Many Telehealth Tuesday readers have in recent months pointed me towards ChatGPT (launched in November 2022) and invited me to assess its relationship with or value for modern medicine.
While this definitely is a great research route (or rabbit hole?) to follow, after finally signing up for my account, I first started playing a bit with the system.
Here are a few of the results and my commentary.
The Benefits of Telehealth
The first answer I was curious about was what the system thought were the benefits of telehealth. Here was the reply by the “Chat Generative Pre-trained Transformer”:
Telehealth provides several benefits, including:
- Convenience: Patients can receive healthcare services from the comfort of their own home or any location with an internet connection.
- Accessibility: Telehealth can improve access to healthcare for people in rural or remote areas who may have limited access to healthcare providers.
- Time-saving: Telehealth appointments can be scheduled more quickly and easily than in-person appointments, and they typically take less time.
- Cost-effectiveness: Telehealth can reduce the cost of healthcare by reducing the need for travel and in-person visits.
- Improved health outcomes: Telehealth can lead to improved health outcomes by providing patients with more frequent and convenient access to healthcare services.
- Increased efficiency: Telehealth can improve the efficiency of the healthcare system by reducing wait times, freeing up in-person appointment slots, and allowing healthcare providers to see more patients in a given day.
I have to say that after 20 years in telehealth, this is not only a pretty comprehensive list, but also some very good definitions behind it.
I was particularly intrigued by some factoids that are not generally known.
First off the fact that telehealth appointments “typically take less time” — mostly due to the individuals feeling less inclined with small talk — and also because patients did not have to “invest” an hour or more to make it to the appointment, thus they don’t feel they have to “get their money’s (or time’s) worth.
Secondly, I liked the notion of cost-effectiveness – from a systems / societal perspective and (for a refreshing change) not from the perspective of the providers or the payors. No: it’s the patients that save cost. How refreshing!
Though upon further examination, I have to point out that the lead-in “reduce the cost of healthcare” is a bit misleading, as the cost of healthcare does not typically include the mileage to and from. It’s rather the 5th point (better outcomes) that can reduce the cost of healthcare by increasing continuity of care, patient activation, and thus reducing high-cost service utilization, like an ER or even urgent care.
Finally, I’m fascinated by the last point: it’s a perspective that I’ve been trying to convey to providers and executives. There’s not much explanation given (and it almost sounds like it’s biased towards the merits of telehealth), but all the points raised can be accomplished, though it’s not an easy lift.
Health System Telehealth Readiness
Putting on my entrepreneurial consulting service definition mindset, I asked the AI for inspiration for our next blockbuster service: “How would you assess a health system’s telehealth readiness?”
Again, here is the comprehensive answer:
To assess a health system’s telehealth readiness, you can consider the following factors:
- Infrastructure: Availability of reliable and secure technology infrastructure, including high-speed internet, cloud-based solutions, and secure communication platforms for telehealth.
- Clinical Workflow: Integration of telehealth into the existing clinical workflow, including appointment scheduling, patient data management, and provider documentation.
- Provider Adoption: Assessment of provider comfort level and training needs in utilizing telehealth technology.
- Patient Acceptance: Understanding of patient preferences and behaviors in regards to telehealth, as well as ensuring patients have the necessary technology and equipment to participate in telehealth visits.
- Payment and Reimbursement: Review of telehealth payment and reimbursement policies, including private insurance, Medicare, and Medicaid, to ensure sustainability of telehealth services.
- Quality and Safety: Evaluation of telehealth quality and safety standards, including HIPAA compliance and patient privacy considerations.
- Data and Analytics: The ability to capture, analyze, and utilize telehealth data to continuously improve patient outcomes and satisfaction.
- Legal and Regulatory Compliance: Review of telehealth laws and regulations, including telemedicine licensure, informed consent, and malpractice liability.
By evaluating these factors, a health system can gain a comprehensive understanding of its telehealth readiness and identify areas for improvement.
Once again I was impressed by the breadth of the answer and the comprehensive 8-element framework that is proposed.
A few phrases stood out here as well.
One of our key hallmarks in optimizing telehealth is to ensure that providers feel comfortable offering telehealth. So needless to say I was impressed to find that notion of “provider comfort level” in the response.
