For years we’ve been using the well-established terms of Telehealth (“Delivering Care at a Distance”) and Telemedicine (“Practicing Medicine at a Distance”). In the middle of March 2020, right at the beginning of the worldwide social distancing due to Covid-19, we started introducing a third term: Remote Care, which we defined as “Connecting with Patients at a Distance”.
The good news was that in the early stage, as a stop gap measure, “connecting with patients” (primarily over the phone) was absolutely sufficient. Patients wanted to be reassured, directed to Covid-19 test sites, or simply needed a medication refill.
Now, that many patients have been seen in this “Remote Care” world the shortcomings of merely “connecting with patients” is becoming increasingly obvious.
The Unintended Consequences of Remote Care
According to a survey in partnership with the Primary Care Collaborative, many preventive care visits are going unfilled and much of America’s patients’ regular care is being deferred.
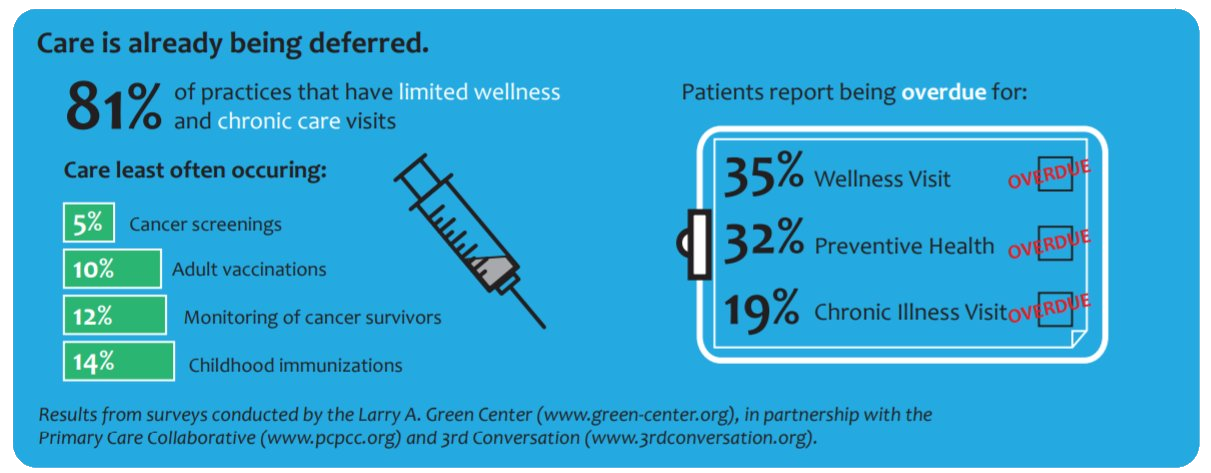
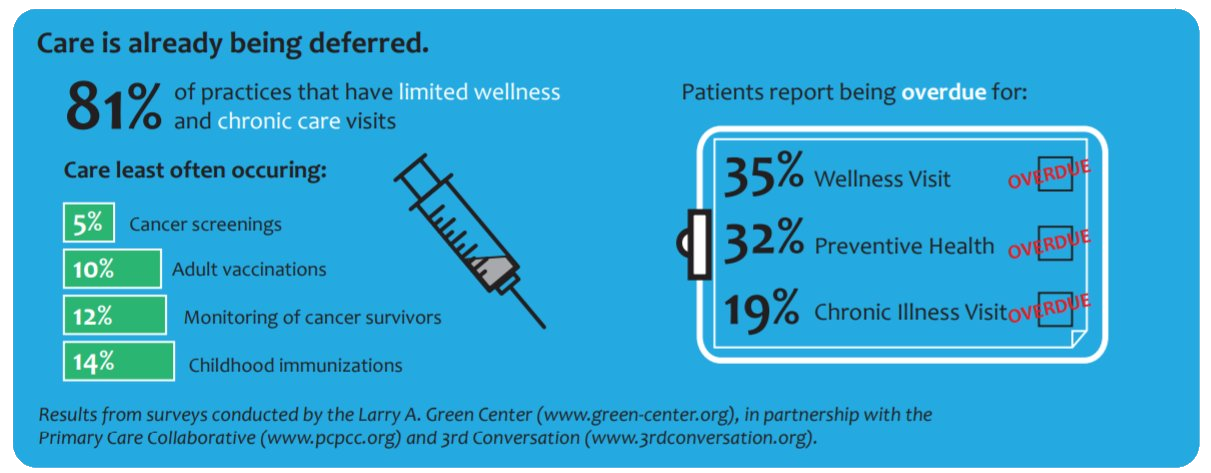
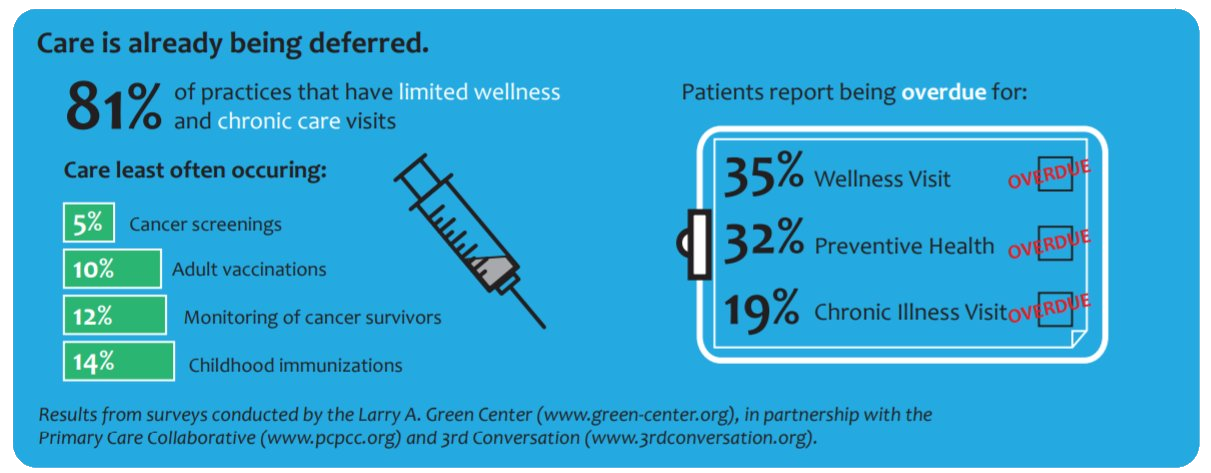
E.g., that is one in five patients (19%), who is not being seen for the proper treatment of their chronic illness, which could lead to higher acuity care. In the worst case scenario, this could even lead to the use of urgent and emergent care and/or a compromised immune system.
The two main reasons for the deferring of care, I venture, are that many people do not trust physician practices to keep them protected from Covid-19, so they do not want to be seen in person. Secondly, many clinicians do not feel adequately equipped or trained to conduct proper live audio/video visits, though oftentimes the patients’ lack of available technology or connectivity causes most of the problems.
Another main consequence is the increasing burnout by the physicians. For one, they are, like all of us, also dealing with their own, personal thoughts and emotions about the coronavirus, desiring to keep themselves and their loved ones and friends safe. Those personal stressors contribute to an ongoing anxiety in addition to the worries about their long-standing patient.
Operating in the Dark
Second, many physicians feel that they are increasingly operating in the dark, especially with their patient population with chronic diseases, even with live audio/video. What is primarily lacking to enable to delivery of “real telemedicine”, i.e, the real practicing of medicine, is the access to key vital signs and rudimentary test results such as blood panels or x-rays.
In a “virtual first” world, it can be very difficult to obtain key vital sign parameters such as blood pressure, weight or even pulse that are reliably accurate. While many patients may have consumer-grade devices that can obtain that data, the accuracy cannot be guaranteed (though it’s better than nothing).
