In last week’s Telehealth Tuesday article I posed the question:
The answer?
No, Telehealth is not Rocket Science.
But getting clinicians to use telehealth well, is.
To get clinicians to embrace telehealth, clinicians need Awareness, Desire, Knowledge, Skill, and Reinforcement:
(1) The Awareness that Telehealth is a viable and valuable way to deliver care.
(2) The Desire to integrate Telehealth into their practice.
(3) The Knowledge of how to use telehealth effectively.
(4) The Skill and experience to use telehealth well.
(5) Reinforcement and support to keep using telehealth when appropriate.
So how do Create Awareness and Desire, Provide the Knowledge and Skill and Supply the Reinforcement?
Let’s review some of the tactics that the best users of telehealth employ.
Creating Awareness and Desire
The creation of awareness and desire is primarily a leadership function.
For many hands-on clinicians who are focused day in and day out on their valuable work of patient care, the larger picture of telehealth’s strategic importance in our rapidly changing (healthcare) world is not imminently obvious. For example, the patients they no longer see because they are receiving most of their care telemedically through other services, are easy to miss.
There are two simple and important principles to creating awareness and invoking desire: information and inspiration.
The primary tool to convey to the clinical workforce the importance of telehealth for the long-term sustainability of the organization is a Telehealth Strategy that clearly lays out the WHY, the WHAT, and the WHEN.
