These days, when people refer to telehealth, telemedicine, or virtual care, the most common use case that comes to mind is the live video visit.
Yet telehealth, defined as “delivering care at a distance”, includes a number of different “virtual care” modalities, including virtual physical exams, secure messaging, digital therapeutics, and remote physiological monitoring (RPM).
The Value of Periodic Vital Sign Collection
If there’s one thing I’ve learned in my 22+ years in healthcare, it is that when clinicians have good data about a patient’s history and current condition, they can make much more informed, much better care decisions.
The one-time snapshot of a blood pressure in the clinic office hides the ups and downs and may even be exacerbated by the “white coat” syndrome or the stress of having to see the doctor.
Similarly a one-time data point of a weight, pulse, or even temperature is no reliable indication of how the patient has been doing in the previous days or weeks.
Since the treatment of chronic conditions often involves the prescription (and dosing) of medications, getting near real time feedback on the efficacy of the drugs is critical to achieve maximum benefit.
As we know in engineering systems, feedback is critical to the quality control of any system – without a speedometer in your car, you’d probably be collecting speeding tickets left and right. Without the automatic tire pressure sensors, you may not notice a tire going flat until it creates a dangerous situation.
The same is true in healthcare about vital signs – which is why in the ICU and other areas of the hospital most patients are connected to a continuous vital sign monitor, to closely keep watch on the patient’s most critical vital signs.
The problem that RPM thus solves, is to get better insights into the patient’s well being, without the need of hospitalization, daily home care visits, or frequent trips to the clinic.
RPM defined
While the main image of our article above may conjure up the definition of “Revolutions per Minute (RPM)”, our focus is on the medical use of this initialism.
There are two ways to translate the initialism “RPM”: Remote Patient Monitoring and Remote Physiological Monitoring. While the latter term is more accurate (and less Orwellian than the former), the former term has been in use longer, so that use is shifting. We are obviously not interested in monitoring patients, but rather in data that can get us insights into the health of the patient.
