For Community Health Centers to chart a course for the future, last week we shared a Framework for the Health Center of the Future developed by a multidisciplinary team brought together by the Mid-Atlantic Telehealth Resource Center (MATRC).
At the core of the framework are evolving business models that leverage enhanced partner- and relationships and a community-focused care model.





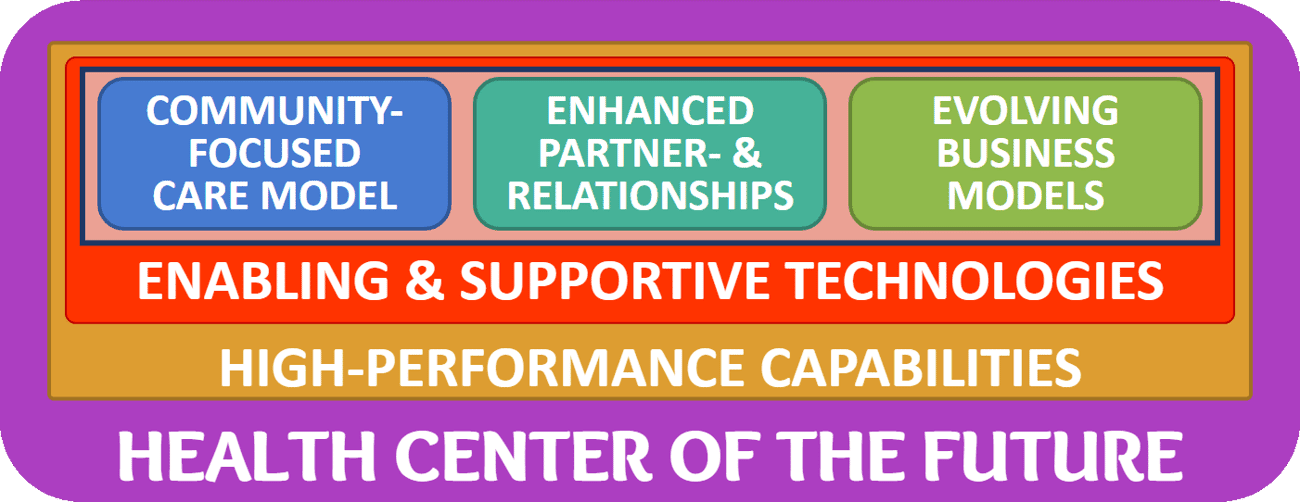
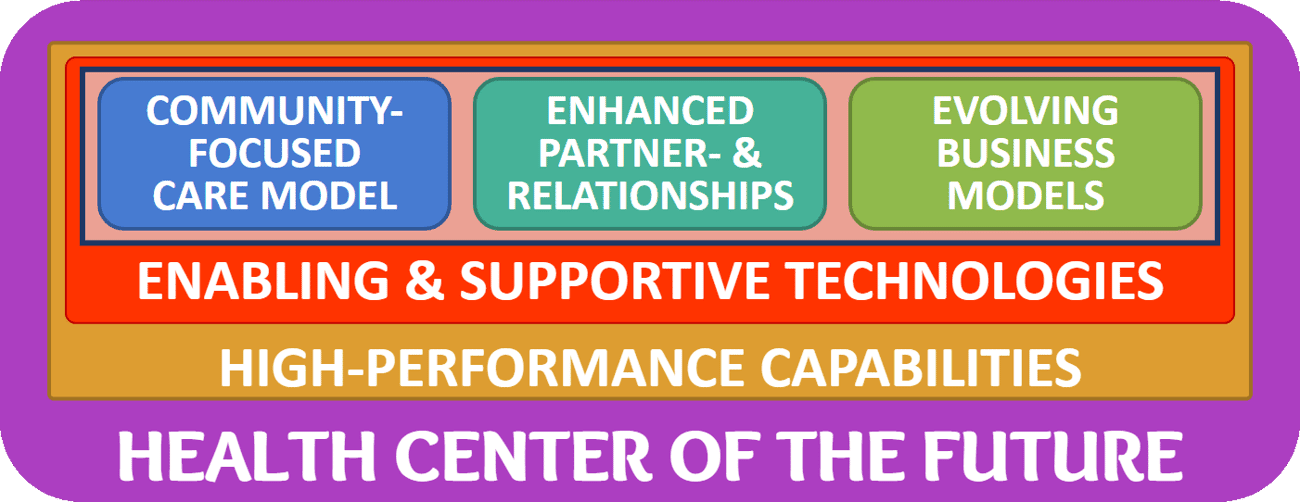
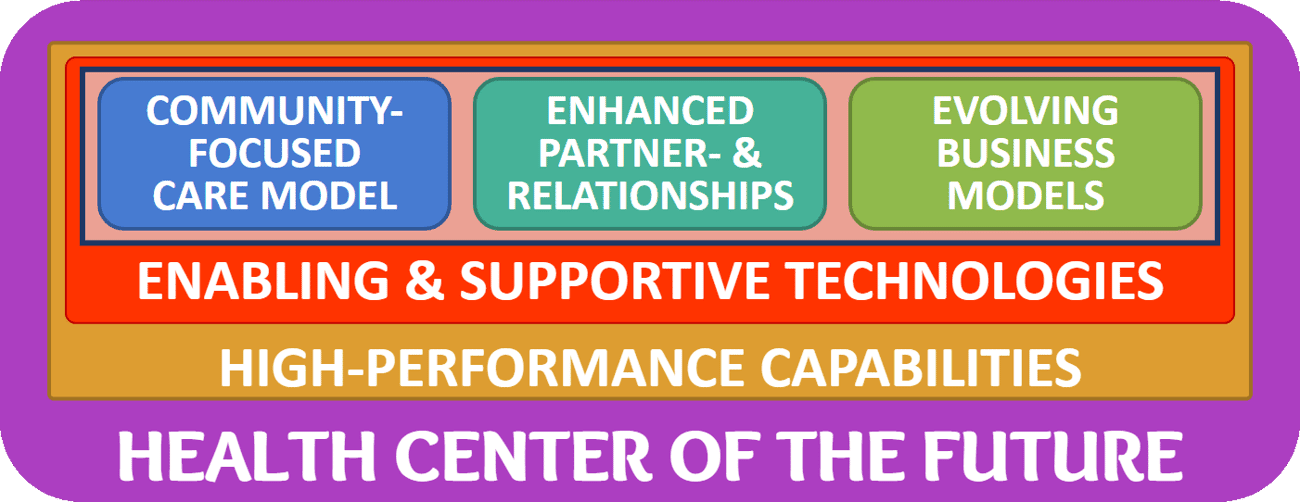
While this multifaceted approach can provide the engine, fuel, and infrastructure for a successful health center, by themselves they do not constitute a blueprint for the future. It is only through the pursuit of two additional key concepts that health centers can transform to be ready for the future: Enabling and Supportive Technologies and High-Performance Capabilities.
In today’s article, we’ll cover the first of these two:
Enabling and Supportive Technologies
For many years, Community Health Centers have used “supportive technologies” to automate or scale their core operations. These technologies, such as the EHR or revenue cycle management solutions, today represent table stakes in healthcare that no longer are considered modern or innovative.
For too long, Community Health Centers have treated the investment in and the support of technology like a utility or custodial services, thereby missing the immense possibilities to create clinical, financial, or strategic advantages.
As a fundamental mindset shift, leaders taking their organizations on the journey to become a Community Health Center of the Future must clearly declare and treat technology as a gift that enables the implementation of innovative business models, that creates opportunities for better partner- and relationships, and opens the door to a novel community-focused care model.
Technology can no longer be shunned as “the necessary evil” to support health center’s operations. Rather, technology should be revered as the opener to unprecedented opportunities, as the enabler of new business and new care models.
Through technology, Community Health Centers can offer novel approaches that improve health outcomes, create new revenue streams, increase clinician productivity, attract new patients, enable partnerships with employers and schools, etc.
The World of Health Center Technologies
To explore and evaluate a suitable set of technologies to become a Health Center of the Future, it is helpful to understand the vast landscape of health technologies through segmentation.
In its simplest form, there are two basic sets of healthcare technologies that healthcare organizations employ: Practice Technology and Patient Technology.
