The end of a year and beginning of a new year are popular times to make predictions about the future. So with Telehealth Tuesday’s edition #222, here are my three predictions for 2024:
A. Telehealth Is Enabling New Care Delivery Paradigms
As I reflect on the journeys we’ve traveled over the past year with our clients on the road to a better use of telehealth, I cannot help to detect quite a shift in the way that those informed leaders and capable staff are taking their use of telehealth to delivery their service. Here are just three examples of how these organizations used telehealth as a springboard:
- A behavioral health agency in a Washington State county larger than Delaware expanding their use of telehealth to bring fast access to TeleCrisis services in five EDs and TeleSUD services in multiple communities 30-60 min away from the main clinic.
- A rural federally qualified health center (FQHC) opening up a telehealth drop-in clinic in a community fire station.
A rural behavioral health agency — now equipped with a Digital Health Strategy that evolved from their Telehealth Strategy — launched a proof-of-concept to assess the integration of a digital health solution to increase clinician efficiency.





My prediction for 2024 is that we will see more healthcare leaders pushing for an expanded use of telehealth to reach new populations or serve their populations in a better way — beyond the mere “hybrid care” of in-person visits and to-home virtual visits.
B: Sustainable Use of RPM that Measurably Improves Outcomes
After the introduction of CCM and RPM reimbursement codes in 2019, Remote Physiological Monitoring services were all the rave all through 2022. Most of them were focused on creating new service revenue facilitated by hundreds of RPM startups that promised easy additional income, but failed to engage the patient or measurably impact outcomes. And many RPM-related initiatives were grants for RPM equipment that ultimately ended up on the shelf, because there was no expertise in successfully launching RPM services that would drive patient engagement and outcomes.



