As Telehealth becomes an increasingly important strategic tool in attracting and serving the modern healthcare consumers’ desire for convenience, it is imperative that healthcare leaders pay attention to the performance of their telehealth services. As the saying goes “hope is not a strategy” and a poor patient experience and low clinician satisfaction will jeopardize your clinic’s ability to leverage telehealth as a viable (and increasingly expected!) care delivery alternative.
With telehealth having been launched virtually overnight during the Covid-19 health crisis in most healthcare organizations, many leaders are pretty much in the dark when it comes to their insights into the performance of their organization’s telehealth services. Without “knowing how it’s going”, healthcare organizations risk alienating clinicians, limiting patients’ access to care, and hurting their bottom line.
Over the past two articles I laid the foundation for today’s topic, describing the various types of telehealth performance measures and providing a set of sample requirements to consider when developing your “Telehealth Performance Dashboard”.
In this week’s column, I’ll be sharing with you the top five most critical telehealth metrics that every healthcare leader needs to pay attention to.
A Mindset Shift
While the percentage of healthcare leaders that regard telehealth as a passing fad is shrinking, the notion of measuring the performance of this (or any) healthcare service is not as widespread as it should be. In our observation this is due to a mix of never having managed by fact and not knowing which metrics are critical and useful.
As I covered earlier this year (e.g., when talking about the VA Telehealth Network’s 2023 Benchmarking Report or Sage Growth Partners’ report), telehealth use remains high and of interest: 88% of providers realize that “patients would be disappointed if [we] stopped offering telehealth appointments.“ Or: 92% of providers in practices indicate telehealth having a major or moderate impact on patient access.
Therefore, while the frontline providers realize, when pressed for an answer, that telehealth is valuable, desirable, etc. But many providers (especially in primary care) also demonstrate a high unwillingness to use telehealth more frequently.
Given the market dynamics of consumer demand and fierce competition, it is up to the leaders to start measuring and managing performance. Which will inevitably show where the organization has to invest in optimizing telehealth.
What is needed at the leadership level is a mindset shift to regard telehealth not as an alternative to in-person visits, but as a viable alternative care delivery modality and a new clinical service offering.
As we discuss with the leadership of our health system clients — you are now managing three distinct service lines: inpatient, outpatient and virtual patient.
Once leadership teams embrace the notion that telehealth (or virtual care) is here to stay, for good, they realize that in order to improve the service, they need to know more about its performance.
The Critical Set of Telehealth Metrics
So what is the critical set of metrics to measure the performance of a telehealth service?
The key metrics come from three performance areas: service performance, technical performance, and financial performance.
Service performance examines the acceptance of the service by patients as well as by the clinicians. With a great service experience on both sides, telehealth is not sustainable.
Technical performance ensures that the technology (which includes connectivity) can support a seamless, painless experience, where the technology ideally just fades into the background.
Financial performance ensures virtual care’s contribution to the bottom line of the organization.
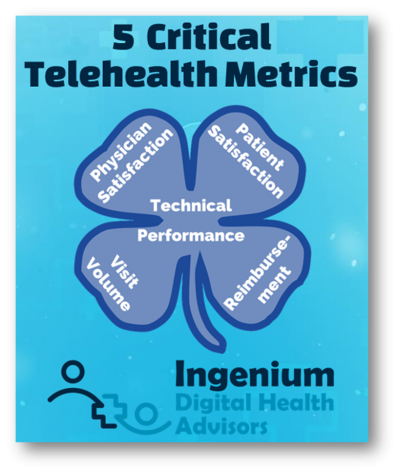
The 5 Critical Telehealth Metrics
Here are the 5 critical telehealth metrics that healthcare leaders need to pay attention to in order to ensure that their telehealth services are performing as well as they should:
Service Performance
1. Clinician Satisfaction
2. Patient Satisfaction
Technical Performance
3. Technical Performance
Financial Performance
4. Overall Visit Volume by Modality
5. Overall Reimbursement by Modality
Let’s review the nuances of these 5 critical telehealth metrics.
