Why after 30 years Telehealth is still Healthcare’s Most Underutilized Strategic Asset
Depending on who you ask, Telehealth (the “delivery of care at a distance”) goes back to the 1950s (transmitting an ECG), the 1960s (humans in space), or 1963 (a telecommunications link between Boston Logan Airport and Massachusetts General Hospital).
Telehealth definitely came into being in the 1990s, when academic medical centers were looking for ways to ease access to their specialty care providers. The University of Virginia is one of such early adopters and nowadays patients can connect virtually with 60 specialty services.
After two more decades of incremental adoption and four years of COVID-accelerated implementation, telehealth has (finally) evolved from a niche solution into a fundamental component of modern healthcare delivery. Yet despite reliable technology, established reimbursement, confirmed clinical quality, and overwhelming patient acceptance, most healthcare organizations are still dramatically underutilizing telehealth’s potential.
The question isn’t whether telehealth works — it’s why so many healthcare leaders remain oblivious to the enormous value telehealth can deliver across every aspect of their organization’s strategic objectives.
The Misunderstood Nature of Telehealth
Too many healthcare executives still view telehealth through the narrow lens of “video visits during COVID”. This limited perspective misses the broader strategic opportunity that telehealth represents: a comprehensive toolkit for delivering care at a distance that includes modalities such as video visits, remote physiological monitoring (RPM), store-and-forward technologies, secure messaging, and digital therapeutics.
When John Halamka joined the Mayo Clinic (where I spent 12 years learning about great healthcare) in 2020 to lead their digital transformation, the pandemic compressed their original 10-year plan into less than one year. As he noted at the time, the future would demand “more telemedicine, telehealth, hospital-level care in the home, wearables and the ability to apply machine learning and artificial intelligence to new data sources.”
That future is here. The modern healthcare consumer — empowered by technology and demanding convenience — expects healthcare to match the accessibility and responsiveness they experience in every other aspect of their lives.
The Breadth of Telehealth Value
Healthcare organizations that fully embrace telehealth’s potential see transformational results across these seven critical areas:
1: Maximizing Patient Access & Convenience
Telehealth eliminates the most significant barriers to healthcare access: time and transportation. A typical in-person visit requires patients to invest 6 times more time than the actual clinical encounter — when you count driving, parking, waiting, and then reversing the entire process. A telehealth visit from home can cut this to mere minutes. And you can fold laundry or prepare food while you wait.
For many patients, especially those managing chronic conditions, juggling work schedules, or lacking reliable transportation, telehealth isn’t just convenient — it’s the difference between receiving care and delaying it until problems become urgent and expensive.
2: Enhancing Clinical Outcomes
The data is clear: when care is convenient and accessible, clinical outcomes improve. Telehealth enables more frequent patient touchpoints, better medication adherence, and earlier intervention before conditions exacerbate. Studies consistently show significant reductions in high-cost utilization such as emergency department visits and hospital admissions when patients have easy access to their care teams.
Remote physiological monitoring takes this further, providing daily insight into patient health that enables proactive rather than reactive care. Some RPM programs for readmission prevention have demonstrated ROI of 13x — a $1,300 return for every $100 invested.
3: Improving Provider Satisfaction & Retention
In today’s competitive healthcare environment, recruiting and retaining quality clinicians is critical. Telehealth offers providers flexibility, variety, and the opportunity to practice at the top of their license. Clinicians can see patients from home, offer evening hours for working patients, and focus on clinical care rather than the logistics of traditional office visits.
When implemented thoughtfully, telehealth consistently achieves high physician satisfaction scores — often above 4.5 on 5-point scales. The key is proper training, optimized workflows, and clinical use guidance that help providers understand when and how to use virtual care effectively.
4: Strengthening Financial Performance
The financial benefits of telehealth extend far beyond simple cost savings. Organizations can increase revenue through:
-
Geographic expansion serving previously unreachable patient populations
-
Schedule optimization by converting no-shows and cancellations into billable telehealth visits
-
Service expansion adding specialties and RPM programs that weren’t previously feasible
-
Patient retention by meeting modern consumer expectations for convenience
Simultaneously, telehealth can reduce losses, e.g., by
-
avoiding readmission penalties (82% of hospitals faced readmission penalties averaging $208,000 in 2022),
-
decreasing recruitment costs through improved retention of clinicians
-
avoiding revenue losses by reducing no shows and same-day cancellations
-
multi-site virtual clinical sharing, e.g., if a provider is out sick, a provider at a different site can cover.
