The problem in Healthcare is not the lack of innovation. It is the slow pace of innovation adoption.
I don’t think I can repeat this phrase often enough.
Given the fast pace of digital health innovation, a fast pace of innovation adoption should follow and this requires a new mindset, a new level of engagement of clinicians to embrace care enhanced by digital health innovation.
Having spent 12 years at the Mayo Clinic with its triple focus on research, education, and patient care, I fully appreciate that in healthcare cannot quickly throw new interventions on the frontlines to see what works. The potential negative consequences on human health and quality of life are simply much more severe than in retail or hospitality or transportation or manufacturing.
As a German engineer by birth and training, respectively, I also expect to make sure that the innovative digital health solution is usable, useful and that its touted benefits can be proven.
But that does not mean that we should take months or years to study, evaluate, and ponder novel solutions in an effort to be safe. Oftentimes it is people’s (and especially clinicians’) lack of experience with repeated change that leads to a healthy dose of skepticism about anything new and slows down progress.
The new mindsets below, the engineering-inspired systematic approach to launch a new digital health solution, and the primary topic of this article (“Engage your Clinicians!”) are all designed to minimize risk and increase the likelihood of success.
Mindset Adjustment | Adopt a New Mindset
Digital Health Innovation is available in many domains of the vast healthcare universe and for the purpose of clinician engagement the following guidance focuses on digital health innovations for diagnosis and treatment. While there are other digital innovations in healthcare, the clinician engagement matters most in these two domains.
Similarly to clinical intervention failure when the patient is not engaged in their care, the adoption of a digital health solution will fail if the clinicians are not engaged, if they are unable or unwilling to use the novel solution in their practice.
To succeed with the adoption of a digital health solution, executive and IT leaders must consciously make three key mindset shifts to ensure efficient, effective and everlasting success.
The first significant mindset shift is that the clinicians have to be front and center in the design, selection, and implementation process.
The second mindset shift for the adoption of digital health innovation is that the core focus should not be about the technology, but about the workflows. Specifically the care delivery workflow from the patient’s and the clinician’s perspective.
The third mindset shift is the realization that the implementation of a digital health solution is an organizational change management project, not a technology deployment initiative. Engaging all those impact by the changes is key to imminent and long-term success.
When pursuing the adoption of a digital health solution, here are the 5 steps where clinicians must be involved or lead the way:
- The decision to invest in a digital health solution.
- The design of the new workflows required by the new digital health solution.
- The review of solutions and selection of vendors.
- The definition of success criteria for a proof-of-concept validation.
- The design of the rollout, including training and communication.
Involved in the Digital Health Investment Decision
In today’s complex, cost-constrained world that is full of enticing digital health opportunities (with promising outcomes and/or returns) the leadership team (including the clinicians!) must ensure that the investment in the digital health solution (and the investment in its implementation!) is a good fit.
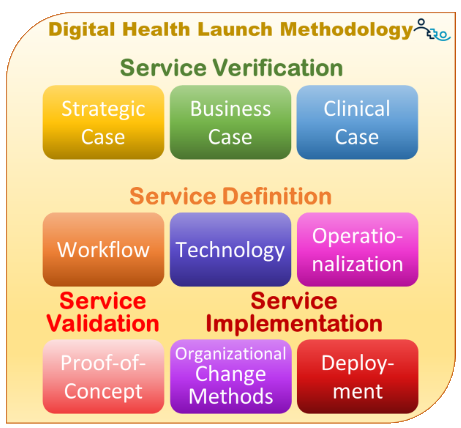
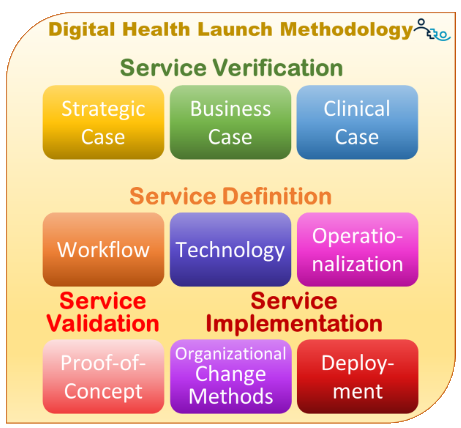
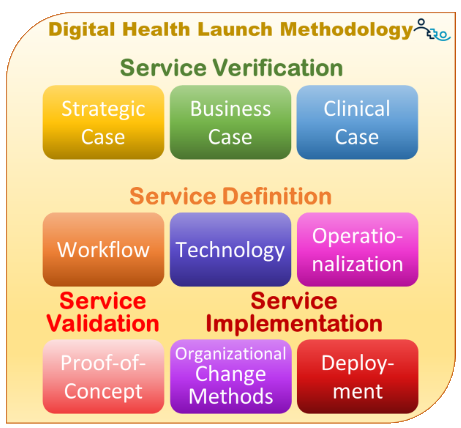
Preferably, before any further time is put towards the digital health solution (and definitely before meeting with any vendors!), three different “cases” should be prepared:
A Strategic Case that outlines how the solution will help achieve the organization’s current strategic priorities. This is usually primary in the purview of the CEO, but could also involve those leaders responsible for the relevant strategic priorities.
