A couple of weeks ago one of the telehealth trailblazers of the last 30 years, Dr. Joseph Kvedar, reflected on the blazed trail he’s been on thus far and mused on what lies ahead.
When in 2016 I revised my basic Telehealth Taxonomy that I first developed in early 2012 to include Connected Health, I took my inspiration for the definition of Connected Health from Dr. Kvedar’s book “The Internet of Health Things”.
While I had settled on a definition for telehealth as “delivering care at a distance” and telemedicine (a subset of telehealth) as “practicing medicine at a distance”, borrowing and building on his idea I simply declared that the purpose of Connected Health, it’s raison d’être, is “Enabled Wellness”: to (digitally) empower us to “be well, get well, and stay well”. I have not felt the need to update the definition ever since.
I’m therefore indebted to Dr. Kvedar for shifting my thinking away from finding a definition, but rather focusing on the outcome. Based on my 12 years at the Mayo Clinic, I think that is a common hallmark of all great clinicians: to focus on the outcome, not the means or the approach.
Since his book debut, Dr. Kvedar has gone on to lead the Board of Directors at the American Telemedicine Association and has been a strong, visible supporter of telehealth.
Dr. Kvedar’s Four Focus Areas
In a recent article on LinkedIn, “What’s a telehealth evangelist to do?”, Dr. Kvedar reflected on his journey in telehealth since the mid-’90s, ending his reflection on four key items he suggests we should focus on to increase the adoption of telehealth:
(A) foster providers’ attitude and use towards telehealth,
(B) change payers’ perception of telehealth,
(C) boldly encourage more comprehensive clinical guidelines for telehealth, and
(D) invest in technologies that make patient data clinically accessible.
His list is a nicely balanced list that focuses on the key elements of telehealth success: clinician attitude (A), money (B), clinical efficacy (C), and technology (D).
In a true masterful understanding of the true power of telehealth as a clinical service, technology comes last in his list, and it’s not even about the technology itself, but the technology as a means to get a more comprehensive picture to the clinical decision maker: more insights about the patient.
I also love how he rightfully acknowledges that the biggest hurdle to widespread use of telehealth is the clinicians’ attitude and professional use of telehealth. A few bad actors give a bad rep to the whole telehealth community and provide fuel for the nay-sayers and objectionists on the sidelines.
But it is not just intentional wrongdoing, but rather the lack of basic training and support to overcome clinicians’ common objections to telehealth that in my opinion is leading to many clinicians’ reluctant use (or inadvertent misuse) of telehealth.
He ends his article with an invitation to the reader to let him know: What’s missing?
Here’s my reflection on that prompt.
The Roadmap to Optimally Integrated Virtual Care
I see the roadmap towards Dr. Kvedar’s vision of “optimally integrating virtual care” happening in three phases: Integration, Acceleration, and Transformation.
These three phases also “happen” to overlap with the Telehealth Maturity Model we’ve been using in our consulting practice to guide organizations in their optimal use of telehealth.
Note: I’ll cross reference Dr. Kvedar’s four points throughout my musings (cf. A-D).
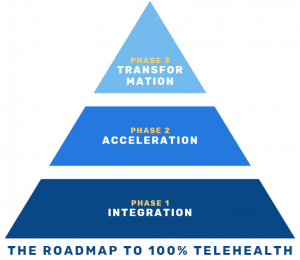
Phase 1: Integration
Just like in the pyramid, Integration forms the foundation, the basis of phases 2 and 3. This is where a bulk of the work has to happen now, so we can build on it later to fully reap the benefits that virtual care has to offer.
First off, changing the hearts and minds of clinicians (cf. A), administrators, executives, and payers (cf. B) is an exercise in change management. For change to start, there first needs to be an awareness of the why and a desire to change. Therefore the first stop on my roadmap is that every organization must have (1) a Telehealth Strategy.
The strategy must clearly define the strategic case, the business/financial case, and the clinical case as to WHY the organization will be investing in the increasing use of telehealth and other virtual care modalities.
