In March of 2020, the Covid-19 health crisis rapidly increased the healthcare-wide adoption of telehealth as an alternative care delivery modality. But in most clinics and health centers who previously had had no exposure to telehealth, the use of telehealth vanished as quickly as a flash in the pan.
Given the proliferation of telehealth through virtual-only providers, virtual-first clinics, and as an alternative option offered by almost all health systems, most healthcare leaders recognize that Telehealth, as a viable, parallel care delivery method in addition to in-person care, is here to stay.
Yet not all clinicians are fully on board with telehealth, and these days healthcare leaders face several challenges from a workforce shortage, a clinician shortage, and the burnout of clinical staff.
So what can healthcare leaders do to offset those challenges – reduce burnout, attract clinicians. What if the adoption and full integration of telehealth could put satisfaction and fulfillment back into practicing medicine?
Engagement in Healthcare
In healthcare, the term engagement is mostly used in the context of getting patients to participate in improving or maintaining their health. The earlier language of “compliance” gave way to the term “adherence” before finally settling on the much more apt “patient engagement”. Healthcare eventually realized that simply following orders (being compliant) would not result the same results as someone is committed (i.e., engaged).
In other industries (and even within healthcare in reference to non-clinical staff) the concept of employee engagement has long taken hold. Engaged employees are more productive, less likely to leave the organization (resulting in costly replacement), and — rather than infecting others with a negative mood — spread positivity that offsets some of the inevitable curmudgeons.
Less, however, has been talked about clinician engagement. On the one hand, the vast majority of clinicians is deeply committed to the core of their profession: to help patients to get well and to stay well. On the other hand, they are frustrated, burned out, and, sadly, increasingly suicidal.
In 2018 the top 3 reasons for physician burnout were too many bureaucratic tasks (56%), too many hours at work (39%), and the increasing computerization of the practice through electronic health record systems (EHRs) (26%). While Covid may have shifted some of those priorities, as we are getting back to a post-Covid routine, the old favorites are sure to make it to the top again.
So how could a focus on Telehealth help? Won’t yet another change and yet another technology thrown at the clinicians have the absolute opposite effect?
Not if telehealth is done well.
Telehealth Done Well Offers Freedom
For example, during Covid, many clinicians shared that they loved the variety of doing telehealth – during those circumstances that meant no masks, no PPE, no risk of getting the virus or accidentally passing it on. And it allowed clinicians to focus on what they are passionate about: to care for patients — who otherwise would not have been able to be cared for if it weren’t for telehealth.
But even prior to Covid, quite a few physicians discovered the beauty and freedom of telehealth, freelancing for one or even multiple telehealth services. In that freedom they could work from anywhere, set their own hours, sometimes even specialize in certain conditions. In rapid-fire succession they were presented with patients ready for a telehealth visit, with all the pertinent information at their fingertips, captured through a pre-go-live questionnaire, able to apply their clinical expertise expediently. The had a great user experience with little to no administrative overhead, few cancellations or no-shows.
Radiologists discovered that freedom more than 20 years ago when the technology allowed the remote reading of radiological reports. TeleRadiologists, who don’t have to be on camera, could work from the beach all day long if they wanted to.
The single-most important mindset for making telehealth work for clinicians is to focus on their experience as a user: enabling clinicians to practice on top of their license. Which means that most of the time they should be only doing the things only they can do. Which speaks right to the highest reason for burnout mentioned above.
Practicing Telehealth on Top of License
So how do we achieve this ideal state of care delivery via telehealth?
At the core is a focus on conscious and deliberate workflow design. This means to first reach absolute clarity on what needs to be done (what are the steps, what are the outputs, what are the outcomes). And then to decide who should actually be doing each of these tasks — based on their qualification.