Here is a good definition we’ve used:
RPM: The continuous or periodic remote collection, transmission and review of physiological data to inform care decisions.
What I like about this definition is especially the last part: the data must be presented in a way that facilitates the making of care decisions. That is the primary purpose of RPM.
RPM System Overview
A typical RPM system comprises three parts:
- the home-based data collection and transmission
- the cloud-based storage system
- the presentation and review system
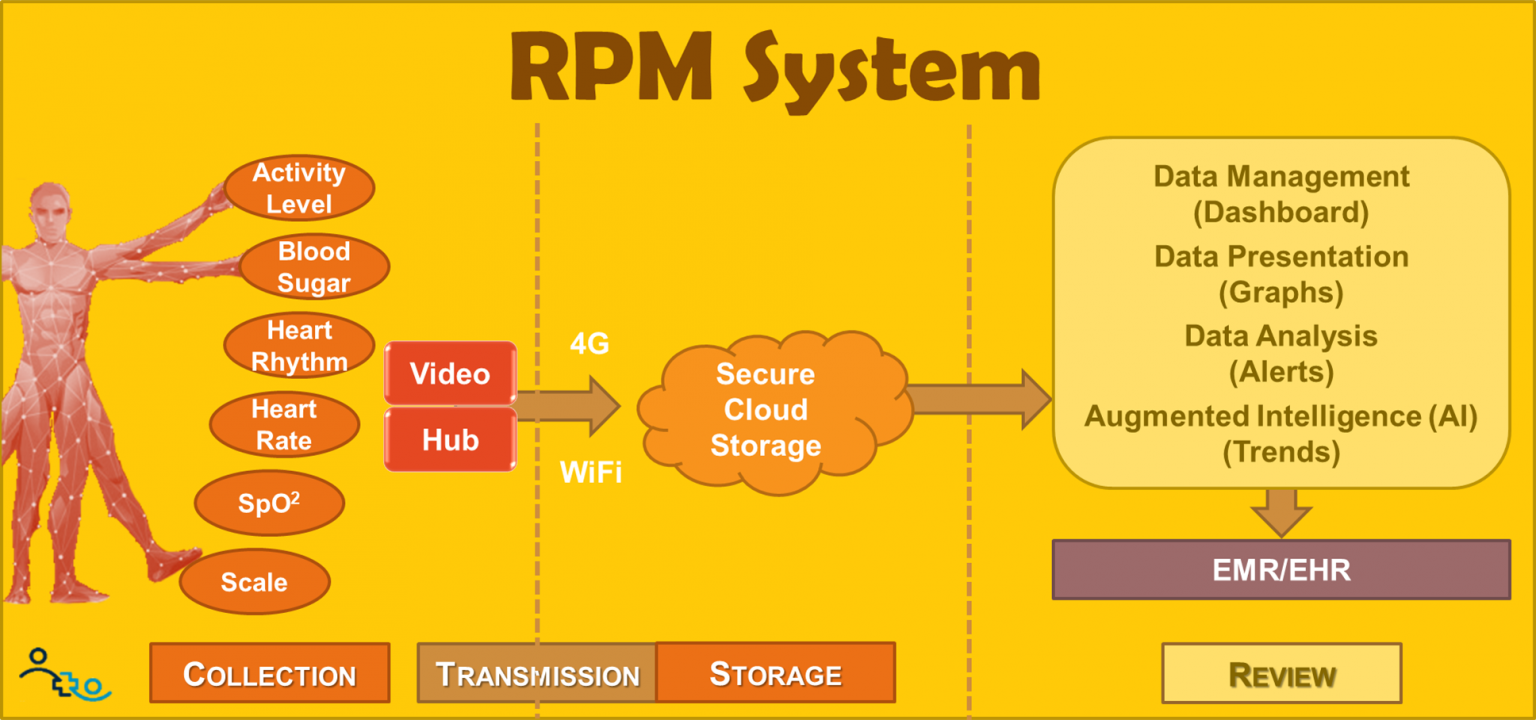
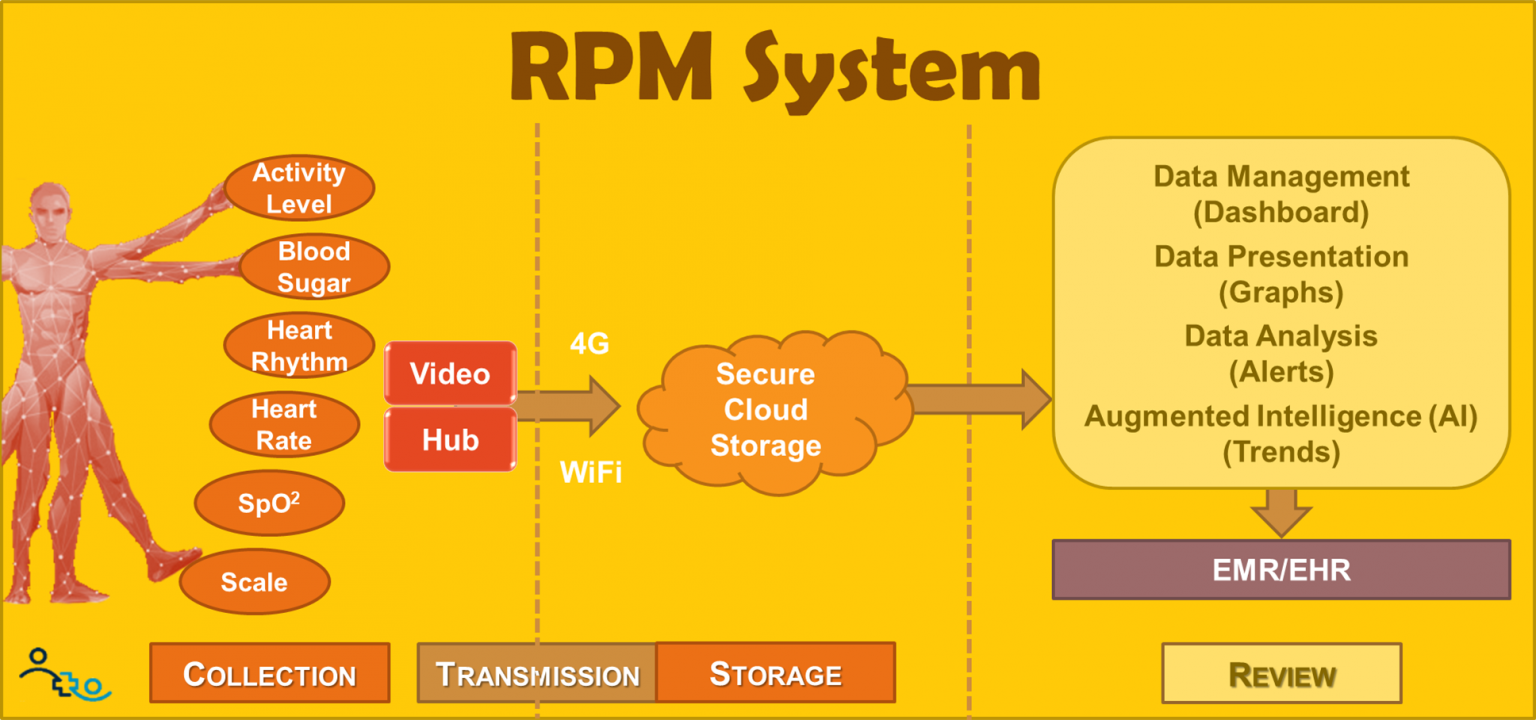
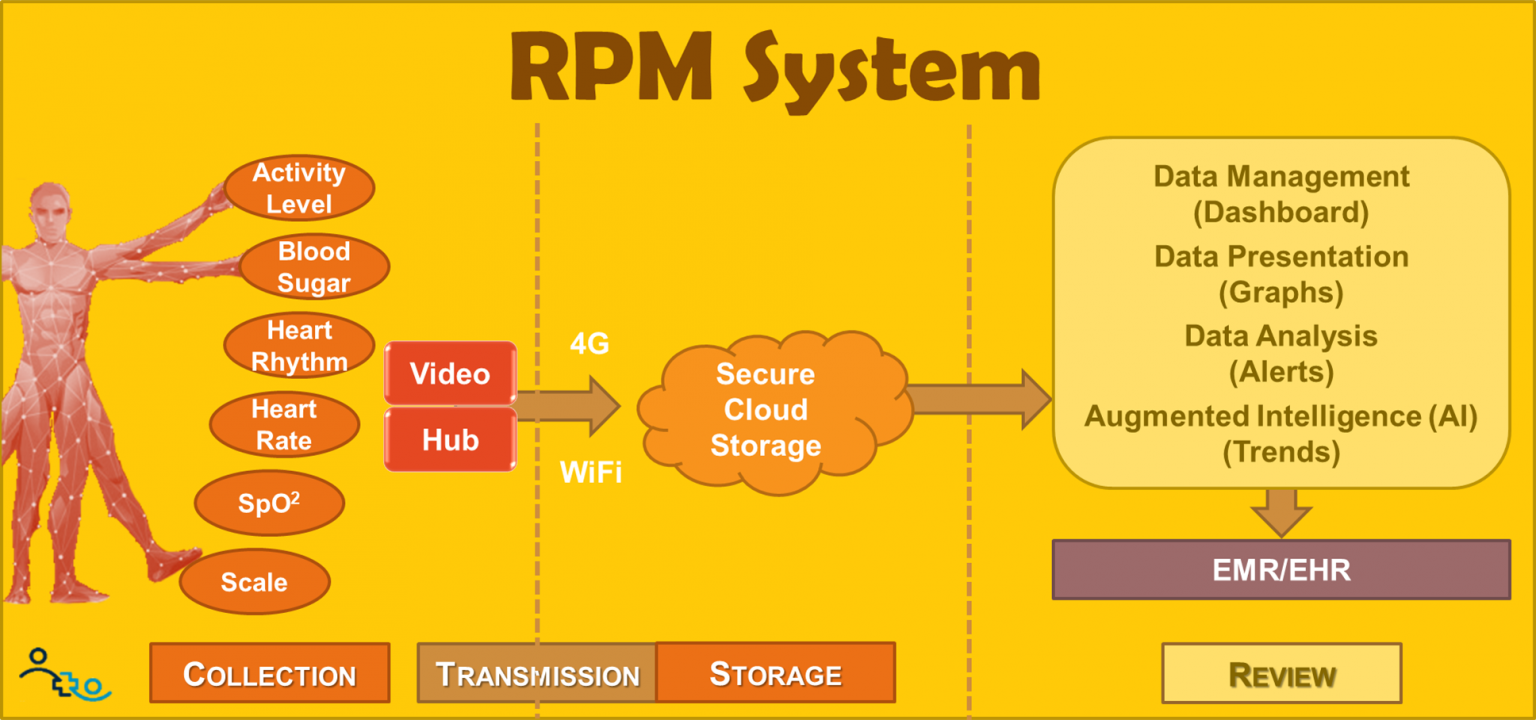
The home-based collection system includes a variety of different data acquisition devices such as a scale, a blood pressure cuff, and pulse oximeter, a glucometer, embedded accelerometers, etc. In addition most modern RPM solutions include a central hub that wirelessly collects the various vital signs and transmits them via the cellular network or WiFi to a centralized secure storage system.