-
optimizing physical space utilization – e.g., alternating remote and in-person work schedules with a shared office
-
…and many more
5: Creating Strategic Competitive Advantage
Healthcare organizations that fail to offer comprehensive telehealth services risk losing patients to competitors who do. Virtual-first companies like Teladoc, CVS, and Amazon Care are aggressively targeting the “convenience-oriented” patient population with accessible, technology-enabled care — who are often the key to a profitable patient mix.
Traditional healthcare organizations have a significant advantage: they can offer the full continuum from virtual to in-person care. But this advantage only exists if they actively develop and promote their telehealth capabilities.
6: Improving Quality Metrics & Population Health Outcomes
Telehealth serves as a strategic tool for improving quality metrics that impact care quality, reimbursement, and accreditation. Whether it’s reducing readmissions, improving chronic disease management, or increasing preventive care compliance, telehealth provides additional touchpoints and more convenient engagement opportunities that drive better outcomes.
For population health initiatives, telehealth enables more frequent monitoring and intervention, particularly valuable in value-based care arrangements where patient engagement directly impacts financial performance.
7: Enabling Scalable Organizational Growth
Perhaps most importantly, telehealth creates infrastructure for serving more patients without proportional increases in physical space, staffing, or overhead. Organizations can hire virtual-only providers, share exam rooms across multiple locations, and extend specialist expertise across wider geographic areas.
This scalability becomes critical as healthcare demand continues to grow while physical and human resources remain constrained.
The Cost of Inaction
Organizations that fail to fully embrace telehealth aren’t just missing opportunities — they’re actively leaving value on the table. They’re losing patients to more convenient competitors, missing revenue from unfilled appointment slots, paying avoidable penalties for poor quality metrics, and struggling with provider retention in an increasingly competitive market.