A Business Case that demonstrates the direct or indirect financial or non-financial benefits the organization expects to derive from the implementation of the solution.
A Clinical Case, prepared and reviewed by clinicians, that describes the solution’s expected clinical efficacy, e.g., anticipated increase in patient engagement or improved health outcomes.
Involved in the Workflow Design
Ultimately the delivery of healthcare is a series of service workflows, though many of them are not well-defined and just have organically grown over time. When it comes to reaping the benefits of the digital health solution, though, it is important to formally document what needs to be in place prior, during, and after the use of a digital solution.
Involving Clinicians at this stage is key (and it is even more important to complete this step before taking any further action toward selecting a solution). The integration of a digital health solution into the diagnosis or treatment of a patient requires the consent and the support of the clinicians because ultimately it will be them who will get patients to use the novel solution.
Since most clinicians are not experts in workflow design, the key is to present them with quick-to-absorb information about the steps prior to, during, and after applying the digital health solution on a patient case. Their involvement at this step is also crucial for the rollout, as they will need to advise on how to best train their peers on the use of the solution.
Involved in the Selection of Vendors
Armed with a clear understanding of what the organization expects from the solution strategically, financially, clinically, and workflow/user-experience wise, the clinician-led digital health solution selection & implementation team can now confidently approach the or multiple vendors to confirm whether the solution can meet their expectations – or where their expectations need to be adjusted to fit the reality of what is available.
This ideally starts with an education of the vendor about what the organization expects to accomplish with this solution which is followed by a presentation about the solution (and its benefits) and which of the organization’s objectives it can accomplish. Which is a very different vendor presentation than what you’d usually receive.
Involved in Identifying Assumptions and Success Criteria
If the organization is following a (highly recommended) “proof-of-concept” approach that is designed to validate assumptions and optimize the workflows and system configuration, involvement of clinicians in the design of the proof-of-concept is important to accurately represent the clinical (and patient) perspective.
Typically at this stage the team has sufficient information to make reasonable assumptions about the various aspects that are of relevance to the clinicians and can prepare an easy to review list of assumptions and success criteria for the proof-of-concept.
Involved in the Rollout Design
Finally, clinician involvement is key when designing the approach to deploy the solution beyond the proof-of-concept scope.
Through the clinician’s participation, the team can design the best approach to communicate with the broader clinical staff the benefits (and impact/implications) of the digital health solution — not only from a strategic and technical perspective, but also from a clinical point of view.
In addition, the review and feedback on the workflow and technology training for the clinicians (and patients) will be key for a successful rollout.
The Acceleration of Digital Health Innovation Adoption
Given the competitive threats by other industries entering the health care delivery market (think: Amazon Clinic, Albertsons, and Samsung) it is imperative for health systems, health centers and clinics to review their attitude towards digital health and invest in the acceleration of innovation adoption.
Just make sure this is not done in a techno-centric ivory tower, but involves the expertise of practicing clinicians. Because when patients are engaged in their care they get better health outcomes. And when clinicians are engaged in integrating digital health innovation, we get better care.








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.








