A quote from one of the brothers Mayo, Dr. Charlie Mayo, has stuck with me all these years:
“Today the only thing that is permanent is change.”
The quote was recorded almost 90 years ago in 1931 and never was more true than today. If change is what we have to deal with constantly, shouldn’t we get better at managing it?
Which is the topic of this article: How through conscious telehealth change management we can achieve Telehealth Success.
A Framework for Change
It was also at the Mayo Clinic that I was introduced to my first change methodology: the Prosci ADKAR® model. Developed by Prosci’s founder and backed by “20 years of research”, the model has found its way into many organizations, especially in healthcare.
The model, as explained in more detail below, focuses on getting five principles right, in order to support people in accepting and supporting the change. Let me use telehealth as a specific example:
- Raise awareness as to why offering telehealth is needed.
- Create within all affected stakeholders (clinicians, staff, patients, etc.) the desire to support telehealth.
- Provide everyone with the necessary knowledge regarding their role and responsibilities to offer telehealth – e.g., scheduling, launching a visit, coding, billing, coding, etc.
- Create for everyone the ability to adhere to the telehealth policies, to operate the technology and to present themselves professionally on camera.
- Provide continuous support in the form of supportive reinforcement through feedback on the performance of the telehealth services including clinician satisfaction, patient satisfaction or reimbursement-related measures.
Together the A-D-K-A-R elements form the basis for enabling sustainable change.
What is Conscious Change Management?
So how can you achieve Telehealth Success through Conscious Change Management?
The level of consciousness with which an organization manages change is directly proportional to the maturity of an organization’s experience with changes overall. In healthcare, even the assignment of a project manager for organizational initiatives (except for architectural, infrastructure and large-scale IT projects) was not the norm even 15, 20 years ago. In smaller organizations the operational person in charge may even hold the title of “project manager” but often with little to no training beyond the identification and tracking of tasks.
The same holds true for change management. Many teams look at an outcome that must be achieved and the tasks that must be accomplished to achieve that outcome. Very few take a step back to proactively anticipate opposition to the change. While opposition to change is widely expected (and often anticipated with some cynicism), the knowledge about what to do about it is not as widespread.
Conscious Change Management thus is the purposeful, proactive identification of activities to minimize opposition to the change, by maximizing buy-in and support while minimizing confusion, reluctance, frustration, or outright resistance.
With our best clients, consciousness starts at the top with the leadership team that allocates sufficient resources and demands focus on proactively managing the change brought on by the launch and optimization of telehealth.
The ADKAR® Model for Telehealth
What I like about the Prosci ADKAR® model is it’s simplicity, breadth and it’s cleverness to explain the various types of threats to a successful change. The brilliance of the model is that it addresses the various emotional needs of the people affected by the change – something we can all relate to.
The model postulates that there are five aspects of the change that you need to pay attention to: Awareness, Desire, Knowledge, Ability, and Reinforcement. Let’s tackle each of these in turn and apply them immediately to the creating high-performing telehealth services.
Awareness
The first step in the model is focusing on the realization that people must be aware of the need for the change. It’s answering the “Why are we doing this question”.
Before the Covid-19 crisis, the answer to the question “Why do we need telehealth” was not always obvious or was not always met with agreement. In the minds of many, Telehealth was something to be reckoned with “in the future”, but not necessarily now. However, for those who could see the long-term benefits for physicians and patients the “Why” was obvious: “because it allows me to see patients that live further away or for whom it may be difficult to travel to see me.”
Obviously during the Coronavirus health crisis the “why” became obvious: because telehealth is a solution that allows us to keep our patients and our staff safe. Also, nobody could claim ignorance about telehealth anymore, so Awareness about the need for telehealth became widespread.
However now that organizations are contemplating how to integrate telehealth with their in person care in “hybrid care delivery” models, the question of “Why do we need telehealth” (post-Covid) needs to be addressed again.
Desire
Many people are familiar with the WIIFM concept – “what’s in it for me”. It is naturally the first question we ask ourselves and without an internal desire to change, virtually no leader in the world can make a person change without the person’s agreement, which stems from their desire.
In the early days of the Covid-19 health crisis, the desire was fueled by wanting to protect patients, staff and self — by using telehealth to keep patients out of the practice and deliver “care at a distance”.
Post-covid we’ll have to take another look at the benefits to patients, clinicians and potentially the organization’s overall business model to find the continued desire to maintain the change of embracing telehealth as a viable care modality
Knowledge
Knowledge, as they say, is power and the absence of knowledge can thus make one feel powerless. Which is especially true for clinicians, who are used to being in the position of holding unique knowledge. This dimension of change is about knowing how to change.
In the context of telehealth, that knowledge is mostly about the new workflows, the new policies and the new technology. When as a clinician you are used to being in charge of the patient visit, having to “relearn” all of the processes can be very disorienting.
Ability
The aspect of ability goes hand in hand with knowledge and can largely be achieved through training. It is concerned with being able to perform the needed skills and behaviors.
One example is the “webside manner” training I conduct where within 10 minutes I can significantly bolster clinicians comfort level with being on camera. In the training clinicians can learn a few tricks that give them the confidence to appear professional and connect well with the patient on the other end.
Reinforcement
The last dimension to ensure sustainable change is the one of continuous reinforcement. Old habits die hard and the “old way of doing things” feels more comfortable to us longer than we care to admit.
Reinforcement is about making the change last and requires continuous measurement of key performance indicators and providing feedback when targets are not met. Not in a punitive manner, but in a way that seeks to understand the root causes for the deviation from the target, offering support and help to bring the performance back in line with expectations.
Putting it all together
Sustainable change is achieved when all five components are in place: when clinicians are aware of “the why”, have the innate desire to support the change and are equipped with the knowledge and skills (ability) to do so, supported by periodic feedback (reinforcement).