Practice Technology helps to run the practice and its operations. This includes the phone system, the scheduling system, the email system, the billing system, etc. While some of it impacts the patient indirectly or sometimes even directly, the primary purpose of practice technology is to improve the efficiency of a health center’s operations.
Patient Technology is intended to benefit the patient directly or indirectly. Many of the technical innovations over the past 15 years have focused on patient-facing and patient-affecting solutions.
While much efficiency and cost savings can be gained from optimizing the practice, the true game changing opportunities lie in the domain of Patient Technology. When we look at the three core elements of the Health Center of the Future, it is mostly that domain that can offer the greatest preparation for the future.
A Digital Health Taxonomy
A large portion of today’s technologies that captivate the interest of community health center leaders is the domain of “Digital Health”.
To understand the potential of what Digital Health can do to enable the various elements of the “Health Center of the Future”, we first must differentiate the various “flavors” of digital health.
The following diagram is a simplified, hierarchical taxonomy of the various digital health terms that are in use today. As a starting point to understanding the various elements, here are brief definitions of the various terms depicted.
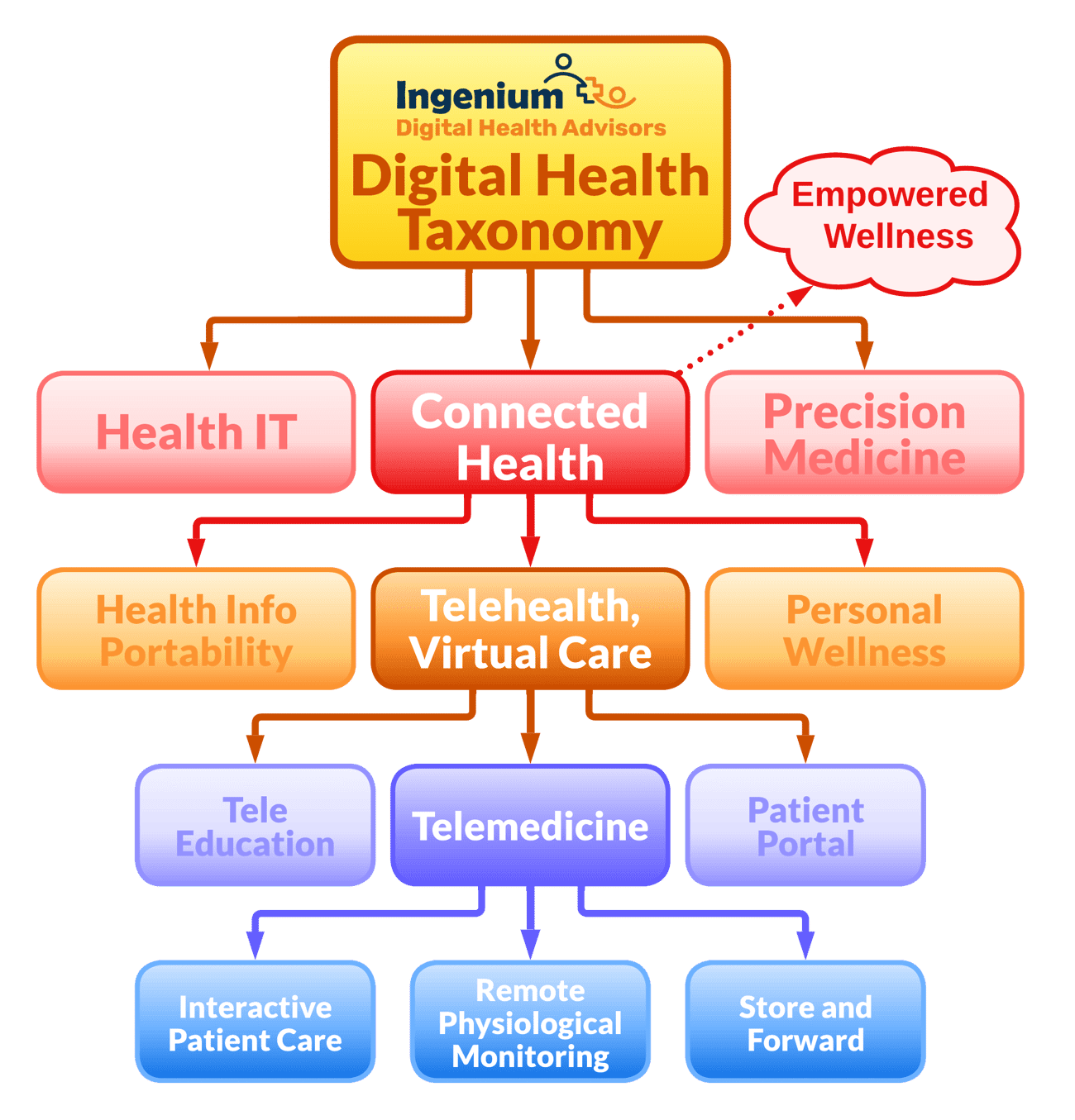
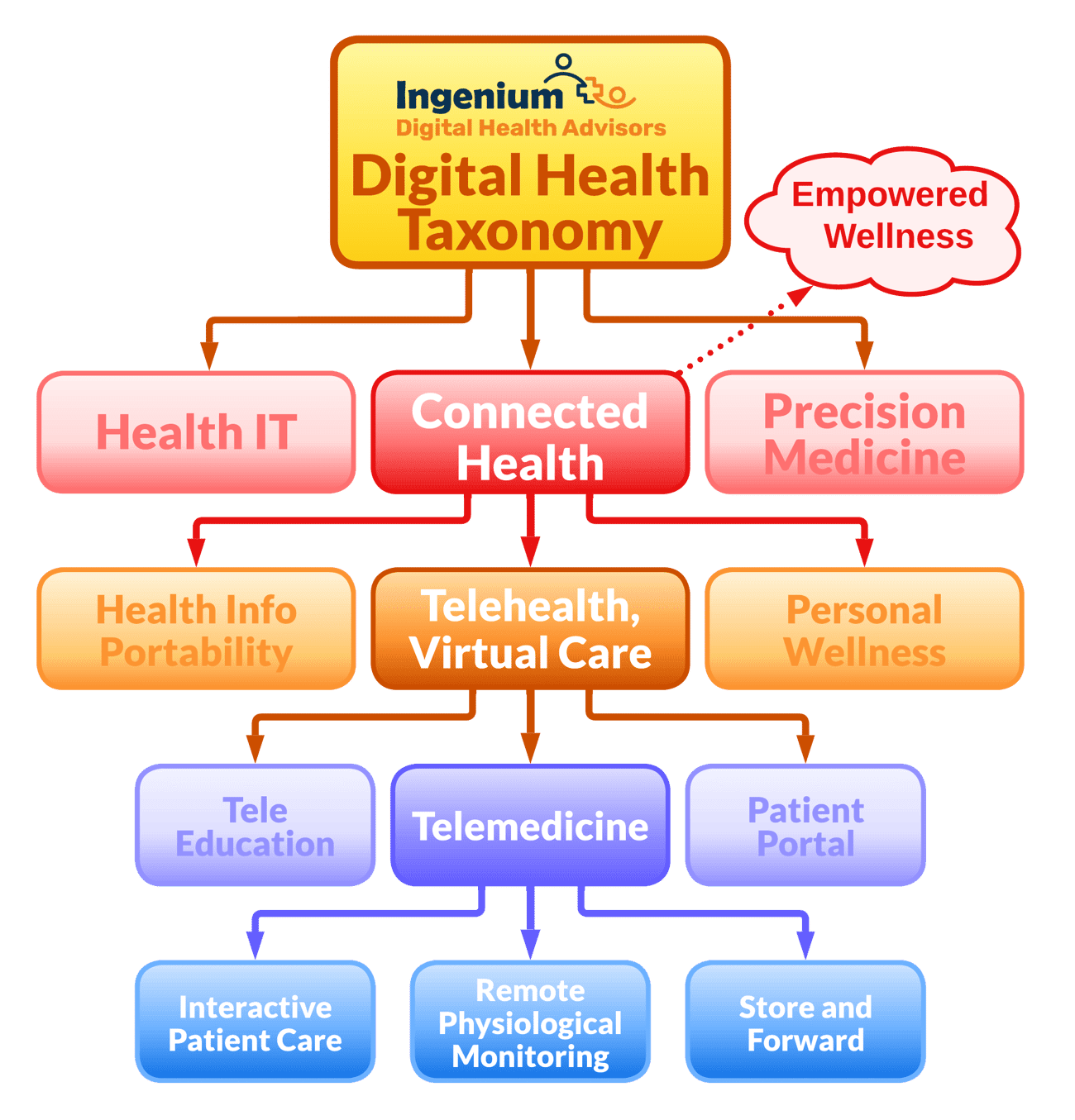
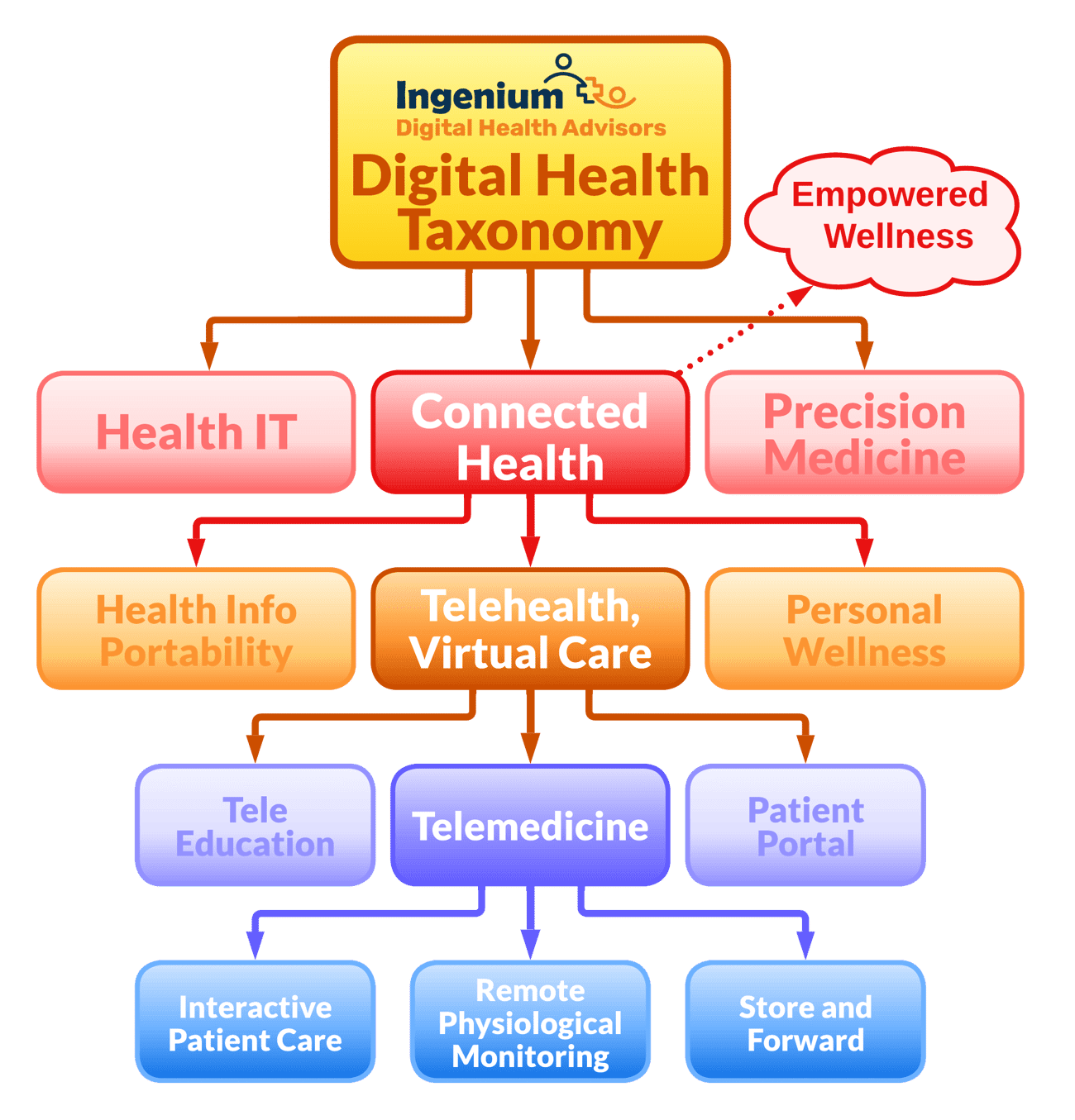
Digital Health
Digital Health is the overarching term for all technologies used in healthcare. Specifically for healthcare delivery organizations such as community health centers, digital health is the use of technology to improve the efficiency and efficacy of care decisions, care delivery, and ancillary healthcare processes.