The best telehealth strategies set forth a bold vision (“WHY”) that recognizes the importance of digital health and derives from it a set of strategic objectives (“WHAT”) that are aligned with the organization’s overall strategy. A roadmap of strategic initiatives (“WHEN”) outlines the work ahead (e.g., employer based telehealth, remote physiological monitoring, mobile clinics, etc.).
Once the telehealth strategy has been developed, the leadership team (and especially clinical leaders) must share the vision in their communication with the clinical staff. Increasing research into the efficacy of telehealth, the changing healthcare consumer expectations, evolving technologies, and competitive pressures from national and regional providers, insurers, and non-traditional competitors all need to be conveyed as driving forces behind the need to become proficient with telehealth.
Another tactic is the implementation of a telehealth performance management system that measures utilization, satisfaction and reimbursement. Coupled with benchmarking (comparisons with similar organizations’ use of telehealth) it can provide additional “social proof” and motivation for clinicians to engage in the use of telehealth.
Providing Knowledge and Skill
While Awareness and Desire are needed, they are by themselves not sufficient to motivate clinicians to use telehealth and certainly not sufficient to use telehealth well.
The majority of clinicians are quite apprehensive about using telehealth, for a variety of reasons.
While the “delivery of care at a distance” is not rocket science, it is still a skill that needs to be practiced to do it well and few if any clinicians have ever been formally trained in the proper use of a webcam to create a good connection with the patient on the other side. A brief training and practice sessions on “webside manners” and on properly conducting (and documenting) virtual physical exams will go a long way to instill the necessary confidence.