One for All and All for One
The most fascinating aspect of this model, however, is what happens when you leave just one of the five components out. Doing so brings out one of five oppositional forces to change: confusion, resistance, reluctance, frustration, and backsliding (“CRRFB” 😉 as the following graphic illustrates.
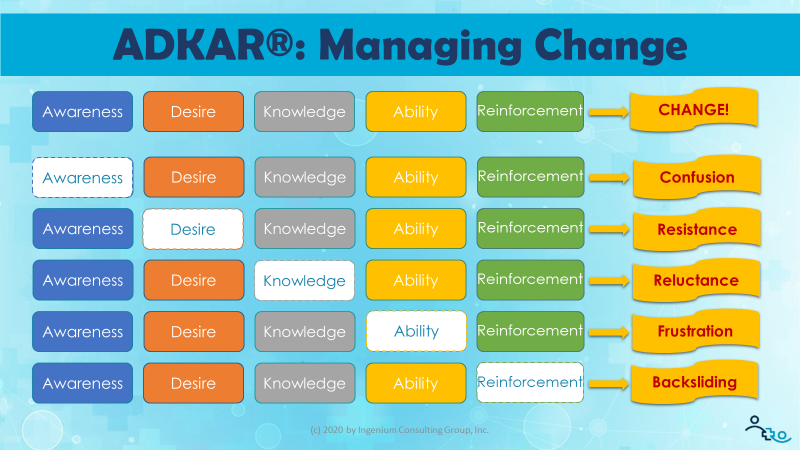
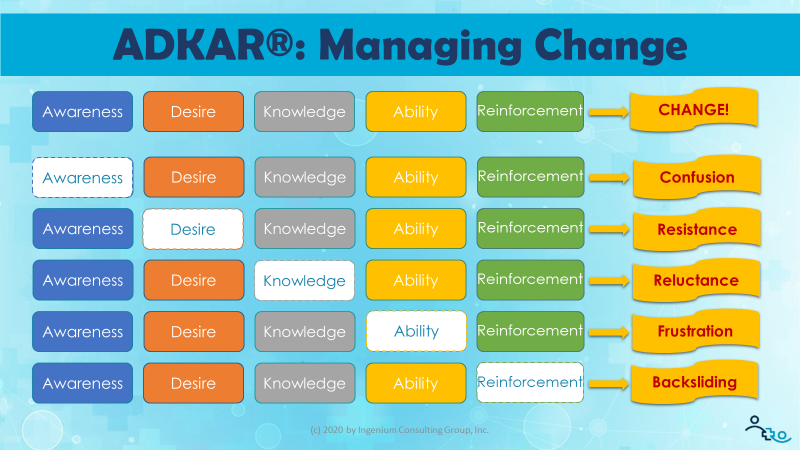
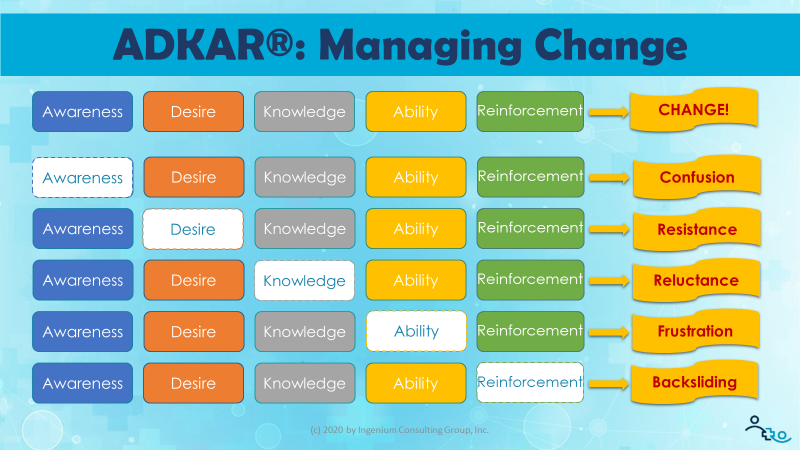
Confusion: The lack of awareness leads to confusion. “Why are we (still) doing telehealth?”, “Why do *I* need to do telehealth?”, “I thought this telehealth thing was only temporary.”
Resistance: Without an answer to “what’s in it for me” and a lack of desire, the obvious response is Resistance, one of the most challenging opposition to change. To overcome resistance, it’s important to study the resistors’ motivations. It may be a lack of knowledge (e.g., about telehealth reimbursement) that leads to a lack of desire.
Reluctance: When people do not have the knowledge of what exactly is expected of them, what the rules and processes are, then most people will be reluctant to move forward. This is especially true for clinicians who are highly trained and used to being fully “in control” of their domain of caring for patients. Suddenly not knowing what to do and not do can be very disorienting and therefore lead to a reluctance to fully immerse themselves in telehealth.
Frustration: Nothing can be more disconcerting than not having the ability to do it right. Sometimes especially technology can make us feel really stupid. “This should be easy to figure out.” is a common positive attitude, but even the best technology has its idiosyncrasies that need to be taught. For telehealth there is also the aforementioned soft skill of the webside manners that, until that ability is mastered, can lead to frustration.
Backsliding: Last but not least, sustainability cannot be achieved without the continuous feedback created by “reinforcement”. By giving everyone feedback on satisfaction, on financial performance and on other relevant metrics, the change has a chance to “stick” and become “the new normal”.
The good news is that by providing a rationale (“WHY”), addressing their needs (“WIIFM”), providing education (“WHAT”) and training (“HOW”) you can easily overcome the first four oppositional forces. And with a good telehealth success measurement program you can even avoid backsliding.








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.









Leave A Comment