Next stop: (2) Clinician Engagement (cf. A, C). At the heart of telehealth adoption is to convince clinicians that virtual care is, in many circumstances, an appropriate, proper way to deliver care. This stop requires the visible clinical leadership, includes clinician training (with training on webside manners), the development of clinical guidelines (cf. C), and providing adequate and easy to reach operational and technical support.
The third stop is actually a prerequisite for the second: (3) Telehealth Workflows. Care delivery done well, is a well-orchestrated series of steps by multiple actors collaborating to create a superb patient care experience (that also is highly satisfying for the clinician). While the clinicians’ focus should rightfully primarily be on the actual visit, many things must happen before and after the visit so that both the patient and the provider can have a superb experience (e.g., including a Telehealth TechCheck for patients new to telehealth).
Since this particular part of the journey is about creating sustainable change, the last stop in this phase is (4) Performance Management. Whereas leaders in the first stop defined the direction, executive and clinical leaders must continuously provide reinforcement until the change sticks. This includes defining which telehealth performance metrics are important (it could be these five) and how to measure and manage them.
Phase 2: Acceleration
Building on the foundation of full telehealth integration and a solid, predictable, well-managed performance, the organization is now ready to turn its focus back on technology to advance utilization: Stop (5) Digital Health Integration stipulates that we go beyond the mere video visit or period transmission of vital signs. Digital Therapeutics open a new world of managing chronic diseases, and leveraging patient-generated health data (cf. D) provides clinicians with a richer and more complete picture of the patient’s experience since the last visit.
But this stop requires that the organization is ready to accelerate their adoption of Digital Health Innovation. New technologies must be evaluated in weeks not months and deployed in months not years. The avalanche of digital health innovation is ripe for the picking with high value solutions, but only for those organizations whose clinicians have been prepared to embrace technology. And telehealth is the perfect “entry drug” to get them hooked on using technology.
Similar to the first phase, this phase needs a similar reinforcement mechanism: (6) Adoption Management, where the focus evolves from managing the performance (4), to finding strategic ways to increase the use of care that is delivered virtually.
Once a critical mass of clinicians’ are embracing telehealth, the herd mentality and social acceptance dynamics will set in and telehealth use will grow, coupled with an increasing demand by the modern healthcare consumer. Already the bombardment with convenient “virtual first” options by payers, Amazon Clinic, and self-insured employer-sponsored plans (such as Walmart) are changing the expectations of the average patient on how convenient access to standard care should be.
Phase 3: Transformation
In the third phase, fueled by widespread acceptance, I predict that traditional in-person outpatient care delivery will completely be turned on its head.
Whereas in prior years strategic planning retreats focused on increasing the integration of digital health solutions (including telehealth), inevitably someone will ask the unspoken question: what would “all virtual” look like — and how “in-person care” could be integrated into that approach.
In the late 2000s, Denmark closed most of its outdated hospitals, replacing them with fewer, more centralized hospitals effectively reducing bed capacity (as established by prior actual utilization) by 20%. Their marching order: Telehealth works, go figure it out.
Because every system is perfectly designed, to get the results it gets, and that system of fewer bed capacity coupled with the mandate to go and innovate worked.
100% Telehealth is not a Dream
Whereas Dr. Joe Kvedar inspirationally talks about the goal of “optimally integrating into the care delivery mix” my vision goes further. I want to see 100% telehealth, so that in the future, as he said”, we can drop the “tele” and it’s just medicine.
But 100% telehealth does not mean that 100% of all care (or all outpatient care) is delivered virtually.
No, my definition of 100% telehealth is simply that telehealth will be delivered every time (1) it is clinically appropriate, (2) the patient wants it, and (3) the patient has the technical capabilities to do so.
Telehealth is a clinical service, offered to the patient at the discretion of the clinician — but not based on the clinician’s level of comfort, but based on the clinical and in some cases the patients’ socio-economic circumstances.
That’s the future I’m building a road towards.
Thank you, Joe, for the inspiration and to invite us to contribute to your vision where care received is simply medicine.








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.








