It is now pretty clear to most of us, that social distancing (whether mandated or voluntary) is here to stay for many months. Especially those patients at a higher risk of a coronavirus infection causing harm to them, will be very likely to remain at home as much and as long as possible.
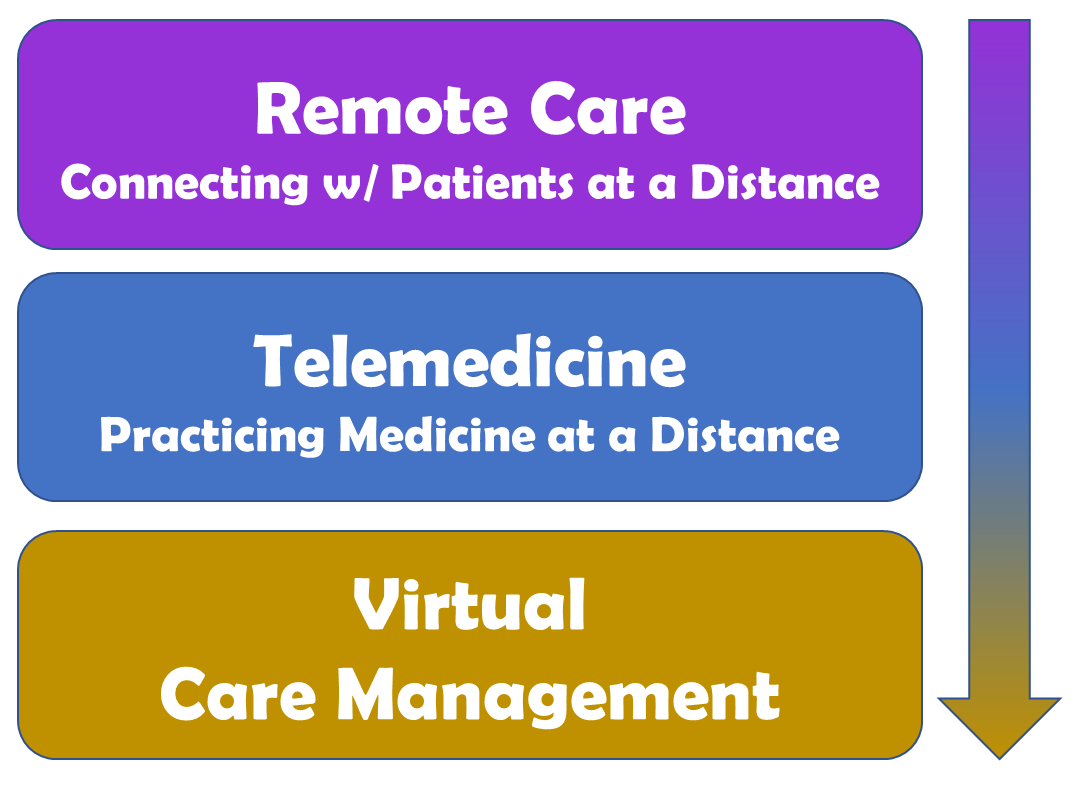
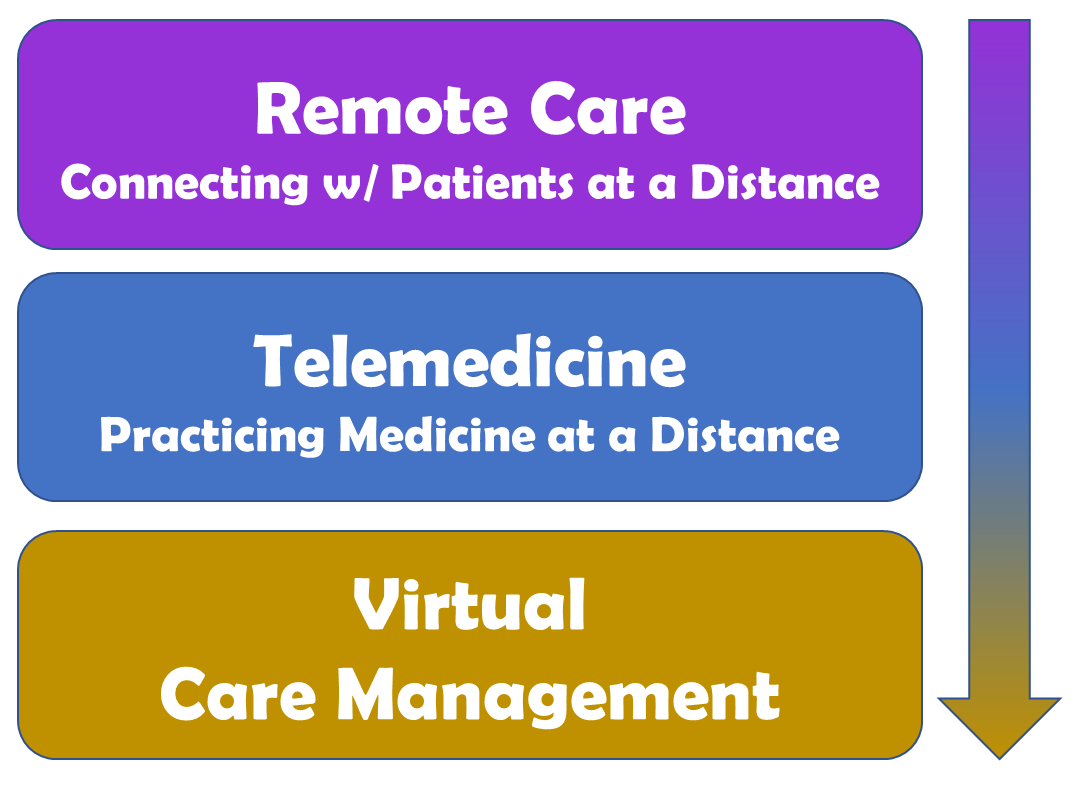
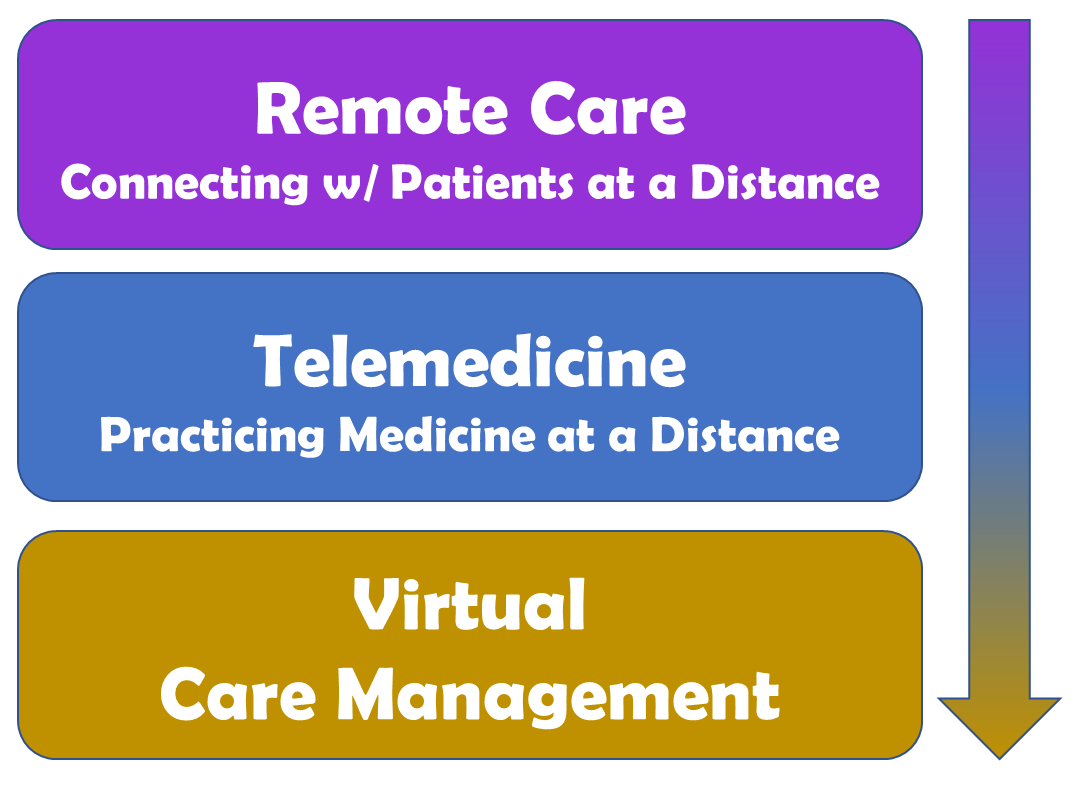
In the early days of our healthcare systems’ response to the Coronavirus in the middle of March 2020, many organizations were rapidly standing up hastily acquired technical capabilities to connect with patients at a distance, a.k.a. “Remote Care”. That is to say that the capabilities of these services for some clinician/patient interactions fell short of “Telemedicine” which we define as “practicing medicine at a distance”.