Third, many physicians were “thrown” into telehealth in a matter of days with no proper training, badly configured equipment and not support processes. Numerous providers have told us that these days they are scheduling their patients’ follow-up appointments and helping patients troubleshoot technology problems.
The hidden victims of Covid-19
Currently the media, politicians and health systems of any size (who typically have a tendency to be inpatient focused) are mostly directing their resources and attention to the hospitalized Covid-19 patients.
The population that is being largely neglected are the tens of millions of patients that have 2 or more chronic diseases and that without an active care plan will decompensate over time and may very well become the secondary victims of Covid-19.
From Remote Care to Real Telemedicine
The success of many telemedicine-only companies is based on the limited focus of diseases they treat, mostly in the urgent care space, such as UTIs, pink eye or common colds. The success of many of the telehealth services I implemented over the last 10 years was based on the limited focus on follow-up visits, mental health, or triage-like assessments.
Most surveys I’ve seen at my clients or from associations like the Primary Care Collaborative indicate that 60% or more interactions between patients and clinicians occur using only the phone. While that is acceptable for the occasional question, it is not good practice of medicine for many patient conditions.
What is needed is first of all a systematic shift to live audio/video visits. Many agencies including the USDA and the FCC are offering numerous grants for the purchase of devices that could be acquired and deployed to those patients in your community that would stand to benefit most from easier, safe access to care via video on a tablet with 4G.
Secondly, further leveraging the grants, distributing vital sign monitors (even if they are not automatically connected) will go a long way to providing great care to many patients.
Finally, as I laid out in my article about the emerging Hybrid Care model, doing telemedicine well for those for whom it is adequate can easily free up more time slots for safe in person care.
Next Steps on the Road to Real Telemedicine
Applying for a grant is not an easy undertaking for most practices, though by teaming up with others in the community, will make such a process much easier.
The best options are to simply
- optimize your operational telemedicine service workflows
- train your physicians
- conduct Telemed TechChecks with your clients so they are “ready to go” for their first or next appointment
- through grants and other covid-19 funds, obtain the most basic vital sign devices and integrate them into your telemedicine visits
With those four steps implemented, you will be much closer to truly enabling your clinicians to practice real medicine at a distance.








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.





Leave A Comment