Similarly impressive was the multi-point view of the patient’s experience – especially with a focus on “preferences and behaviors” that frankly I had not considered in this way. The second part of that answer, patients’ technical readiness, is something we address through Telehealth TechChecks and I was pleased to see that notion reflected, too.
Another thing that stood out is the emphasis in the 7th point on “continuous improvement” as well as the hint in number 5 to “ensure the [financial] sustainability”. That’s quite some more advanced thinking!
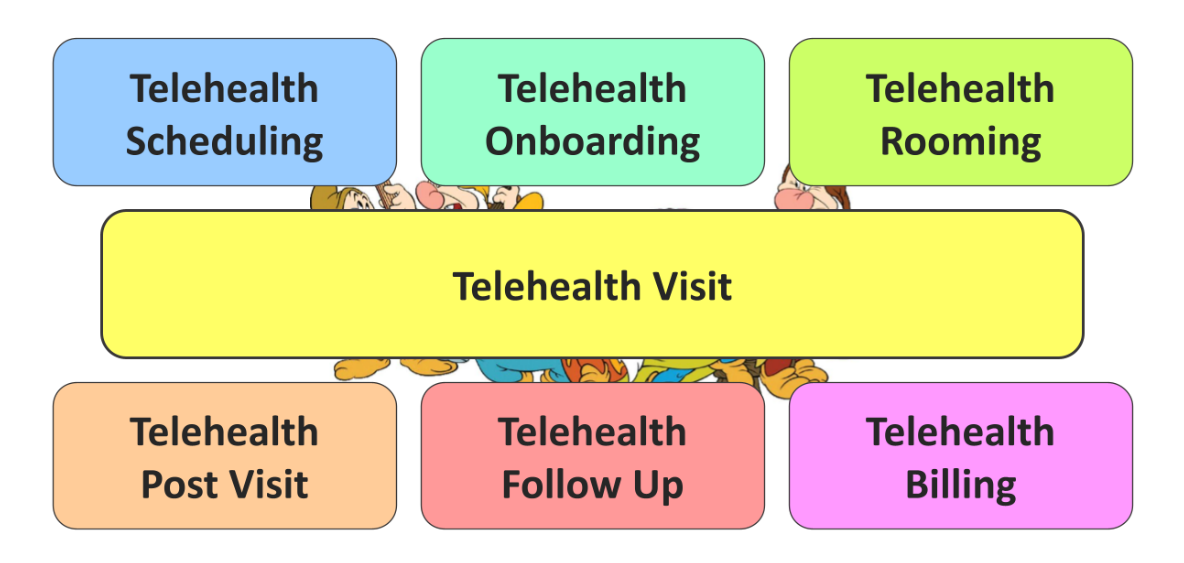
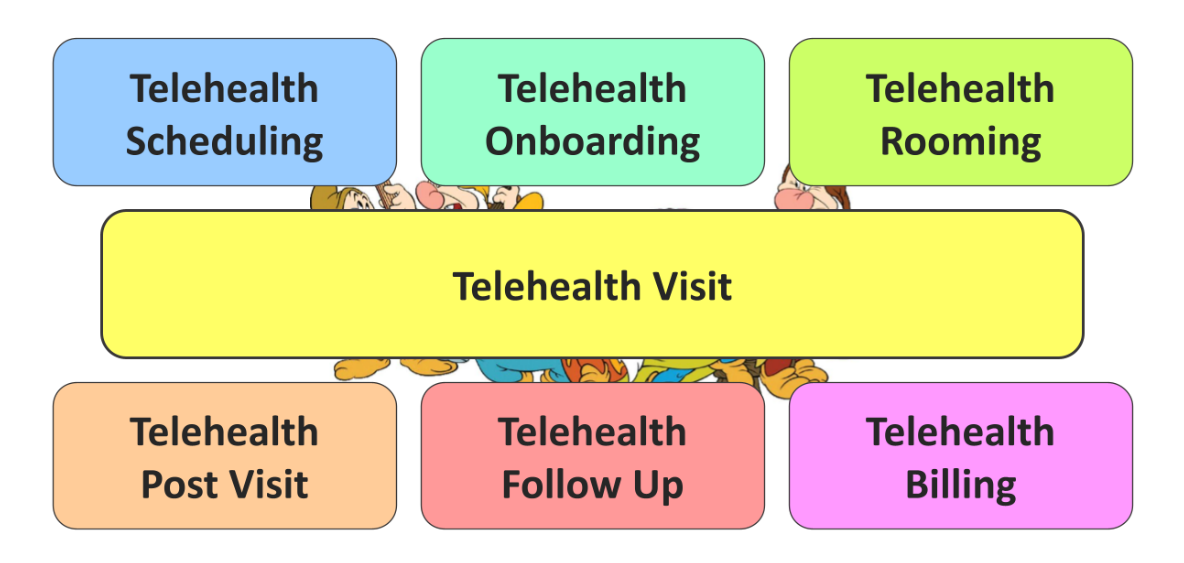
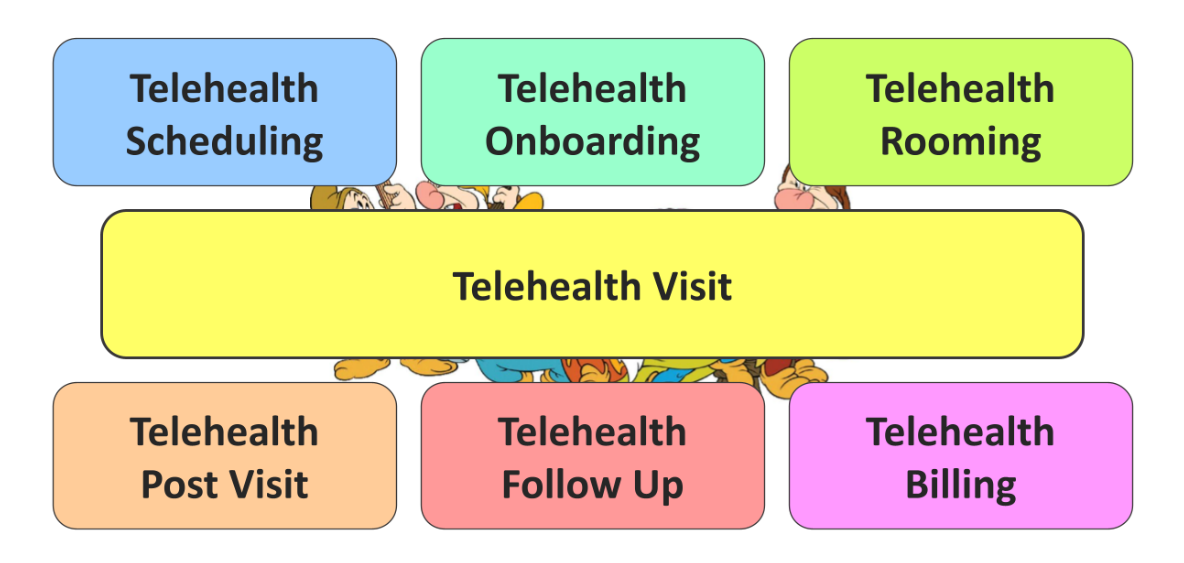
Finally, and I’ve said it for over a decade, telehealth success is about workflow success – which finds itself high up in the list, too, though not as comprehensive as our 7 Telehealth Workflows (“Thworfs”).
On the criticism side, some of the recommendations are a bit bland (e.g., on legal and regulatory compliance), but yet still accurate (e.g., malpractice liability can be different in a telehealth environment).
A Conclusion and a Limerick
Overall the responses to my two key questions were comprehensive, well articulated and quite a few levels about common sense. They were also quite detailed, yet pithy and almost could stand on their own as good guidance.
For good measure and fun (since I had read about someone asking it to write a song), I asked for a limerick on telehealth. Here’s the poetic response:
“Can you write me a limerick about telehealth?”
There once was a telehealth trend
That helped folks from end to end
With screens they’d unite
For virtual delight
And saved them a journey to bend!
Okay, that is pretty clever, right? With constructs such as “end to end” and “virtual delight” the style is pretty nice. And the lyrical freedom to use “saved them a journey to bend” is in my book pretty clever!
So, overall I found this educational, entertaining and impressive. It’s definitely great for high-level thinking, collecting ideas to be more comprehensive, thus a helpful tool.
I’m curious — have you used ChatGPT to have a conversation about telehealth or digital health? What did you ask? What did you think about the response?








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.