing the Reputation of Telehealth Services in the community, among patients, is key to growth and expansion. In the age of online reviews and social media, patients will quickly post flattering and not-so-flattering remarks about their experience, and it’s important to monitor and respond to those public comments.
One of the best marketing tools is word-of-mouth referrals by satisfied patients, so keeping a close eye on the aforementioned net promoter score (“How likely are you to recommend a telehealth visit to your friends and family?”) is key.
To Manage Means to Measure and Act
All of the six domains above could each yield a number of measures — specific data points that indicate performance. For more information, see my numerous articles on the various aspects of measures and key indicators.
What is key to remember is that to manage means to measure (and to act), as my colleague Kathy Letendre frequently points out. The process for managing performance is quite straightforward:
- Identify the key performance indicators (KPIs) that best represent performance
- Identify the data sources and define the process for proper data collection, analysis and presentation
- Establish desired targets or goals for those KPIs
- Collect, analyze and present the data to identify any gaps between the actual and the target
- Identify corrective actions to bring the performance of that metric in alignment with the desired performance
- Implement the corrective actions and repeat
Without the collection and analysis measures, you are flying in the dark and are merely assuming that everything is going well.
Only through continuous improvement of the performance of your telehealth services will you be able to reap the promised benefits of telehealth for your organization.
Do you want to launch or improve your own telehealth performance management program? Reach out to me for some guidance to get started.








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.