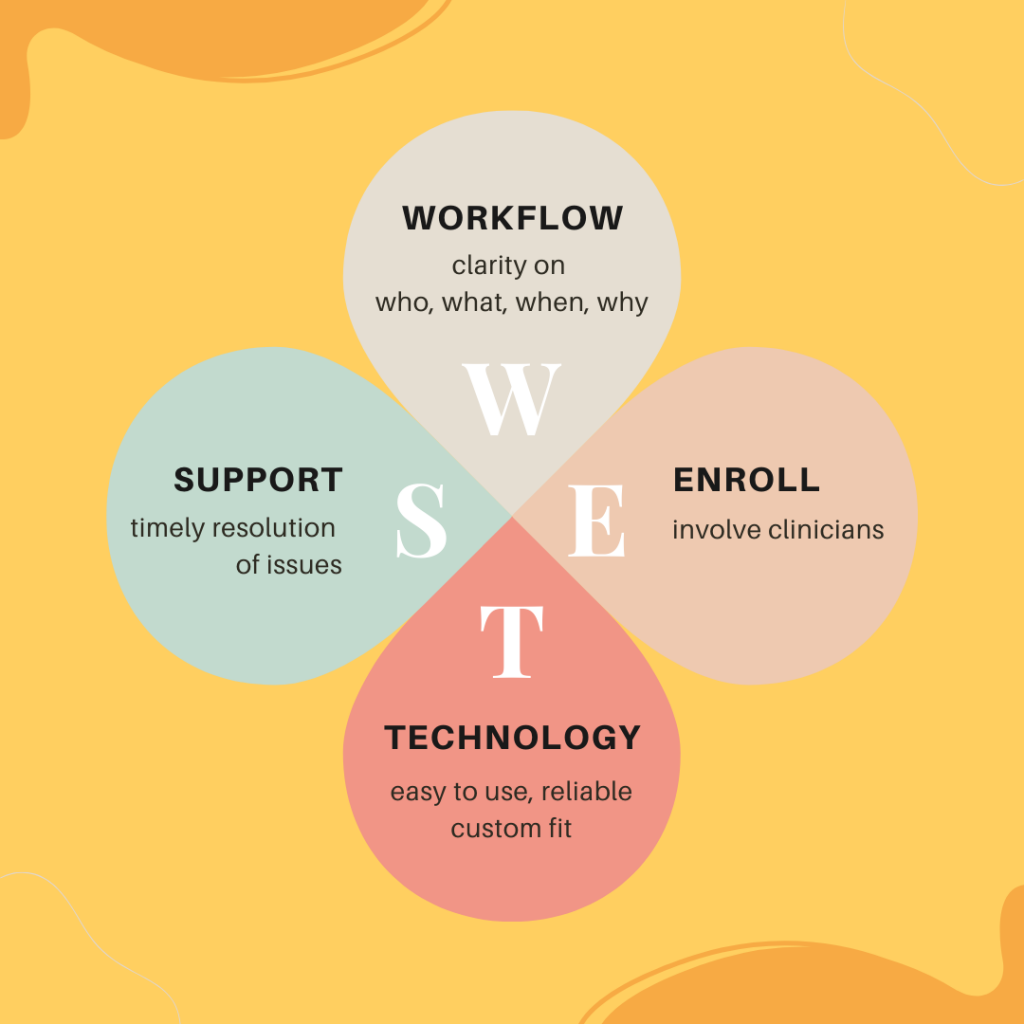
The second tactic is to involve and enroll clinicians in the design of their workflows, to integrate their ideas and feedback into the design of the overall solution, and to rigorously resolve the issues that reportedly plague them.
Next, the technology to deliver telehealth must be easy to use, reliable, and supportive of the clinicians’ mindset and workflow. The reason why surgeons have highly customized surgical tools is to increase their efficiency and efficacy. For the same reason, clinicians should have the best customized telehealth solution that supports the way they need to practice medicine.
Finally, there must be ongoing attentive telehealth support available to clinicians at all times. To use the analogy of the operating room again, surgeons use a multi-disciplinary team to get, at a moment’s notice, the tools and support they need (“Nurse, scalpel please”). Similarly, support needs to be available to clinicians when they encounter problems. And of course prevention (e.g., in the form of Telehealth TechChecks™) is the best cure!
Engaging Clinicians
When clinicians can focus on patient care, when clinicians are involved in the process of designing and optimizing “care delivery at a distance”, then the commitment by clinicians for telehealth is easy to come by.
When it comes to telehealth service, I always design for this Happy Day experience:
- The clinician checks their calendar for their next visit.
- With a single click the clinician is taken to the patients medical record.
- After the review of the patient’s chart, a single click brings them into their virtual exam room.
- Here, the patient is in the waiting room and the clinician “escorts” them in.
- They greet and move right into the conversation
- Quickly, the technology fades into the background — because the patient is using their technology well – audio, video, lighting, connectivity are all good.
- During the visit, the clinician charts his notes in the medical record and orders tests or prescriptions as needed.
- The patient leaves the virtual room, the physician leaves the virtual room — and is ready for the next patient.
Now, I’m not a clinician, but that sounds like a super easy experience that might just make it rewarding to be in healthcare.
Where is your organization struggling with clinician engagement? Where are you running into resistance, frustration, confusion or a lack of desire? Reach out to me to chat about some proven tactics to overcome these challenges.








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.








Leave A Comment