Many leaders see the wisdom in embracing “care at a distance” for their organization. Yet once they look at their clinician’s utilization data, they are often surprised about the discrepancy of the media’s description of high telehealth utilization and their own organization’s low use of telehealth in primary and specialty care beyond behavioral health.
In our experience over the past 15 years, and especially over the past 3 years post Covid, this oftentimes stems from not adhering to these five core principles for a successful telehealth adoption:
- Design your telehealth services around the Needs of the Patients.
- Focus relentlessly on enrolling and Engaging your Clinicians.
- Accept (and act accordingly) that this is an exercise in Change Management.
- Create a culture of Accelerated Innovation Adoption.
- Invest in a designated launch, operational, and technical Support Team.
Principle 1: Design for the Needs of the Patients
In the year 2000 I was lucky to stumble into healthcare at the Mayo Clinic in Rochester, Minnesota. With an innovative approach to care delivery (Mayo invented and perfected the paper-based integrated medical record starting in the early 1900s) and a cadre of brilliant physicians and dedicated nurses, I immersed myself in a culture that the Mayo Brothers had established more than 100 years ago and that somehow survived and evolved over the years.
One of the Mayo Clinic’s key mantras and value statements, which truly is alive and applied to decision making every day, is that the Needs of the Patient come first — A modern version of one of the founding Mayo brothers’ quotes that “the needs of the patient are the only needs to be considered”.
Similarly, as you consciously design your organization’s approach to delivering “care at a distance”, it is critical for sustainable success that this is done with the patient experience in mind.
While in an in-patient experience we have multiple opportunities to shape the patient’s experience and quickly correct for small mistakes, when the patients is miles away, course corrections are not as easy to provide.
Thus the most important question that anyone involved with telehealth needs to know the answer to is: what do our patients want and how can we provide them with what they need?
For some of our clients that led to the implementation of a Telehealth TechCheck before a patient’s first telehealth visit to address any questions or uneasiness the patient may have and to ensure that the visit goes well for both the patient and the clinician.
Other considerations include the review of patient communication before, during, and after the virtual visit, a continuous evaluation of the overall user experience, and customized training for clinicians on how to effectively conduct virtual visits (including physical exams).
Principle 2: Enroll Your Clinicians in Telehealth
But the telehealth experience should not only be optimized for the patients. Indeed for the patients to have a stellar experience, the most critical factor is the attitude and aptitude of the clinicians to conduct a telehealth visit well.
This means that your clinicians need to be engaged, i.e., committed to offering and conducting telehealth visits that are at least as good as in person care. As you’ll see in the next section, this is about the following:
- Making clinicians aware why telehealth as an alternative care delivery modality is a clinically and technically viable option.
- Creating in clinicians a desire to leverage telehealth in their practice, providing them with the necessary clinical rationale (e.g., for continuity of care, a telehealth visit is better than no visit) and financial reality (e.g., today’s modern healthcare consumers have alternative choices and many of them are virtual).
- Providing clinicians with the knowledge and ability to conduct telehealth visits with confidence and without hesitation. This includes well designed workflows and process handoffs as well as clinician training on webside manners, virtual exams, and proper documentation.
- Periodically checking in with clinicians whose usage is below the average of their peers to examine whether some process or technology issues (or lingering questions about the clinical efficacy) are standing in the way of them using video visits more often.





Principle 3: Telehealth Adoption is a Change Management Exercise
Most clinicians have been trained at least 15 years to provide care in an in-person environment and the experience during Covid (where most telehealth resorted to telephonic care) left many clinicians either affirmed in their pre-Covid perception that telehealth does not work, or left them disillusioned about telehealth’s potential.