Service Performance Metrics
The most critical metric of all (and the one most health systems ignore) is the satisfaction of the clinicians. When we work with clients we ask the clinicians, for example, “the telehealth visit was as good as an in-person visit” and we repeatedly get 4.3 or 4.4 on a 5-point Likert scale, so high satisfaction across the board is possible.
The second service performance metric is patient satisfaction. Typically, the acceptance of telehealth across all demographics is very high. Patients love the convenience and appreciate the efficacy with which care can be received. With our clients, we typically ask the patients “How likely are you to recommend telehealth with this provider to your friends and family?” and have gotten Net Promoter Scores (NPS) in the 70s, which is considered world-class service.
Here’s the reality: If the physicians do not like delivering care via telehealth, none of the other metrics matter much. The most prevalent root cause of statements such as “patients don’t like telehealth” is that physicians don’t like it. Even with the slickest technology and full reimbursement, if the physicians’ mindset is that telehealth is not as good as in-person care, they will find self-fulling evidence to support their sentiment.
It is therefore imperative that healthcare leaders frequently measure physician satisfaction – and then act on the data to improve satisfaction.
Technical Performance
While telehealth is not about the technology (but about the workflows and managing the organizational change), it certainly is about the technology when the technology is not working.
With regards to telehealth technology, there are a few “givens” that we assume: that the technology is reasonably usable, that it is secure and also, given good internet connectivity, reliable.
The metrics to capture under technical performance should simply be on whether the clinician and patient could easily connect and that there are no audio/visual problems.
Any deviation from the targeted goals is mostly the cause of individual circumstances on the clinician’s or patient’s side. Most user experience problems can be most easily addressed by workflow or process intervention (such as Pre-Visit TechChecks) and by training and coaching (e.g., on “webside manners”).
Financial Performance
Of the 5 critical metrics, the first 3 can be measured intermittently whereas the financial metrics should be measured continuously.
The “overall visit volume by modality” metric is critical in providing a good overall picture of the performance of your healthcare organization. It should include attributes such as date, time, provider, visit type, show/no show, and modality (one of: inpatient, outpatient, video visit, telephonic visit).
In addition to modality, clinic location and specialty are other attributes that are of value.
Semi-automated analysis of this metric can reveal a multitude of insights: comparison to prior year volumes, distribution (and shift across all modalities), adoption by individual providers or provider groups), change in no-show rates, etc.
The “overall reimbursement by modality” metric provides critical insight into the financial performance of the organization. It should include similar attributes, including date, time, provider, modality, CPT code, payor/health plan, and actual reimbursement.
Here, semi-automated analysis of this metric can reveal an additional set of insights: e.g., comparison to prior year revenue, “the cost of telephonic vs. video telehealth”, average reimbursement per visit, usage by CPT code and modality, etc.
Using the Metrics to Drive Improvement
As I’ve described in an article before, “Action is the Ultimate Value of Measuring Performance”.
To implement “paying attention to”, all 5 metrics should be reported on a regular basis (weekly first, monthly later) in the form of a telehealth performance dashboard. Each metric must have a target goal along with a predefined action list in case the metric falls short of the goal, meets the goal, or exceeds the goal.
Driving in the dark without any feedback about direction, speed or the fill-level of the gas tank can be a very dangerous undertaking, especially if you are going 80 miles an hour. It is thus crucial for healthcare leaders to invest in establishing a telehealth performance dashboard that at a minimum includes these 5 critical telehealth metrics.
- Physician Satisfaction
- Patient Satisfaction
- Technical Performance
- Overall Visit Volume by Modality, Location, and Speciality
- Overall Reimbursement by Modality, and Speciality
Next week, we’ll dive deeper into the mechanics of collecting, analyzing, and presenting these 5 metrics.
Which telehealth metrics are your healthcare leaders evaluating on a regular basis? What predefined actions have you identified to overcome the challenges you are encountering?
Are you curious about my experience at my second ever telehealth visit? Then sign up for my newsletter, where I always include a few personal words and commentary on my weekly article.








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.








