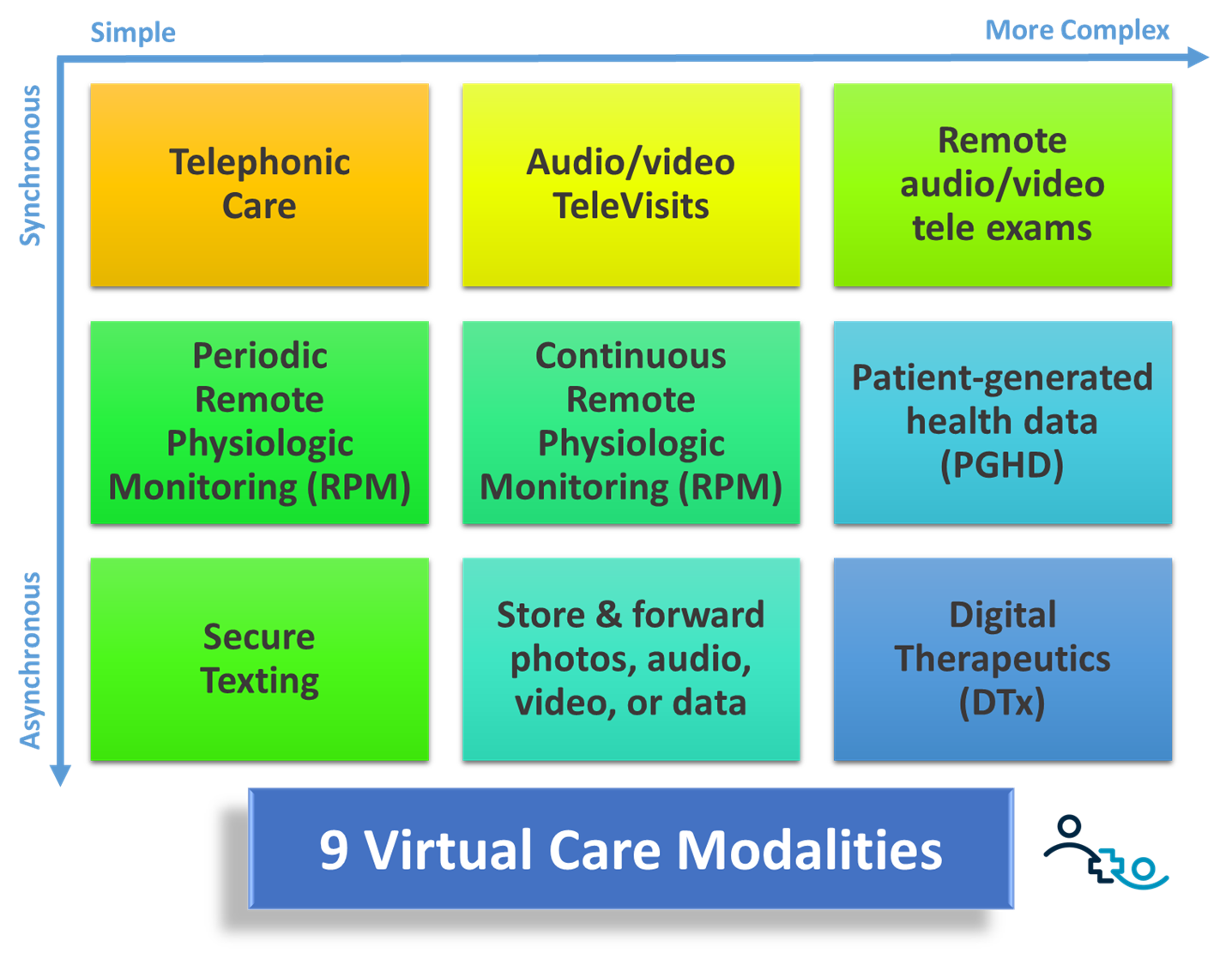
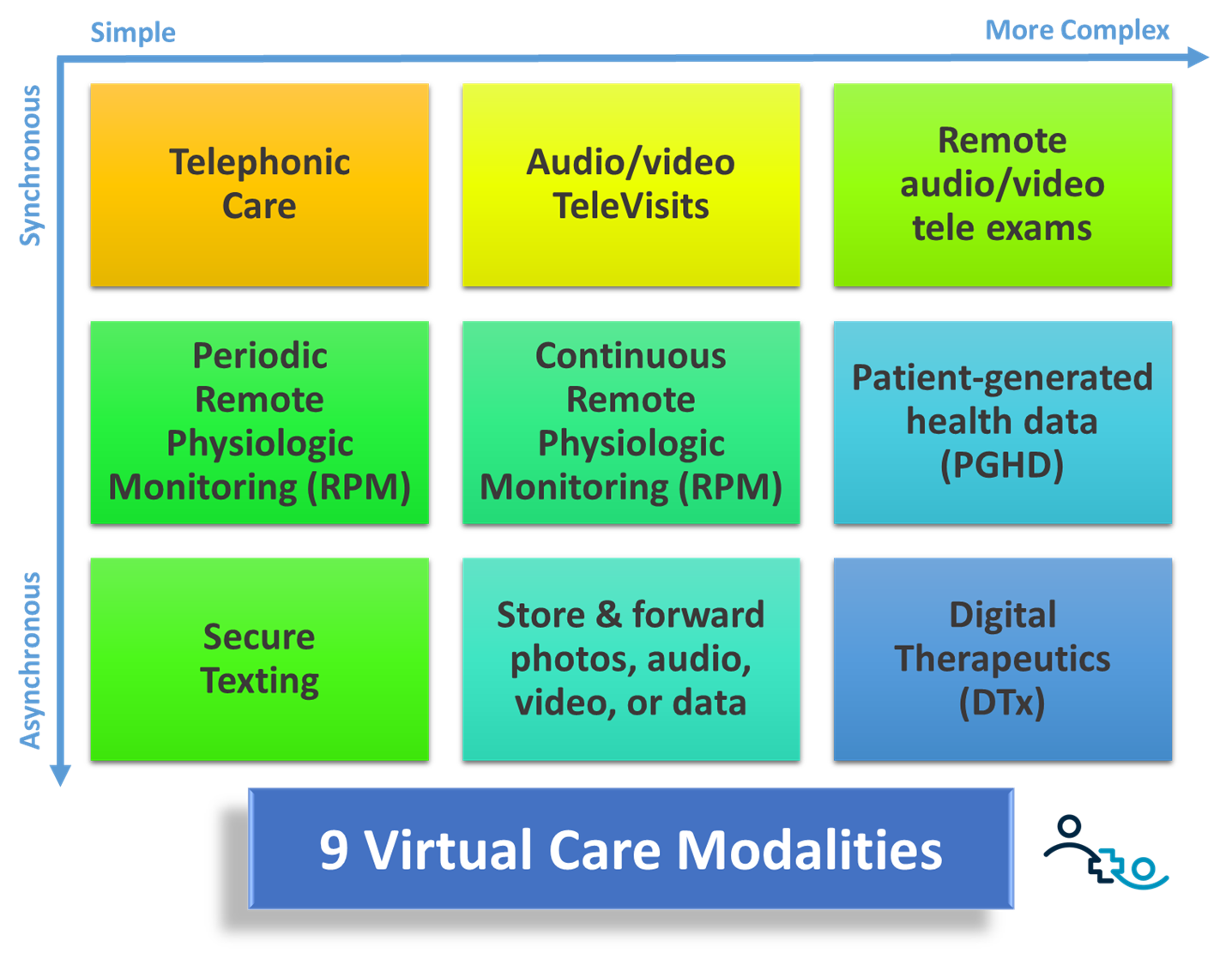
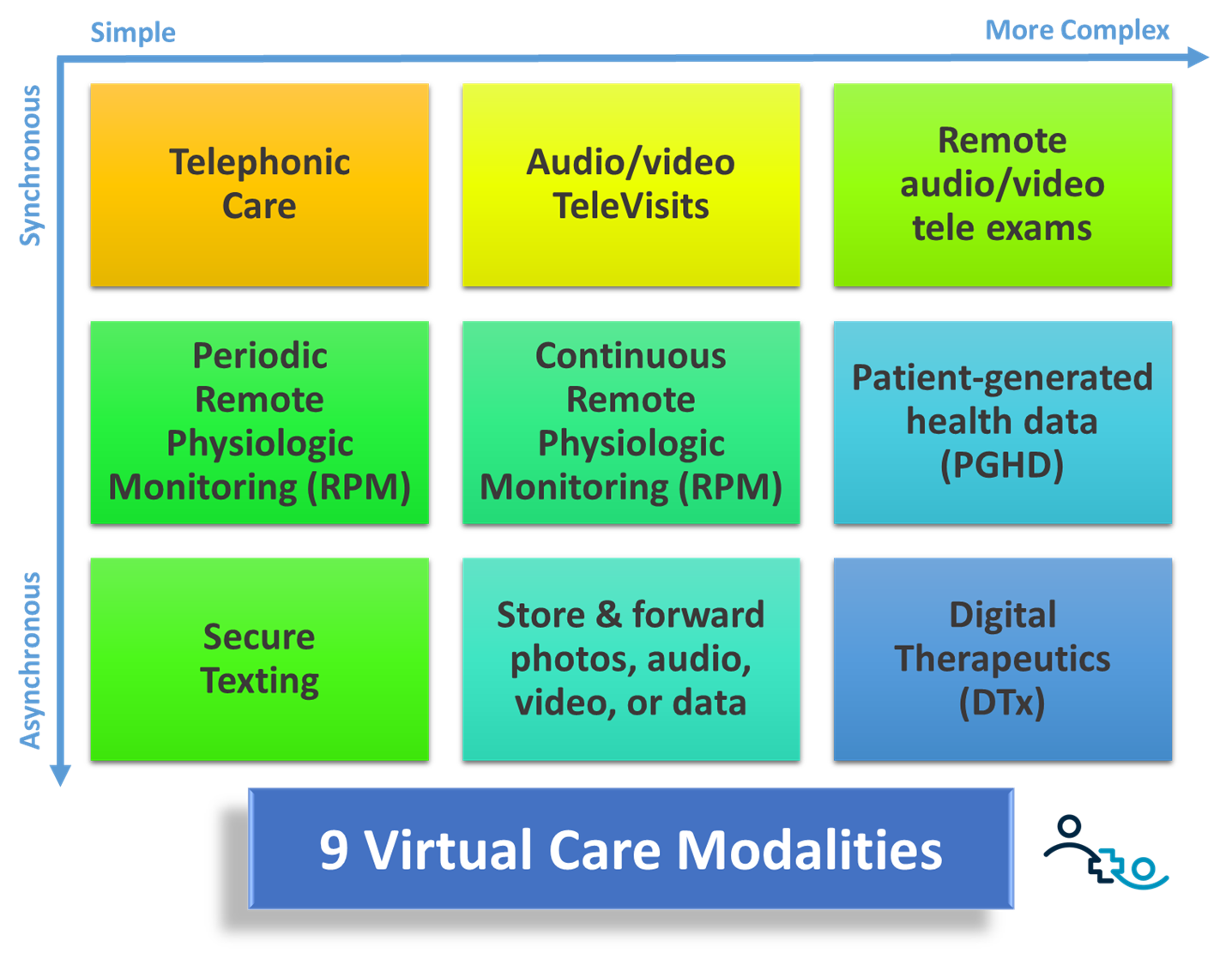
Post-Covid, telehealth has “survived” as a mainstay modality to deliver care to patients at a distance. And many healthcare leaders now more fully understand that telehealth is much more than just video visits, including patient portals, patient education, and a full host of virtual care modalities including remote physiological monitoring (RPM), virtual exams, and digital therapeutics.
What many healthcare leaders fail to appreciate is the positive financial impact telehealth can have on their organization’s bottom line by increasing revenue, reducing losses, decreasing costs.
As I wrote about before, Telehealth can add to the bottom line through an increase in revenue in multiple ways:
- Increasing Patient Loyalty
- Geographic Expansion
- Filling Schedule Holes
- Reducing cancellations
- Reducing No Shows
- Expansion of Services
In this article I’ll explore how telehealth can reduce losses and decrease cost, to create a tremendous financial case for investing in telehealth.
Using Telehealth to Reduce Losses
Losses in healthcare come in multiple (bitter) flavors and we’ll be considering three of those: lost revenue, penalties, and missed gains.
There are a few ways that healthcare providers can miss out on revenue opportunities — when existing patients stop using your organization for their care; when potentially new patients use a competitor (physical or virtual) to receive the care they seek; and when you do not have sufficient clinical staff to meet the demand.
