While Community Health Centers have long used technology, mostly for managing operations and the revenue cycle, many CHCs are only just now beginning to employ more “modern” technologies such as data analytics and, mostly fueled by the Covid-19 health crisis, video visits. Many health centers also had in recent years brief, grant-enabled flirtations with Remote Physiological Monitoring, though in most organizations these programs rarely went beyond the initial trials.
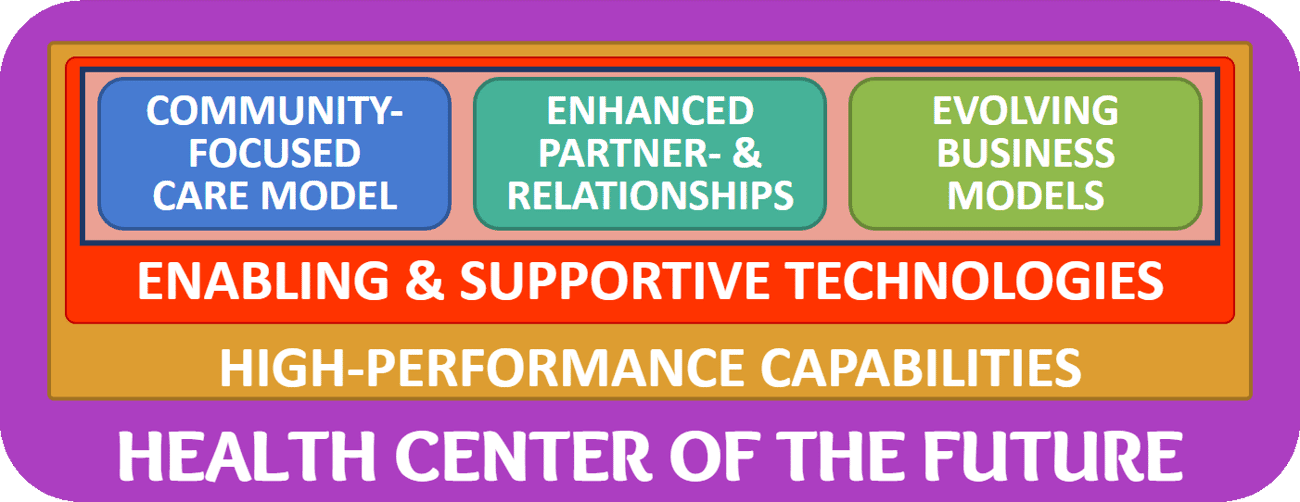
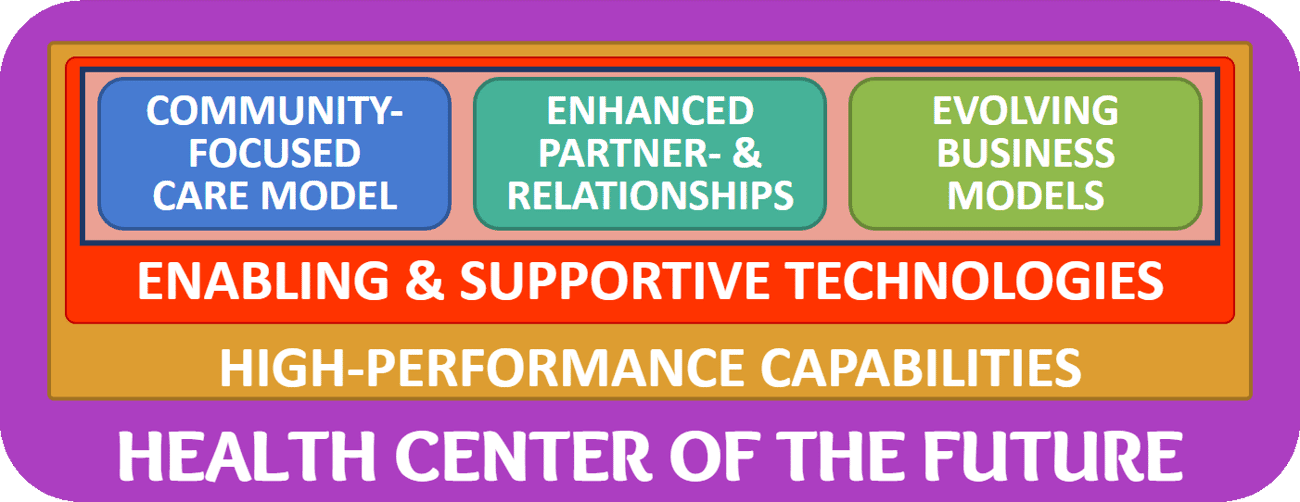
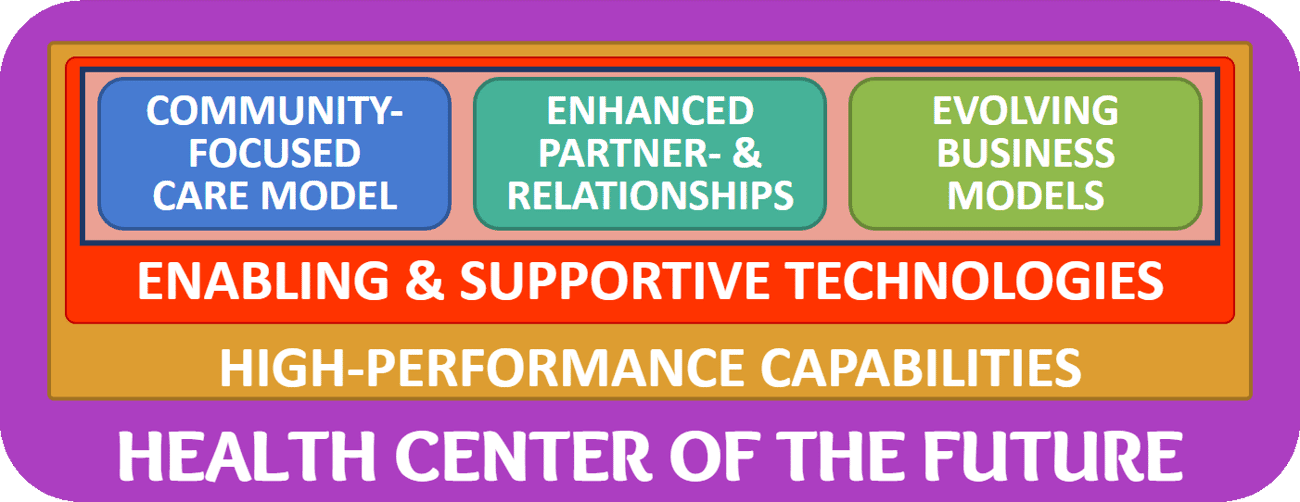
To prepare a Community Health Center for the future, leaders must realize that technologies, especially digital health technologies, are the key to enabling and supporting new care models (and new care delivery modalities), opening the door to new kinds of partnerships and business models, as the core of our framework depicts:





Since many leaders’ focus quickly turns to technology as the first and most important ingredient to prepare a health center for the future, it is essential to emphatically emphasize that based on the collective expertise of all involved in the development of the framework, the consensus was clear:
Technologies are only a means to an end and by themselves cannot create or ensure a Community Health Center’s future.
Technologies can, however, create novel opportunities that improve outcomes, create new revenue streams, increase clinician productivity, attract new patients, enable partnerships with employers and schools, etc.,
The Care Model of the Future
While it is beyond the scope of these articles (and even beyond the scope of the MATRC-sponsored workgroup that developed the original framework) to fully define the hallmarks of a “care model of the future”, here are four conceivable aspects of how care could and should be delivered in the future to provide excellent outcomes with the least amount of resources at the lowest cost.