Most significantly, they’re failing their patients who increasingly expect and deserve convenient access to quality care.
The Path Forward
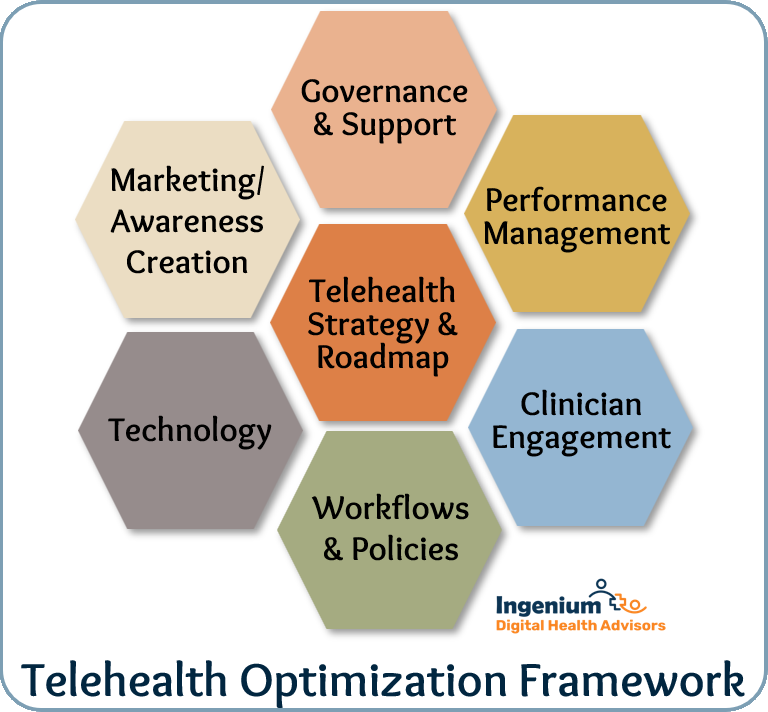
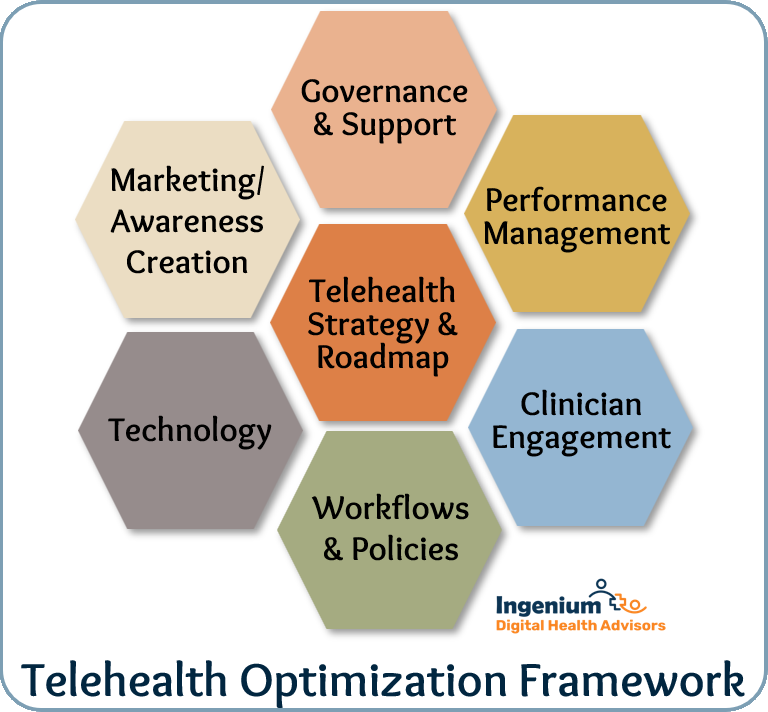
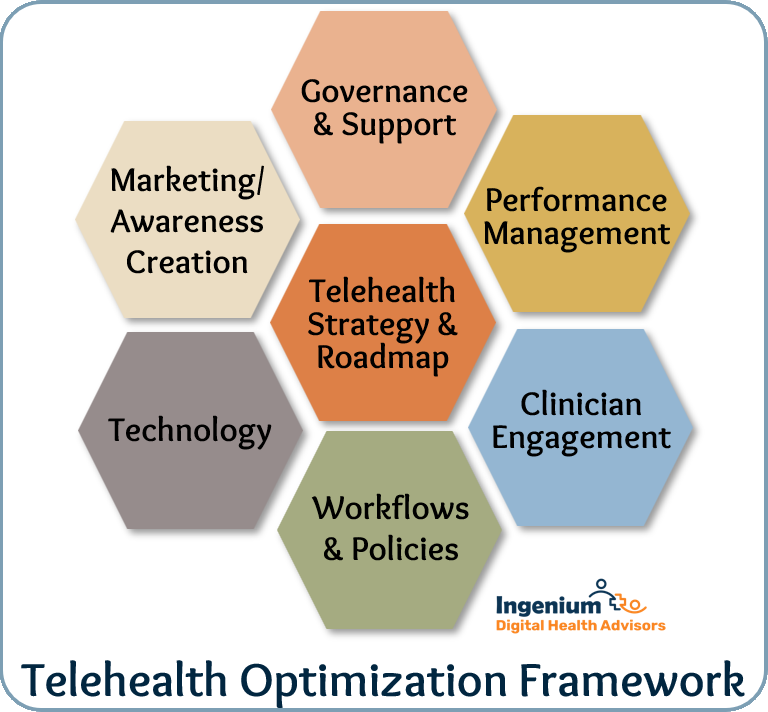
Successful telehealth implementation requires more than just purchasing video software and hoping for the best. It demands:
-
Leadership commitment to telehealth as a strategic priority, not just a COVID response
-
Performance measurement with clear metrics, targets, and actions for continuous improvement
-
Workflow optimization that integrates virtual and in-person care seamlessly
-
Provider engagement through training, support, and well-designed clinical guidelines
-
Patient education to maximize adoption and satisfaction
-
Technology selection that supports rather than hinders clinical workflows
It requires a strong commitment to continuously optimize telehealth — a topic we know a lot about, as reflected in the dozens of articles I’ve written on the topic.
The Opportunity Ahead
Telehealth represents healthcare’s most significant opportunity for simultaneously improving patient access, clinical outcomes, provider satisfaction, and financial performance. The technology is proven, reimbursement is established, and patients are ready.
The only question remaining is whether healthcare leaders will recognize telehealth’s complete value proposition and take action to capture it — or continue leaving this tremendous opportunity unrealized while competitors gain ground.
The future of quality care is already here. It’s just not evenly distributed yet.
What is your organization doing to capture the full value of telehealth? Are you ready to move beyond viewing telehealth as just “video visits” to embracing it as a comprehensive strategic asset? Start by assessing the maturity of your Telehealth Program.








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.