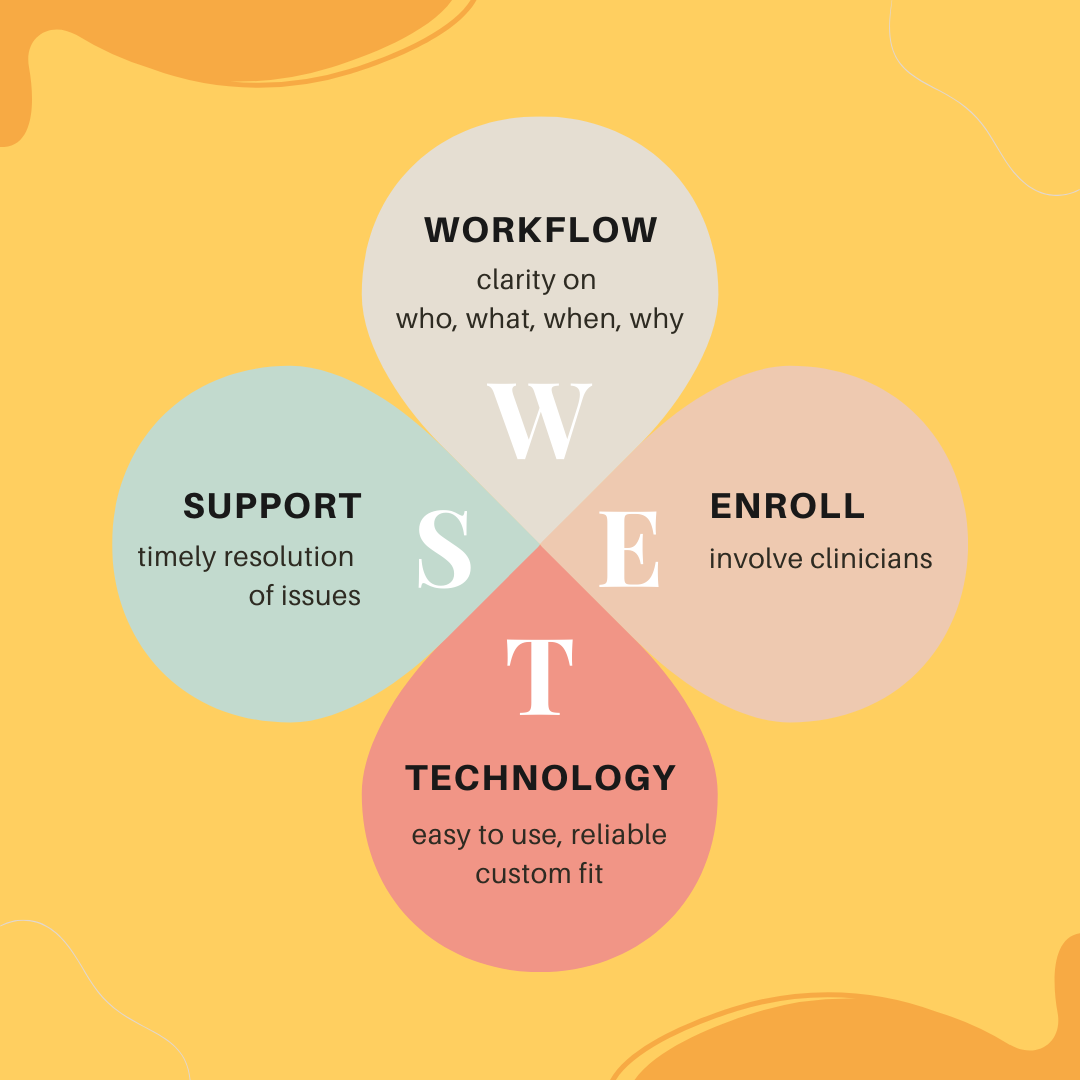
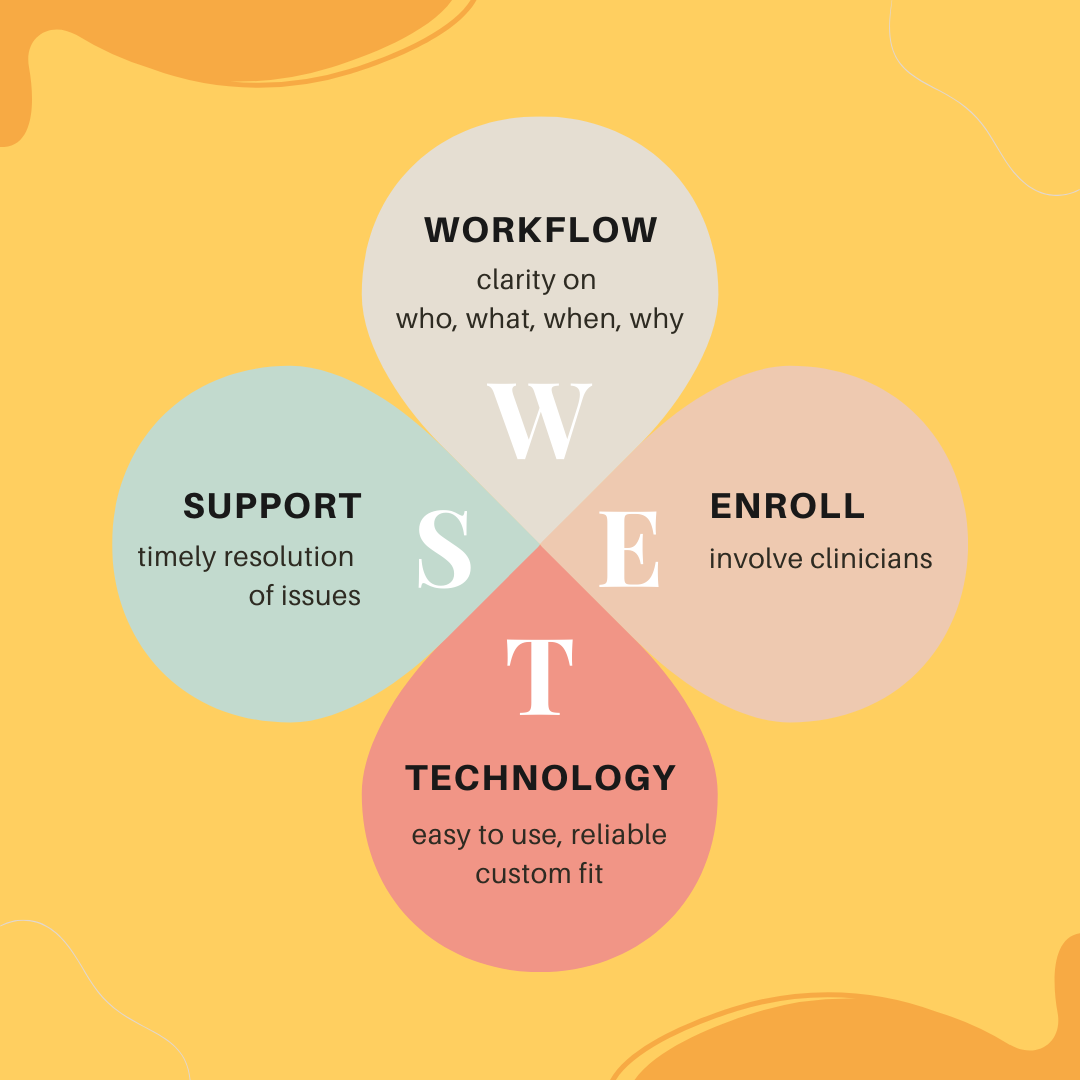
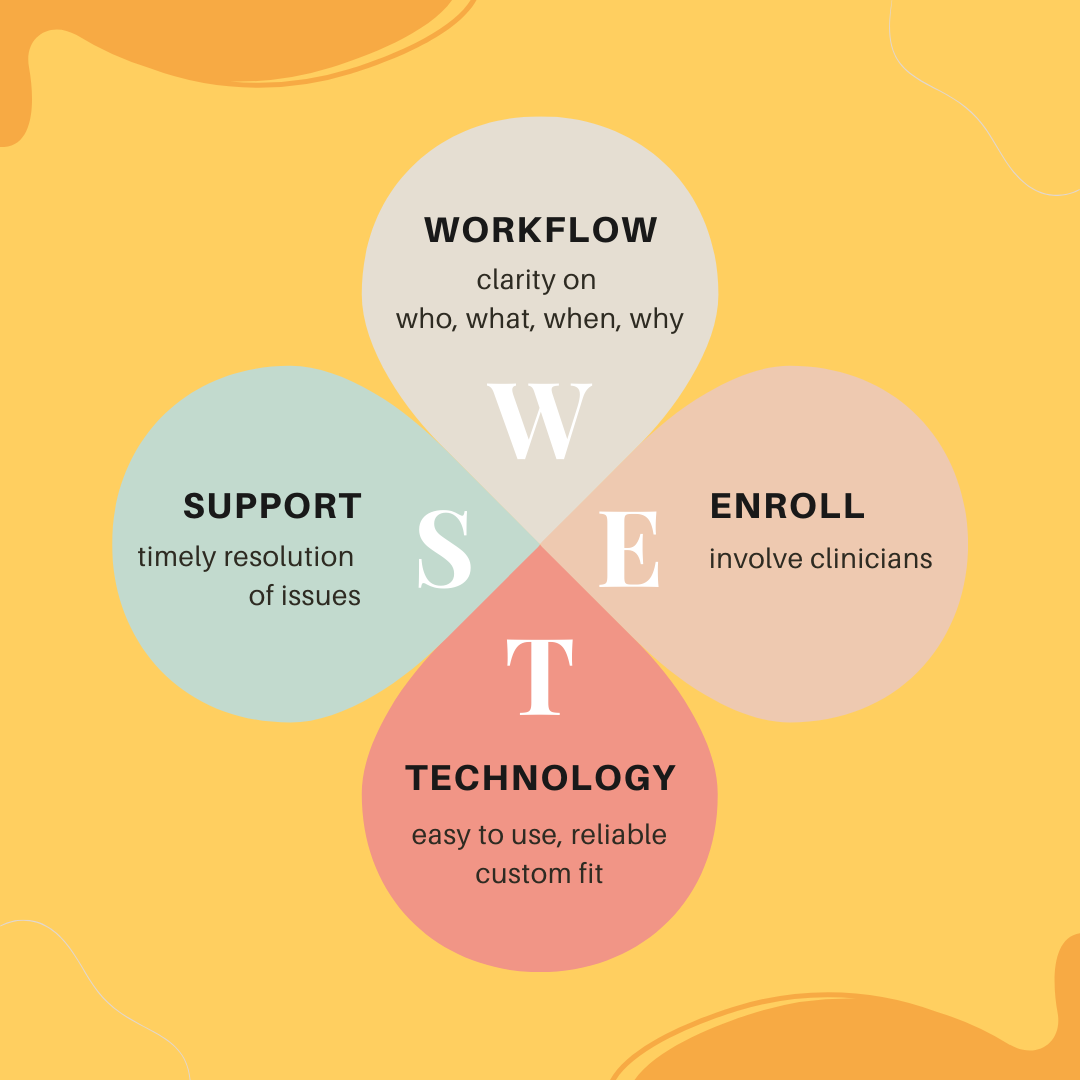
In addition to training, easy access to operational support and the occasional technical support is also critical for the increased use of telehealth by clinicians. The majority of frustrations with telehealth originate from breakdowns in communication and readily available operational support is critical to keep frustrations to a minimum.
Also — technology is great when it works, but when it does not, nothing is more frustrating to clinicians not being able to quickly get technical support. For telehealth to work well, easy access to support is thus key!
A very effective proactive way to avoid problems — especially first first-time telehealth patients — is a quick Telehealth TechCheck a few days prior to the visit. These brief calls are designed to ensure that both the patient and the clinician will have a great experience.
Supplying Reinforcement
It is human nature to always seek the path of least resistance and going back to the “old days” of doing things always seems to be easier (and more enjoyable).
Once an organization has committed itself to the sustainable growth of telehealth it is imperative that the leadership also monitor and manage the performance of the organization’s telehealth services.
The typical key performance indicators include utilization by specialty, modality, location, and sometimes down to the clinician level. This barebone metric can provide a good indicator when clinicians start using telehealth less. While there may be seasonal variation or normal fluctuations, more often than not it is unresolved frustrations that lead to clinicians’ unwillingness to use telehealth as often as they could. Utilization data provides good insight into that.
The next set of performance indicators include the satisfaction of both clinicians and patients, which should be collected periodically (every 3-4 months) for a few 3-5 days. This snapshot first of all demonstrates that “leadership cares” — but only if leadership acts on the data, which is critical.
Poorly Delivered Telehealth is Unacceptable
Telehealth is undoubtedly here to stay and a slow but steady integration of telehealth as an alternative care delivery modality is required by all but a few healthcare providers to stay relevant.
Telehealth is not Rocket Science. Most Telehealth solutions are very mature, increasingly user friendly, secure, and reliable. Defining the 7 core telehealth workflows can be involved, but still is quite easy.
What’s missing in many organizations (especially smaller, rural clinics and agencies) is a clear communication of the imperative to embrace telehealth to stay relevant and clearly defined support in the form of a Telehealth Coordinator.
Without it, clinicians will stay hesitant or reluctant to use telehealth and will not be skilled enough to do it well.
But the “rocket science” on getting clinicians to use telehealth well is clearly laid out in this article: from a telehealth strategy and performance management to clinician training and support: the elements are well understood, well defined.
Are you ready to guide and empower your clinicians to do telehealth well?
Do you have Questions? Are you interested in finding out in which areas your organization could benefit from improvements most? Then connect with me.








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.