Expansion of Care Services: With our increased understanding of the inner workings of our body, subspecialization is the key to improving the health of everyone. Providing access to care of that many specialists, proofs quite challenging — and given the decline in the need of physician exams in exchange for more precise tests, what’s more needed in patient physician interactions are explanations and joint decisions making on the most appropriate care plan. Furthermore, not all care must be delivered through real-time conversation.
Team-based Care: While not a new concept (I started my healthcare journey at the Mayo Clinic which over 100 years ago enabled a comprehensive team-based care approach by giving all specialists equal access to a complete patient record and by instituting medical grand rounds to discuss cases with a multidisciplinary team). Today’s team-based approach also involves technicians, nutritionists, therapists, etc. to aid in the execution of the care plan.
Care Coordination: While similar to team-based care, care coordination addresses the challenges of keeping everyone on the team informed and handling the hand-offs between different entities – from the hospital to a swing bed, from the nursing home to assisted living (under the care of the primary care team).
Value-based Care: A final key concept in the chorus of future care model approaches is the approach that steers away from the traditional fee for service model and rather focuses on the outcomes of care, the well-being of the individuals in a whole population. Under these economic circumstances, the question does not become whether payment for the service is available, but rather whether this will improve the patient’s well being – thereby presumably lowering the total cost of care.