Health IT
The traditional collection of healthcare technologies, such as electronic health records, clinical decision support systems, enterprise image management, revenue cycle management solutions, etc. Most of the practice technologies fall under this umbrella.
Precision Medicine
Precision Medicine (also sometimes referred to as individualized or personalized medicine) are technologies that enable the tailoring of treatment to the patient’s unique specific biology. Examples include custom-fabricated implants, T-cell treatment, or 3D bioprinting.
Connected Health
Connected Health is a vision for Empowered Wellness. It transcends episodic care and takes a more comprehensive, long-term view. In a Connected Health world, providers, caregivers and patients have access to the right information at the right time in the right form to make better decisions.
Connected Health not only connects providers to patients (as in Telehealth), but also consolidates health-relevant information from multiple sources inside and outside the system, to inform decision making. Ultimately, better outcomes are about better decision making — including the decisions patients make.
Connected Health is the vision of knowledge-empowered care: A fully-connected healthcare system where patients and providers can easily connect with one another regardless of their locations — doctors connecting with patients, generalists connecting with specialists, and caregivers connecting with loved ones. It’s a system where all pertinent information (patient condition, health history, treatment options) is readily available to facilitate quality decisions.
The step from Telehealth to Connected Health is a big one and an evolution long in the making. No longer will technology be driving care (as did telecommunications technology), but rather the prefix “connected” shifts the focus to relationships: closeness between people, interactions among systems, and connections between bits of information (soon made more accessible through AI).
Telehealth (or Virtual Care)
While there are fancier and longer definitions out there, at its core, Telehealth is simply “delivering care at a distance”. Telehealth is technology-enabled communication with patients who are not right next to the doctor. This includes education of patients at a distance (TeleEducation) as well as giving patients access to a variety of self-service options, such as reviewing clinical notes, scheduling appointments, paying bills, or refilling prescriptions through a Patient Portal.
In most contexts, Virtual Care is synonymous with Telehealth, though that term was more frequently used by the media to focus on video visits and telephonic care.
Telemedicine
While I often use the terms Telehealth and Telemedicine interchangeably, I still prefer using Telehealth for the overarching notion of care at a distance, with telemedicine being a subset focused on “practicing medicine at a distance” to describe the interactions of clinicians with patients, including examination, assessment, consultation, and treatment.
At the lowest level of the taxonomy, Telemedicine breaks down into three common subsets:
Interactive Patient Care, which includes video visits, tele exams, but also asynchronous secure texting. I.e., any technology-enabled bi-directional communication between clinicians for the purpose of delivering patient care.
Remote Physiological Monitoring, the continual and periodic collection and transmission of key vital signs including weight, blood pressure, pulse, oxygen saturation, temperature, or blood glucose.
Store & Forward, the long-time tried and true transmission of key data about the patients condition for future review by a clinician, ranging from electronically transmitted EKGs (including via fax) to photographs of skin lesions or other visual or audio-visual recordings.
For more information on the digital health taxonomy, please see my white paper on the Ingenium Digital Health Taxonomy or articles on the various aspects of Digital Health.
Beyond the Telehealth Terminology
While an understanding of the various technologies involved in enabling and supporting the Community Health Center of the Future is important, it is by itself not sufficient.
In future installments in this series we will explore
-
Guidance on creating a culture of accelerated adoption of Digital Innovation to create and maintain competitive relevance in this world of fast-paced technology innovation.
-
The importance of adopting a mindset of Information Management to enable data-driven decision making and management by facts.
-
A systematic approach to selecting, validating, implementing and supporting technologies, including governance, change management, process & workflow design, training, etc.
-
Illustrative examples on using technology to enable community-focused care models, enhanced partner- and relationships, and innovative business models.
Are you or is someone in your network working in a Community Health Center?
Then reach out to me for more information about the current “Health Center of the Future Training” initiative by the National Association of Community Health Centers (NACHC).










To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.