Some systems also include a display screen (e.g., a tablet) that can be used in many ways – to prompt patients to collect the data, to remind patients of other tasks (e.g., refill medication), to ask daily questionnaires (e.g., a PHQ-9) and, when equipped with a webcam, to converse with their providers and nurses via video.
Once transmitted to the storage location, the data can be accessed and used to monitor a multitude of patients at the same time. A proprietary data presentation is optimized for the unique nature of the longitudinal data (something most EMRs are not capable of handling). In addition to dashboards to quickly identify those patients that need immediate attention, these review systems also include rudimentary data analysis (alerts) and increasingly sophisticated predictive analytics, or AI to detect the slow onset of deterioration.
Some of the more sophisticated RPM solutions also integrate with the standard EMRs for long-term storage of the data in the patient’s medical record.
Uses of RPM
The uses of RPM are dependent on the where the system is used: in a clinical or in a non-clinical setting. The most common use of RPM-concepts in the clinic setting is the setup of an eICU. This provides the opportunity for rural hospitals to have 24×7 access to experienced critical care staff.
The more common outpatient scenario (and the scope of our basic introduction to RPM) is the use of RPM in the home (or a home-like setting). Here the primary use cases include:
- short-term readmission prevention
- long-term chronic disease management
- long-term disease onset monitoring for at risk populations
Short-term readmission prevention offers one of the highest ROIs of any telemedicine service – as high as 1:15, i.e., every $70,000 invested yields over $1M in savings, bonuses, avoided losses, etc. The primary value here lies in avoiding readmissions that are not reimbursed (e.g., within 30 days of discharge) and also to avoid penalties (primarily from CMS but increasingly also from private payors).
The most common diagnoses qualifying patients for participation in a Readmission Prevention program include COPD, CHF, and MIs.
Long-term chronic disease management has become a big focal point over the last years, not the least due to the payment for every 20 minutes of chronic care management. This may or may not involve the use of RPM equipment, depending on the condition of the patient.
From a health system’s perspective that is trying to decide where to get started with RPM, we offer the following use case prioritization as depicted in the chart:
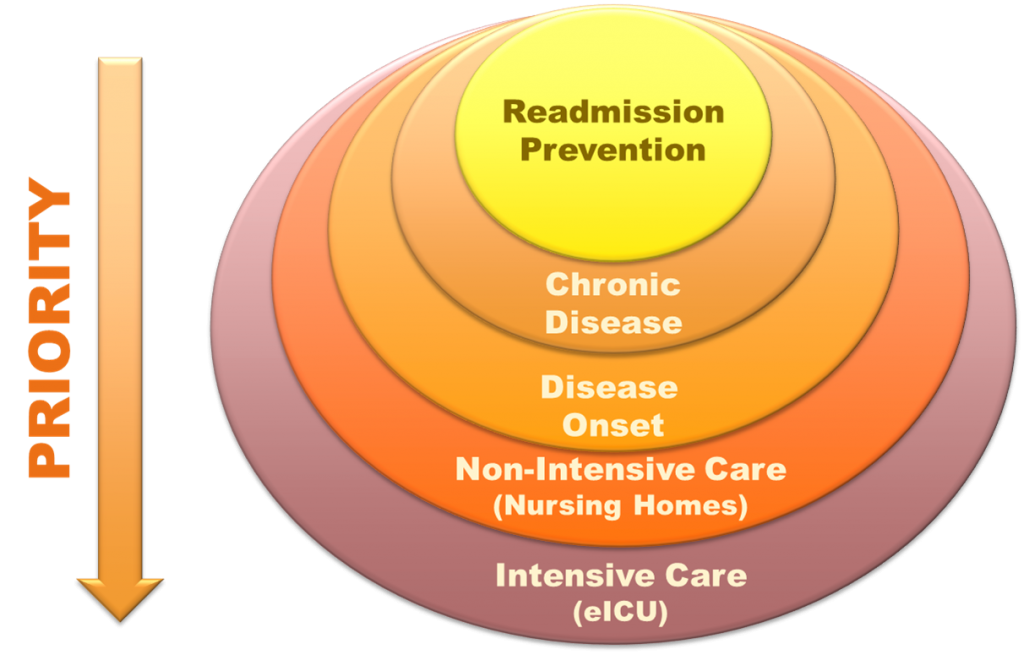
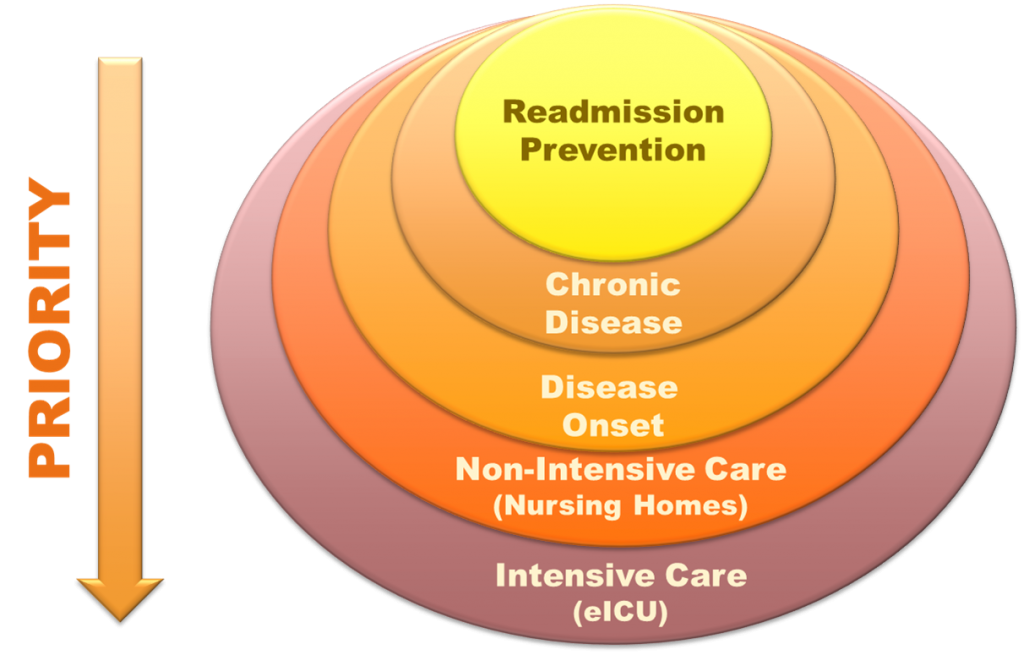
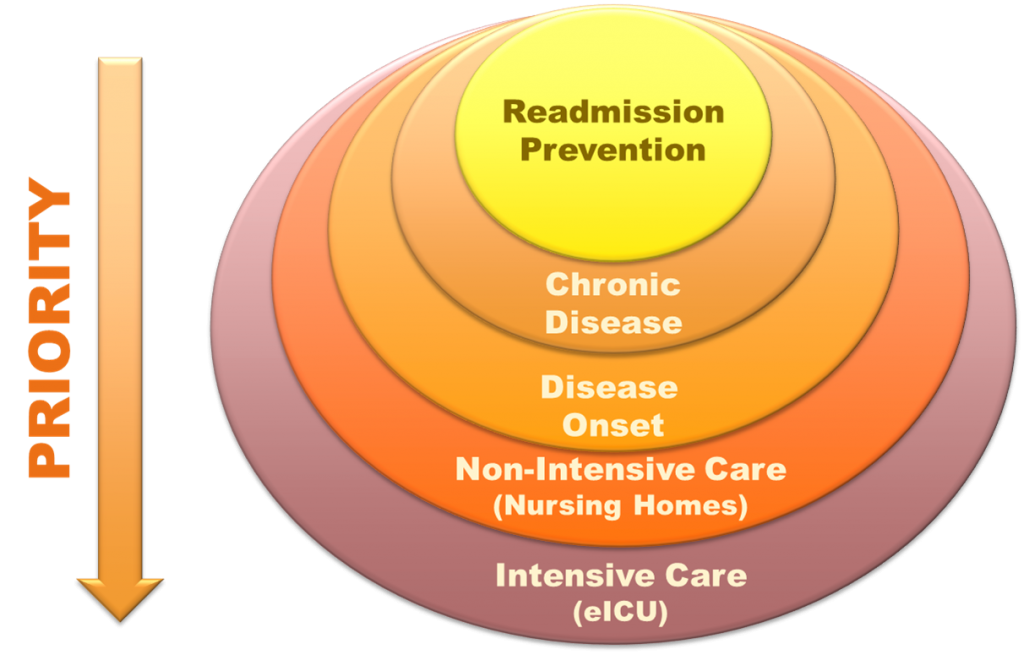
In this chart, Readmission Prevention offers the highest, quickest ROI whereas eICUs are expensive to implement but also yield a tremendous ROI for the rural hospital aiming to keep patients in their community.
