For the last 17 years I’ve been an adamant fan and promoter of telehealth, predicting that over 80% of patients’ interactions with healthcare providers could be delivered “at a distance”. And it’s only 80% because I have also learned that telehealth, in its most common form as a live audio/video conversation, has its limitations to deliver extraordinary care.
On the obvious side, telehealth is not going to replace hands-on exams, such as palpations of the stomach. Similarly, dental exams are trickier, too, though for an initial assessment and triage, telemedicine does suffice.
What’s less obvious are the limitations of telemedicine for the longer term virtual care of patients, mainly because of healthcare’s rightful reliance on the aptly named vital signs (pun intended).
One of my favorite quotes is that of Don Berwick, founder of the Institute of Healthcare Improvement, IHI: “Every system is perfectly designed to get the results it gets.” What that quote has taught me over the years is that in order to achieve different, better outcomes, one must change the system: the processes, the workflows, the technology, the incentives, the rewards, the policies, the training, etc.
In the rush into telehealth, though, many elements of the system were not changed, were not optimized for the delivery of care at a distance.
The Rush into Telehealth
When healthcare rushed into a full-throttle rollout of telehealth (albeit a lot of it still hiding as “telephonic”-only telehealth), it was definitely the right thing to do: give patients, who need care or medical advice, access to medical professionals, preferably over video.
Going over test results? Great.
Ordering an interim refill? Got it.
Discussing the implications of delayed surgery? Doable.
Triaging your best care route with Covid-like symptoms? Perfect fit.
Where video-based telemedicine is definitely a great fit is in the behavioral health space – and has been for years. Counselling over video or the phone, including the prescription refills, offers new opportunities for continuity of care, reducing no-shows and improving engagement.
But when we enter the primary care and specialty realm of healthcare, going only by words, by live video of facial expressions and body language is not sufficient clinically in the long run. Ultimately, clinicians rely on access to good data about the clients conditions to make good care decision.
An Engineer’s Care Process
My 20 years of working with physicians has taught me that I’m oversimplifying the following (and I mean no disrespect), but today’s modern primary care and specialty care medicine is most often a simple sequence:
- assessing the patient’s condition and history
- ordering tests to confirm suspicions or hypotheses
- analyzing and reviewing the results
- developing and discussing a care plan
- following and monitoring the care plan (including in some cases invasive procedures)
While Telehealth is great for steps 1, 3, 4, and 5 (except the invasive part), there are limitations in the assessment of the patient’s condition in step 1 and assessment of the difference the care plan makes in step 5.
As Covid-directed physical distancing continues, what’s mostly lacking is an accurate insight into the patient’s key vital signs – those that typically would be acquired by the clinic staff in preparation for a patient’s visit. For a few visits it was definitely acceptable to “fly in the dark” and go by the patient’s vital signs’ past performance (which, as we know from the financial literature fine print, is no prediction for future performance). But now, as the health crisis lingers, we need better solutions that still keep patients and staff safe.
What’s also missing, regarding step 2, is the coronavirus-safe access to frequent tests such as lab work and imaging. While solutions available for the home exist, the logistics of deploying them to a patient’s home make most innovative solutions impractical for scaling.
Preparing a Patient for a Telemedicine Visit
Most healthcare organizations that jumped newly into telehealth in March 2020 merely gave the clinicians a video chat tool (or permission to just use the phone) and told ‘em to “go do telehealth”. What was lacking was the whole set of workflows for the scheduling, pre-visit, and post-visit steps that typically make up a complete visit experience in the in-person-care world.
Telemedicine TechCheck
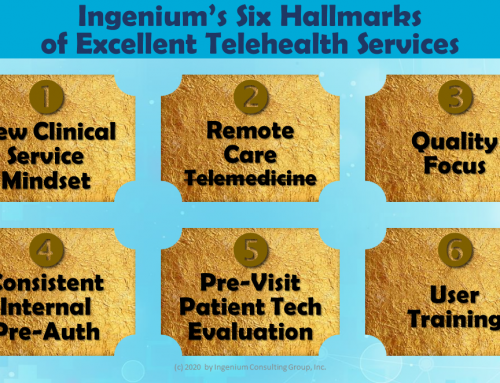
One of the key hallmarks of successful “direct-to-consumer bring-your-own-device” telemedicine that we are practicing during this health crisis is the Telemedicine TechCheck, preferably conducted at the time of scheduling. I have written extensively about his unique but largely unknown practice here, here and here.
While a Telemedicine TechCheck can ensure a satisfying experience regarding the technical aspects of the telehealth visit, the clinical quality of the visit requires more than just a good connection. In addition to access to the patient’s medical history, clinicians also need to have access to a most recent set of vital signs.
TeleRooming



Thus some of our clients have now started calling patients on the morning of the telehealth visit to either collect a most recent set of vital signs or to remind them to take their measurements and share them with the physician. Oftentimes these visits, especially when conducted over video, can be excellently used to review their current medications.
A Learning Experience
For me, the rollout of telehealth has for a long time been mostly an exercise in managing the change in how clinic staff work. The Covid-necessitated shift to DTC BYOD telemedicine now also requires us to focus on helping patients to change the way they not only receive care, but how they schedule their care and how to prepare for a visit.
And guess what – after the physician ends the video call, there’s a whole new set of virtual care process steps to be defined. But that’s an article for another day.








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.




Leave A Comment