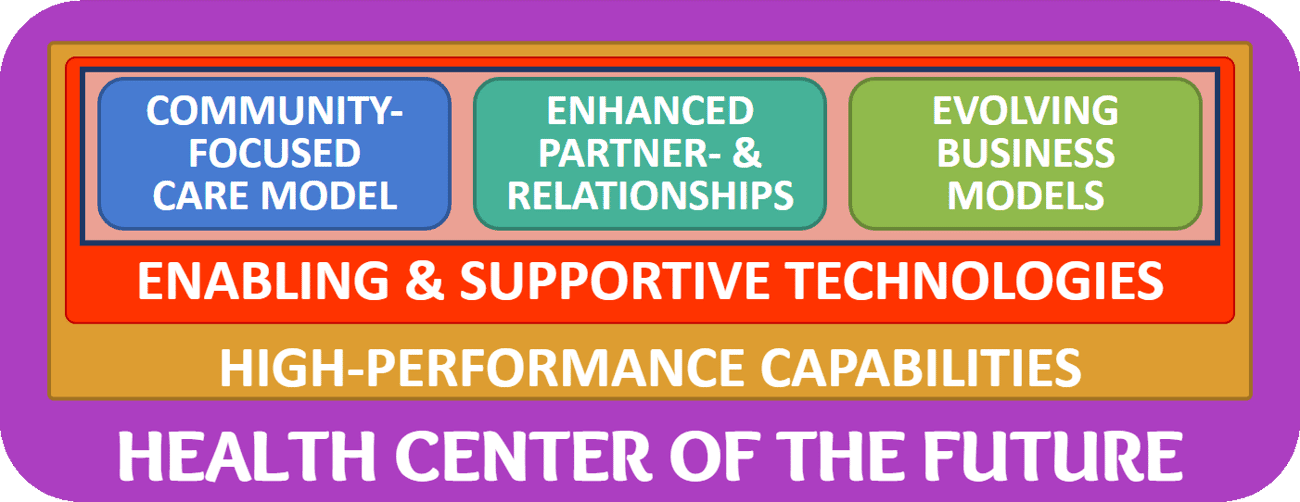
The Framework for the Health Center of the Future provides a simple yet comprehensive roadmap for community health centers to prepare for a sustainable future.
At the core of the framework are the three elements of a health center’s engine (a community-focused care model), the fuel (evolving business models) and the infrastructure (enhanced partnerships).
The successful transformation to and successful operation of new care models, new business models, and new partnerships requires a set of critical, high-performance capabilities that we’ll describe in more detail in a future article.
Today, we’ll be diving deeper into the world of “enabling and supportive technologies”, expanding on the overview of the “World of Health Center Technologies” and the “Digital Health Taxonomy” previously covered.





Principles of Health Technology Adoption
To use supportive and enabling technologies to create the Community Health Center of the Future, health centers have to recognize barriers to technology adoption and be ready to apply the strategies to overcome those barriers.
The most commonly encountered barriers to technology adoption in healthcare are:
Confusion — clinicians and staff do not fully understand why a particular technology is important to the organization’s success. Oftentimes they are not aware of how the technology will help the organization’s key objectives – and may not even be aware of the strategic goals themselves.
Resistance — an outright refusal or, more commonly, clinicians’ and staff’s passive aggressive refusal to use the technology by. This barrier clearly originates from a lack of desire which is related to not fully understanding or not agreeing with the strategic goals, or how the technical solution can help achieve those.
Reluctance — the hesitation to use a technology mostly out of fear to look foolish or break something. The origins for this are often due to a lack of familiarity with the technology, originating from insufficient training and inadequate or inaccessible, timely support.
Frustration — irritation stemming from technology with a poor user experience, a mismatched or poorly defined workflow, or lack of adequate training and support.
Backsliding — the slow reversal to doing things “the old ways”, pursuing the “path of last resistance” which oftentimes are the ruts of familiarity.
Looking at this list, the strategies to overcoming these barriers to technology adoption are pretty straightforward:
#1. Explain the Why: Leadership must clearly communicate the “why” behind the technology and explain how the technology addresses key organizational goals. E.g., “We are investing in RPM for our diabetic population as part of our value-based contract to better engage patients in their care and improve the management of their condition.”
#2. Appeal to the Emotions: While the “why” must address the “logic” behind the use of the technology, communication must also make an emotional appeal to clinicians and staff, explaining the rationale behind the use. Logic makes people think, but emotions jumpstarts people into action. E.g., “Our patients deserve access to our excellent care which is why we are investing in making access to care via telehealth as easy and convenient as possible.”