Diving, deeper, her are four examples of how technology can enable the creation of an evolved care model:
Technology-Enabled Expansion of Care Services
In today’s world, the majority of care is (still) delivered through one-on-one, real-time in-person clinician-patient encounters, though group treatment options are available in some circumstances (e.g., for chronic care management, or group therapy).
A technology-enabled expansion would not only take the delivery of care outside of the exam room (a.k.a., video visits), it could also eliminate the need for real-time interaction (e.g., asynchronous secure messaging) or even replace much of the standardized elements of care (e.g., pre-recorded or an AI-generated explanation of a diagnosis, or preparation for a surgical procedure).
Furthermore it is conceivable to enable proactive care pathways through near-real-time feedback loops (individualized to the patient’s unique situation) and to seamlessly bring rapid and easy access to a multidisciplinary team to the patient, vs. the reliance on a single clinicians.
The opportunities for better care and hyper-optimized clinician time are technologically within reach, but changing the culture of healthcare delivery is now the larger challenge.
Technology-Enabled Virtual Team-Based care
A few years ago, the concept of the patient-centered medical home (PCMH) swept through the healthcare world and brought a new meaning to the age-old saying that it takes a village to care for a child – and definitely a multidisciplinary team to care for a sick villager.
But the complexities of quality communication across a multidisciplinary team were challenging enough within one co-located team, given the rigidity of supportive technologies to accommodate the myriad of unique circumstances. In addition, once patients received or team members delivered care virtually, the timely exchange and maintenance of the integrity of information became daunting and close to impossible.
With the availability of technology solutions that support “virtual team-based care” in a much more flexible, customizable way, new opportunities opened up to not only treat patients remotely, but to also integrate super-specialized team members that are not embedded in the core team of the PCMH.
As in the first application, asynchronous communication across geographically dispersed teams allows access to subspecialty expertise with a common repository of critical information about the patients history and up-to-date (or even real-time) information about current condition.
Technology-Enabled Care Coordination
Treatment in the 21st century rarely happens in isolation provided by a single clinician. Rather, a multidisciplinary approach involving specialists (from endocrinologist to cardiologists), therapists (from psychological to occupational), and technicians (from phlebotomists to sonographers) is required to achieve the best possible outcome.
Once again, the complexities of timely and accurate information stand in the way of scalability (treating more patients, in more geographic areas), of comprehensiveness (involving even more specialists, therapists, or technicians), or simply of providing basic quality care.
With computers being predestined to dealing with complex and vast amounts of information, innovative solutions can enable timely, comprehensive, and high-quality care coordination. Yet those solutions cannot stand alone, making their use inefficient and prone to error. Rather, fully EHR-integrated solutions are needed that are optimized for the desired care coordination workflows in order to be “future proof”.



Technologically Enabling Value-based Care
The opportunities for enabling value-based care are almost endless. From just-in-time care interventions based on continuous vital sign monitoring, using data analytics to focus on the patients that stand to benefit most, to predictive modeling to detect the onset of disease early based on a multitude of parameters.
Software-based tools for performing analytics and evaluating elements of a value-based contract or care delivery model’s success metrics are key to direct the scarce resources to those interventions on the patient population that will yield the biggest benefits. The processing of this vast amount of data is almost impossible for humans to perform effectively. Oftentimes bias (such as first impression or cultural bias) will lead to an allocation of efforts that is skewed and not optimized for the critical results. Technology can help minimize the bias and prevent overlooking patients that stand to benefit most from interventions.
The Challenges of Technology Adoption
Over the past two decades, the oftentimes government-mandated electronification of the healthcare system left many clinicians jaded and scarred by the haphazard implementation of technologies. And rightfully so: not only were many of the solutions not optimized for an acceptable clinical user experience, the rollout of solutions ignored the core principles of effective change management.
Against this backdrop of bad experiences, it’s easy to understand why many clinicians are so hesitant to embrace new technologies.
Yet as outlined above the future of care delivery depends on the appropriate integration of technologies that can make the clinicians’ (professional) lives easier, dramatically improve patient outcomes, and lower the overall cost of care.
For more information on “accelerating the adoption of innovation”, you can read my collection of past articles on this topic (especially article #5 on “Successful Innovation Implementation”).
Are you or is someone in your network working in a Community Health Center?
Then reach out to me for more information about the current “Health Center of the Future Training” initiative by the National Association of Community Health Centers (NACHC).










To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.