RPM Benefits
Aside from the obvious benefits of improved health outcomes and avoided utilization there are a number of not so obvious clinical benefits and opportunities, especially around patient engagement:
“Seeing your body” increases patients’ engagement: the more patients understand the cause and effect of diet and exercise on their “values”, the more they are willing to be engaged in the care of their health. With patient activation being one of the critical factors for moving the outcomes needle into the right direction, RPM offers a tremendous opportunity, when used appropriately.
Daily Insights allowing adjustment of the Care Plan: Oftentimes weeks can pass before the care team learns about the changing condition of a patient. Having daily “interactions” allows for rapid changes and improvements to the care plan, such as adjusting medications, starting or stopping physical therapy, etc.
Opportunities for Just-in-Time Education: The collected data can also be used to educate patients on the effects of their actions. My favorite anecdote is of a patient whose fluid retention increased the day after going to the Chinese Buffet. Through the data, the monitoring nurse could illustrate to the patient the effect of the high salt intake in the restaurant. Another example of patient activation!
Better “exam” capabilities – not “flying in the dark”: This benefit is the one we will see more exploration of and more innovative technologies for. With the high convenience of virtual visits now experienced by millions of patients, clinics can deploy RPM tools that can aid in the proper full-spectrum exam, at least to the extent that it is regularly performed for a traditional in-person visit.
Establishing a Baseline to detect onset of disease: We know that, especially in health, an ounce of prevention is worth a pound of cure. Early “deviations from the norm” (especially when genetically expected) can be counteracted early on, never leading to the secondary and tertiary consequences.
With Video, opportunities for interactive visits: As mentioned above, an RPM solution with a screen (e.g., a tablet) is a great tool for the care team to stay in touch with the patient. This could be the monitoring nurse, a case manager, an endocrinologist, a counselor, or the primary care clinician. (Which is a third example of using RPM to motivate patients to actively participate in their care).
The RPM and CCM Bonanza
Last but not least I have to comment on the wild west of RPM and CCM (chronic care management) companies out there.
The 2019 creation of reimbursement codes for RPM by CMS has spurred a bonanza of hundreds if not thousands of RPM/CCM service/solution startups with dazzling calculators boasting the phenomenal revenue potential to lasso physician practices. A simple Google search for <(RPM or CCM) “revenue calculator”> yields 27,400 results!
In all fairness, I should point out that some of the mature companies are also listing the impact on outcomes (mostly reduction in ER utilization), though there are no dazzling calculators there. One company proudly reports 87,000 patients enrolled with 30% reduction in all-cause hospitalization — at a cost of 625,400 staff hours and $52M in reimbursement.
Sounds impressive? Yes, impressively expensive ($600/patient) and not very telling, as we don’t know the actual number of hospitalizations that were avoided, and how many of those 87,000 patients actually would have never been hospitalized.
Is it 10% of those patients who would have seen a hospitalization? And that number was reduced by 30%? That would be 2,610 hospitalization avoided – at a cost to the system of about $20,000 per avoided hospitalization. Hmm, not so impressive now, is it?
Of course if you pick your patients wisely (let’s say that 50% of those would have experienced a hospitalization), then the numbers change a bit – to $4,000 per avoided hospitalization. I.e., there could be a potential return on investment for the system as a whole — but only if the patients are wisely selected and not just for “revenue generating reasons”, as the fancy calculators indirectly seem to suggest.
In summary, while I’m all for bolstering a clinic’s financial bottom line, I’m concerned that once payors perform a true ROI analysis, that it will get much harder to get adequately reimbursed for RPM, which would be a shame. I thus hope that some system measures can be created to counterbalance an overuse of RPM.
RPM is here to stay (and grow)
While with the increased use of electric cars the RPM meter on a car dashboard will disappear, RPM for “driving patients’ health” is here to stay and will grow exponentially in the next years to come.
Many payors (CMS, most State Medicaid programs) are recognizing the value or RPM to avoid expensive utilization by being able to intervene earlier and are paying reimbursements that are pretty much on par with the expenses and overall value of RPM to an organization.
It thus behooves every clinic, health center, and health system to seriously evaluate where RPM can help move the needle on patient outcomes, patient engagement, quality measures, and (yes) revenue. There’s nothing wrong with making money if it saves the system money (and hardships for the patients).








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.