With an increase of chronic diseases predominantly caused and/or exacerbated by patient behavior (poor diet, poor exercise, poor sleep) it is increasingly becoming evident that our clinical care system must engage and activate patients to participate in their care.
RPM, when implemented properly, can teach patients more about the effects of their lifestyle (e.g., the effect of Chinese takeout on water retention and weight gain for CHF patients), therefore engage them in their journey to better health. In my non-clinical opinion, if physical care is also augmented with tele mental health care via video visits, we could see a dramatic improvement in health outcomes — with RPM being the catalyst of real-time feedback.
C: AI will have little to no impact on Telehealth
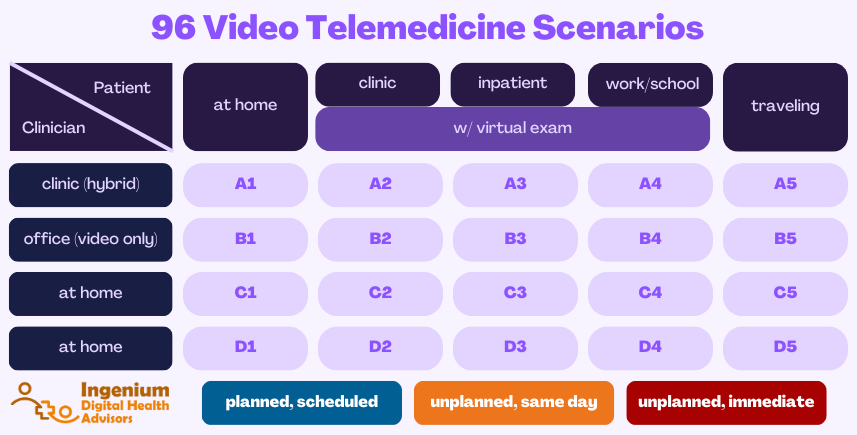
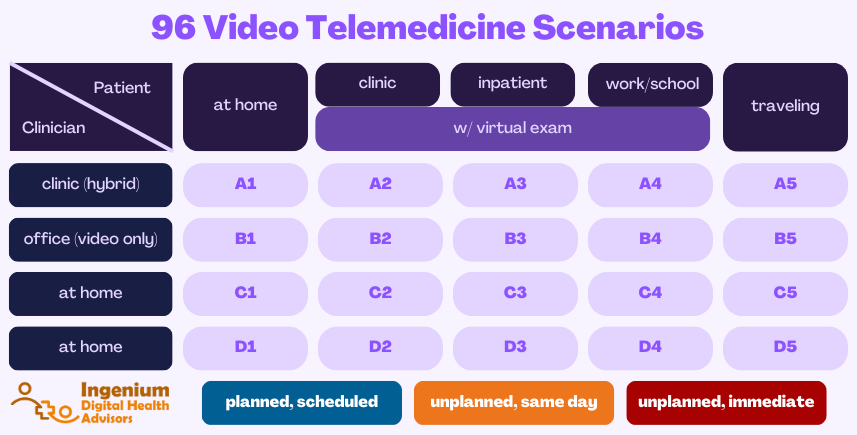
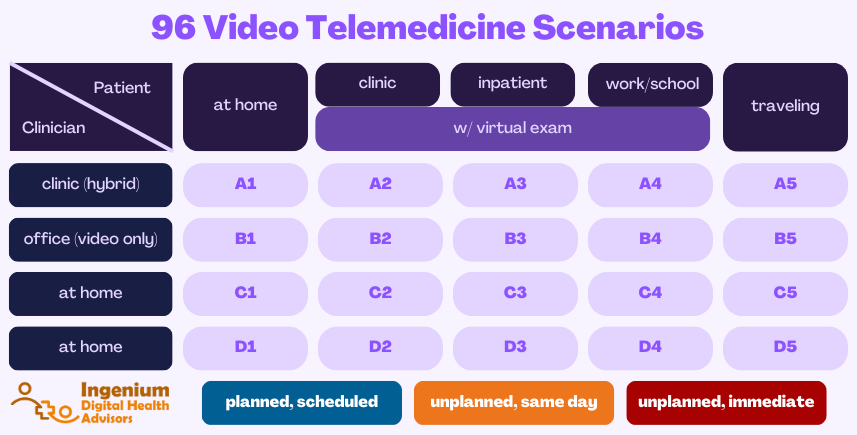
We define Telehealth as “Delivering Care at a Distance” and “Virtual Care” as “Providing Care at a Distance”. This encompasses video visits and RPM, but also the whole set of “patient portal functions” including appointment scheduling and asynchronous secure messaging.
And in this basic world of delivering care, Artificial Intelligence will not add much incremental value — yet. While AI currently is “all the buzz” — especially the ominous-feeling generative AI — too many healthcare organizations still have not even reached the “Strategic” telehealth maturity level, let alone the “Integrated” maturity level just below.
I.e., organizations have learned to crawl, stand, and walk – but are not quite ready in 2024 to run, let alone run “artificially enhanced”. While many Health IT leaders and nerdy clinician leaders will be attracted to the AI bells and whistles; and while many telehealth vendors will feel pressured to add “AI-enabled functionality” to their products — these feature sets will not create the hoped-for value, since clinicians are still struggling to use telehealth well, let alone take advantage of advanced functionality provide by AI.
There will be good, effective use of “Augmented Intelligence” (as I like to call it in healthcare, being less threatening to clinicians) in areas more related to digital health, e.g., diagnosis, care planning, and treatment titration. But the actual deliver will be devoid of any true AI (in 2014 one RPM vendor was touting ‘predictive analytics’ to detect trends – that which now would be called “AI”).



But AI does have good entertainment value as this limerick from my February 2023 article demonstrates:
So, what’s in Store for 2024?
More or less of what’s been before!
Maybe it’s my wishful thinking or my systems focus, but in 2024 I’d like to continue to see Telehealth be solidly cemented into the care delivery system to form a solid foundation for what’s to come with digital health (and AI).
The lessons learned from a proper rollout of telehealth about workflow design, change management, and data-driven improvement will serve organizations well as they prepare to reinvent not just care delivery, but care overall.
Let’s check back in January 2025 to see how I did.










To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.