While payors refer to this type of care enabled by live audio/video as “telemedicine”, most healthcare organizations’ initial (or current) offerings merely facilitated a conversation with the patient, with varying degrees of success to truly “practice medicine”.
Which is exactly what was needed in the early days of our response to social distancing — the ability to quickly connect with patients to “see” how they were doing and help them with their imminent challenges, medication refills, etc.
Now that we’re over 4 weeks into social distancing in most parts of the country, we are realizing that social distancing will stay with us for a long time until we have a vaccine, treatment, and sufficient testing.
Which means that the mindset of healthcare administrators and clinical leaders in healthcare delivery organizations needs to focus now on planning and preparing for how we can care for those patients that need access to care but who can’t or don’t want to come into the clinic in months to come.
Or said in other words: to focus on quickly evolving from “Remote Care” to “Practicing Medicine at a Distance” and then to Virtual Care Management.
In US healthcare, we rely for our diagnosis and evaluation of treatment efficacy very heavily on data such as the patient’s most recent vitals and the results of tests such as labs, x-rays or EKGs. Any of those are these days very difficult to obtain.
While a secure, live audio/video telehealth visit can provide much more information than a simple phone call or text messaging, its ability to collect actionable data from the patient about the patient is still very limited.
Before considering technical solutions, what is mostly needed is a mindset shift away from “transactional” visits week after week to a more mid- and long-term oriented approach to keeping shelter-in-place patients safe. What is furthermore needed is access to scalable, affordable technical solutions to acquire the data that clinicians, rightfully, are so accustomed to obtaining.
Tailored Solutions
One of the 6 common misconceptions about telehealth is that “one size fits all”, that one telehealth solution can address all the needs of all clinicians for all patients. That belief is a fallacy often promoted by IT which sees it as its role to limit the number of technical solutions it has to license and support.
What is needed is a collection, an arsenal of fine-tuned service offerings readily at the disposal of clinicians, that can bring the care to the broad spectrum of patient populations your organization, your clinicians are serving.
The populations that over the next months will most greatly benefit from telemedicine services that are geared toward them include the chronically ill, the high utilizers, and those affected by the deferred elective surgeries.
Each of these populations — and subsets within each population — will require different solutions. For diabetics we want to get reliable blood sugar readings. For those with CHF or COPD, having good blood pressure and even pulse ox data would greatly increase the clinicians ability to “practice medicine at a distance”. Patients with deferred hip replacements need a different level of care than those waiting for a carpal tunnel repair or an ablation/cardioversion.
Another driver for the need of “Virtual Care Management” is to take the concepts of population health management and the patient-centered medical home into the new “at a distance” world as well.
Transition to Virtual Care Management
So what is an organization to do? Well, first things first.
To build clinicians’ confidence in telemedicine, an organization must first ensure that clinicians are highly satisfied with the processes, the policies, and the technology. You need to evolve from Remote Care (“connecting with patients”) to telemedicine (“practicing medicine”) by using creative, innovative approaches and, oftentimes, community resources to overcome the limitations of care at a distance.
Then, and only then, can you bring multi-disciplinary teams together to identify ways to treat your most vulnerable, most sick, and most at-risk populations safely and efficaciously at a distance. And set the stage to evolve from Remote Care to Virtual Care Management.








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.






Leave A Comment