My introduction to healthcare came in 2000 when I joined the Mayo Clinic in Rochester, Minnesota. Having never been exposed to healthcare before and having only moved to the US two years prior, little did I know how unusual and unique this introduction to healthcare was.
One of the key tenets of the Mayo Clinic, that I’ve repeatedly quoted, is that “The Needs of the Patients come first.” And it’s not just an empty slogan, but truly considered repeatedly by all staff, even by those working two or three layers behind the front lines of care delivery.
As with many organizations that put the customer experience first, this mindset has served the Mayo Clinic well for over a century. It was adopted from a quote from one of the founding brothers Mayo: “The needs of the patients are the only needs to be considered.” Back then, in the 1920s and 1930s, when physicians often reigned as “demigods”, this was a novel, almost revolutionary mindset.
In recent decades, many organizations have also focused on putting their people, their staff first — because dissatisfied, disgruntled employees can’t really be compelled to provide a great customer experience. In healthcare, where many of the staff and most of the clinical staff are deeply driven by the desire to serve the patient, focusing on the patient also creates a strong alignment for the values of the staff responsible for providing the care, for creating the patient experience.
Whenever we are designing a set of telehealth success metrics (see our articles on “Measuring Telehealth Success”), patient satisfaction AND clinician satisfaction are always at the top of our list: rare is the provider frustrated with the process or technology of telehealth that has provided a great patient experience during a video visit.
The Needs of the Patient
Healthcare has long made it its job to know what patients need — particularly in terms of their medical, physiological, and psychological needs. With the transition from obedient patients to the Modern Healthcare Consumer, the needs to be considered now transcend beyond mere care.
As in other service industries that are relentlessly focusing on the customer experience, the patient’s experience during a clinic visit or a hospital is nowadays a very important factor to consider.
Why? Because to achieve the best outcomes, patients cannot just merely follow instructions. They need to be involved in their care, they need to be engaged, and “fully activated”. Whether that includes following their medication regimen, engaging in physical therapy, or making fundamental lifestyle changes to increase healing — the patient’s participation in their care is paramount to the modern approach of care delivery.
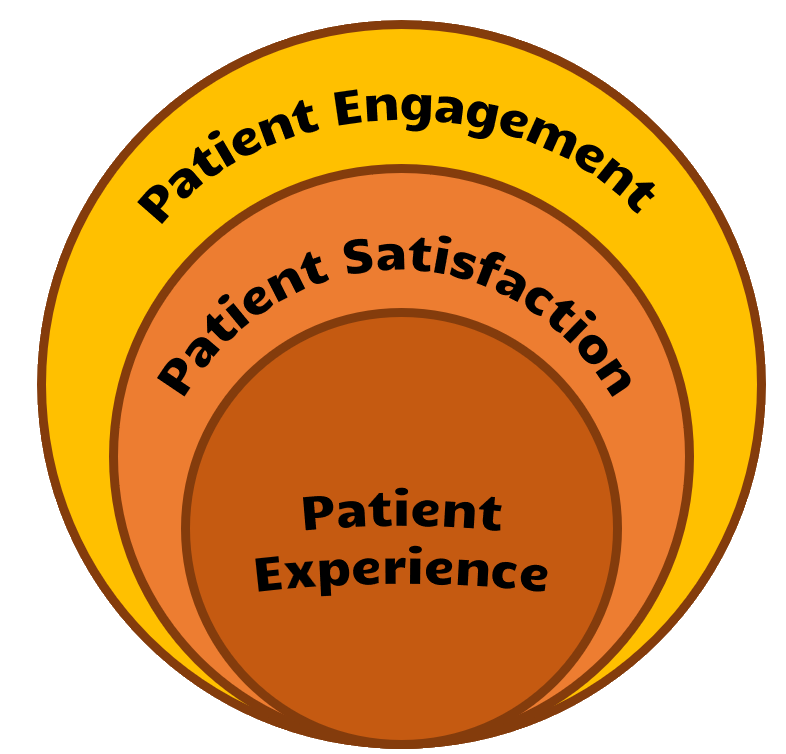
Patient Experience
In simple terms, the patient experience is the totality of the patient’s interactions with healthcare — from scheduling an appointment, traveling to the clinic, checking in, waiting, and visiting, to paying the bills. Each interaction, each transaction forms a piece of the patient experience puzzle and virtually everyone in healthcare has a role in influencing that experience.
Here are four key components of “experience” that are worth contemplating for the various services healthcare delivers to patients:
Credible: Can I trust the information given to me, the advice provided? Do I trust the provider’s expertise? Did the staff convey competence?
Accessible: How easy was it to accomplish what I needed? Was it easy to schedule an appointment, to get to the visit, to download the notes, to refill my prescription? Could I find what I needed?
Usefulness: Was the interaction helpful to me? Did I get the information that I needed? Did this help me to improve my current situation?
Valuable: Did the experience leave me better off? Has my situation improved? Has the interaction experience or information received helped to solve my problem?
In short, the Patient Experience reflects the patient’s subjective experience with your healthcare organization — whether that’s directly with staff or through automated systems.
Patient Satisfaction
The patient’s satisfaction is best described as the gap between the patient’s explicit and implicit expectations and the actual experience.
On the one hand that means that you are “at the mercy” of the patient’s pre-formed expectations: if their expectations are unrealistic or idealistic, then no matter how good the experience is, patients will be dissatisfied.
The obvious solution here is to proactively set expectations — and to quickly dispel myths and correct any assumptions that cannot be met. Proactive and frequent communication is key and will prepare the patient for a much better, more satisfying experience.
Obviously, the most control you have is over the actual experience that you are providing, so investing in understanding the patient’s expectations is also key to achieving a high satisfaction.
Patient Engagement
To achieve the best possible outcomes — aside from an accurate diagnosis, high-quality treatment, and compassionate care — it is equally important to fully engage the patient in their care journey.
A great patient experience resulting in high patient satisfaction will much more easily facilitate a high degree of patient engagement, resulting in a higher degree of the patient’s participation in their care and their treatment.
Measuring Experience, Satisfaction, and Engagement
In order to improve any of the three patient-centric aspects, the first step is to periodically and systematically measure each. Of the three, patient satisfaction is the easiest to measure, though it also provides the least-valuable information about the root causes of patient dissatisfaction.
Typical patient satisfaction measures get at the patient’s subjective opinion about the experience: Was the care good? Were the doctors and nurses friendly, and courteous? How likely are you to recommend this service to others?
Much more meaningful measures assess the patient experience more objectively, for example by looking at process measures: E.g., were you greeted promptly? Did the provider confirm that all your questions were answered? Were you offered a virtual care follow-up appointment? Etc.
The insights gained here can lead to specific process improvements that lead to a better care experience.
Finally, measuring patient engagement as an indication of patient outcomes can include a variety of measures that are indicative of how much the patient is committed to participating in their care, e.g.,
- no show and cancellation rates
- patient retention over the years
- adherence to care plans – medications, exercise, referrals
- care management graduation rates
- frequency of patient portal use
- patient activation measures
- etc.
Leveraging Virtual Care
With convenience and affordability ranking very high on today’s Modern Healthcare Consumer’s expectation list, virtual care with its multitude of modalities and plethora of scenarios offers outcome-driven organization and a wide range of options to improve the patient experience, achieve high levels of patient satisfaction, in order to create a high degree of patient engagement.








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.