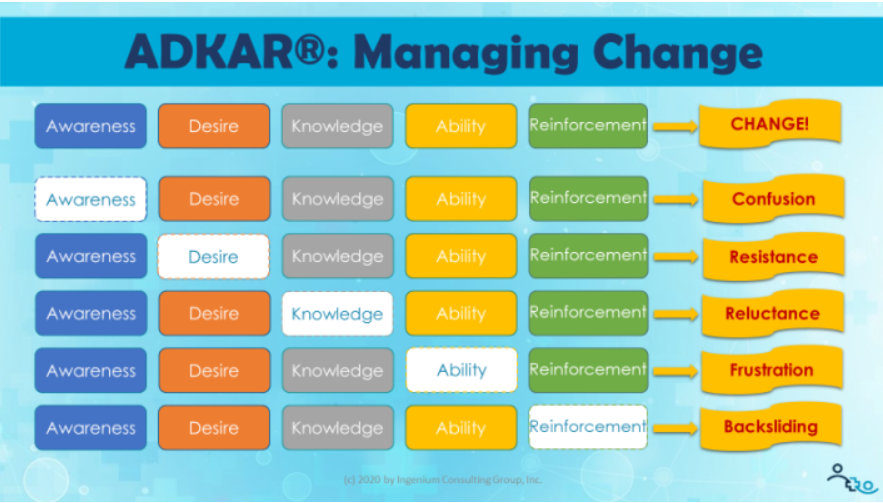
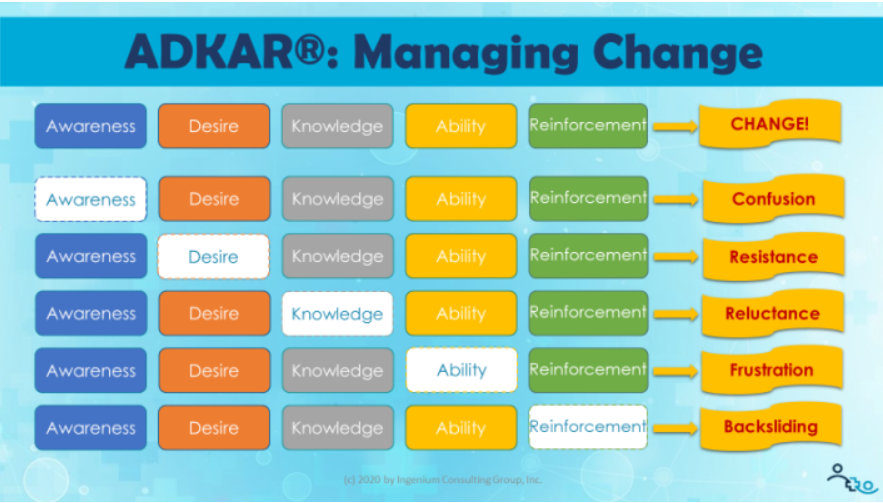
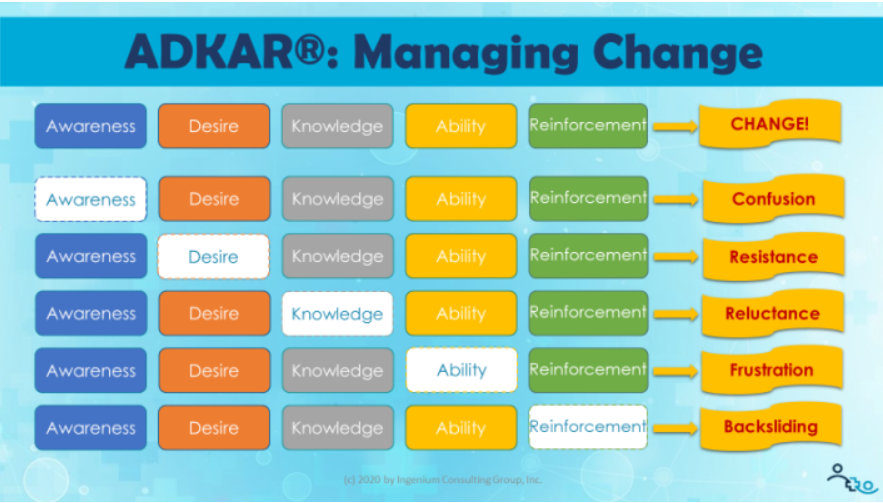
Thus for an organization to truly adopt telehealth well, it must approach the adoption as an exercise in change management. Our favorite model to guide change management is the Prosci Institute’s ADKAR® model: Awareness, Desire, Knowledge, Ability, and Reinforcement.
In this model, the focus is first on raising Awareness among the clinicians and staff as to why telehealth now is clinically, financially, and strategically more important than ever. This is best documented in a cohesive and inspiring Telehealth Strategy and Business Plan that for the people in the organization paints a vision for the future and lays out initiatives to undertake now and in the near future.
The next step is to instill in the clinicians and other staff the Desire to integrate the delivery of care at a distance into their clinical care delivery repertoire. This is also done through a well documented strategy (that provides the strategic and financial rationale), but also through key influencers and the clinical and medical leaders.
As described in the last principle, the next two steps are to provide all staff involved in the delivery of telehealth (from scheduling and rooming to post-visit followup and billing) with the appropriate Knowledge and Ability to support and conduct telehealth well.
Most importantly, from a sustainability perspective, is the Reinforcement of making sure that the change is sticking and people are not reverting back to doing it the more comfortable, the “more used to this” way. This is best achieved through the implementation of a Telehealth Success Management System that periodically reviews utilization, satisfaction and other performance metrics important to the organization.
Principle 4: A Culture of Accelerated Innovation Adoption.
Telemedicine, Telehealth, Virtual Care, Connected Health (or whatever you call it in your organization) does not stop with video visits to the patients home. There are numerous different other scenarios (here are 96 commons scenarios) telehealth modalities (here are 9 Telehealth Modalities), and novel technologies (now accelerated by the buzz around AI) that all fall into this category.
For sustainable, long-term success in telehealth adoption (and in preparation for other digital health innovations such as digital therapeutics), it is crucial to start creating a culture of accelerated innovation adoption.
The evaluation of new care delivery approaches enabled by technology should not take a year, but weeks and the validation and subsequent organization-wide deployment should not take multiple years but only multiple months.
Non-traditional competitors such as Amazon, Walmart and a whole slew of startups are built on a culture of constant innovation. To keep up “with the Joneses” healthcare organizations must up their game when it comes to embracing innovation.
Principle 5: Invest in Commensurate Telehealth Support
I saved one of the most important principles for last: to invest in people, especially individuals to support the care delivery team and patients in the scheduling, conducting, and post-visit follow up activities of telehealth.
Support for telehealth has to come in multiple forms:
- operational support for the continuous improvement of the workflows and training an retraining of clinicians and staff;
- technical support to instantaneously solve connectivity or connection issues and aid in the integration of telehealth technology into the technical ecosystem
- launch support (including process design, training, and project management) to support the rollout of new telehealth services or new telehealth modalities
- governance — the leadership and steering by senior leadership and a multidisciplinary team that represents all the aspects of care delivery at a distance from scheduling and rooming to technology and finance.
A minimal starting point for appropriate support is the creation of a Telehealth Coordinator role, responsible for providing the aforementioned operational and launch support and acting as a liaison to technical support and the steering team.
Without support and telehealth left to the staff and clinicians “to figure it out”, utilization will continue to stay well below what’s possible and what’s demanded by your patients.
What principles for successful telehealth adoption have you found worked for your organization? Let us know in the comments below.










To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.