#3. Involve Key Stakeholders: In addition to communication, involving key stakeholders early on in the technology selection and implementation process ensures ownership and buy-in that minimizes confusion and resistance. E.g., “We would like to tap into your experience and leverage your input to select the best solution to launch our virtual scribing initiative.”
#4. Focus on Workflow: Technology in healthcare never exists in a vacuum. Technology is always part of an overall workflow – either to deliver care (including diagnosis, care planning, and care plan execution) or the dozens of “auxiliary” processes related to the core care processes. To avoid most of the above barriers, focusing on a joint design by all users of the desired workflow that supports the technology (before, during, and after) is the most effective strategy.
#5: Train comprehensively and adequately: To avoid frustration and reluctance, training on (1) the “why” behind the technology, (2) the workflows, (3) the policies, (4) operating the technology, and (5) getting support is key to successful adoption of new technologies.
#6: Establish launch, operational, and technical support: While most technologies do not require a significant level of support, many technologies disrupt the way health centers have delivered care and therefore require support, especially at the operational level. Technical support is mostly a given, but focusing on operational support that tracks and resolves issues and provides just-in-time training is key to success.
#7: Provide Accountability: One of the most common reasons why new ways of doing things don’t stick (and thereby rob the organization of reaping the benefits for which the change was initiated) is the lack of accountability. The most common reason is the lack of executive insight as to the utilization and actual performance (and potential savings) of the new technology. Establishing, measuring, monitoring and acting on key performance indicators (KPIs) is key to overcoming barriers to technology adoption.
Don’t Put the Horse Behind the Cart
Another common reason why technology adoption often falls short of the expected potential is the way that technology solutions are often selected. From my observation of almost 25 years in healthcare, too many healthcare organizations are victims of the “horse behind the cart” trap. Yes, I’m butchering the idiom (and I’m using my German engineering background as my excuse).
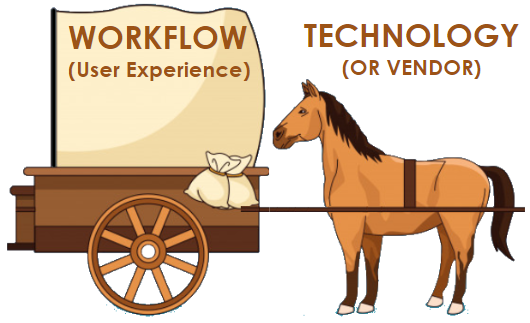
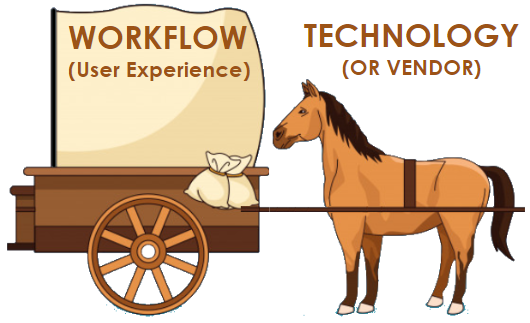
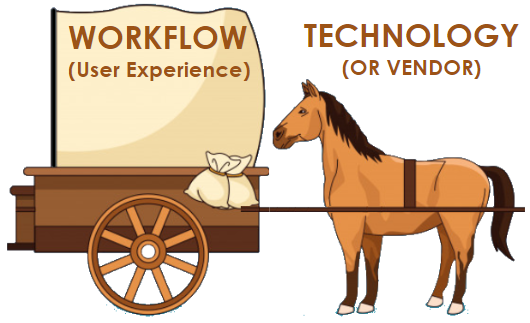
What I mean is that more often than not either clinicians or frequently also Health IT leaders make the selection on what technology they want (the horse), before they gain clarity on what the solution actually should be doing, especially in terms of the workflow or the user experience.
Clinicians fall prey to the shiny object syndrome, focusing on superbly cool features; IT staff tend to focus on the lowest administrative overhead to bring in a vendor or on the tightest integration with existing technologies.
Yet few teams develop a solution/vendor-independent catalog of specific requirements as to what features, performance, and experience would be desirable. Since oftentimes these individuals charged with finding a solution “don’t know what they don’t know” the best starting point seemingly are the sales presentations by vendors.
A Business Case for Technology Solutions
When it comes to finding suitable technologies on your journey toward becoming a health center of the future, the first step is to clearly identify which of the core elements — care model, business model, or relationships — the technology is going to support.
There are plenty innovative technology solutions available — the secret to success lies in first gaining clarity as to what you want to accomplish, and the selecting the technology that helps your organization to achieve that goal.
Next week, I’ll provide a few examples of technology solutions that can support new care models, new business models or new relationships.
Is your health center considering new technologies? How about a brief conversation about the underlying clinical and business case? Reach out to schedule at time.










To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.