Patient Attrition: In management there is the axiom that “employees don’t quit their job, they quit their bosses”. The corollary is also true in healthcare: patients are very loyal to their physicians, nurse practitioners, physician assistants and other providers. The relationship they cherish is with the human being on the other end that is “taking care” of them.
Yet in competitive environments and for patients who use healthcare infrequently and more or less “transactionally”, factors such as cost and convenience often outweigh the providers’ bedside manners. Yet it is that fairly healthy patient population that often yields the biggest contribution to the organization’s bottom line. Thus losing those patients (which may be hard to detect at first) can significantly impact a clinic’s profitability.
Telehealth — especially virtual visits, same-day virtual appointments, and a more user-friendly “digital front door” for self-scheduling appointments or downloading medical records — can greatly improve the patients’ opinion of how well the healthcare organization can take care of them. Failing to offer these “modern modalities” of access to care means running the risk of losing those patients to organizations that do this well.
New Patient Drought: New customers are the lifeblood of any organization and healthcare is no different. Most healthcare organizations rely on a small number of select profitable healthcare services to offset the losses incurred by other services. This ranges from elective surgeries for health systems to 340B pharmacy programs for community health centers.
To bring in new patients that would (eventually) leverage those services, iot is thus imperative that healthcare organizations position themselves as modern, forward-thinking organizations that acknowledge the modern healthcare consumers’ desire for convenient and speedy access to quality care. Similar as above, telehealth in its various forms can greatly contribute to improving the organization’s reputation in the eyes of the future patients.
Staff Attrition: Another way a healthcare organization can miss out on revenue is when there is not sufficient staff capacity to meet the existing or potential demand. Telehealth, as I explored in more depth in these linked articles, can be used to improve clinician satisfaction, combat clinician burnout, and help address the nursing shortage (click on each of the links for more guidance).
Penalties: Penalties are most often imposed by government payors when an organization is not meeting its quality goals. One prominent example is the avoidance of readmission penalties (in particular the lack of reimbursement of avoidable rehospitalizations) through RPM programs. This strategy often served as my go-to strategy for financial sustainability of telehealth programs when working with health systems before Covid.
And the need to expand RPM programs has seemingly not vanished: In 2022, 2,499 hospitals (82% of all assessed hospitals!) were called out by Medicare for failing to meet readmission standards, with an average penalty of $208,000 per penalized hospital. With proven, sustainable RPM programs having been around for more than 10 years, this lack of progress is, for me, shocking.
There are plenty of other quality metrics (e.g., UDS measures) where telehealth can be used as a strategic tool to move the needle into the right direction and to avoid the penalties associated with poor performance (set up a call with me if you’re interested in discussing your organization’s quality metric that you want to improve through telehealth).
Using Telehealth to Decrease Costs
In addition to increasing revenue and reducing losses (see above), the third area where telehealth can add to your bottom line is to help decrease costs.
Here are some examples how telehealth can help you achieve that.
Decrease Recruitment Costs: The costs of replacing a critical, revenue generating staff member are enormous when you take into account the higher salary and benefits, the time it takes to interview and select a replacement, and the lost revenue while the position was not filled. As referenced above, using telehealth to increase satisfaction, combat burnout, and address the nursing shortage, will result in less turnover and in turn reduce recruitment costs.
Decrease Marketing & New Patient Acquisition Costs: Traditional marketing, especially in large geographic areas, is quite costly. With more and more healthcare consumers seeking information online first, targeted online marketing and advertising to allow those in your area to find you can be much more cost effective. The simplest way is to set up a frictionless way to self-schedule a virtual visit from your home page. Winning a new patient has rarely been easier!
In addition, telehealth success stories (e.g., avoiding transportation to and from the clinic for a mostly home-bound patient) can provide wonderful publicity that is very much of interest to the local media.
Less need for Physical Space: As I’ve outlined in my strategies to combat clinician burnout, much of the telehealth work can easily be done from the clinician’s home (or another location of their choosing). For example, telehealth could be used to allow multiple providers to share an exam room by scheduling them “in the clinic” on separate days.
To expand the geographic reach (as outlined in the strategies for revenue growth through telehealth) no physical space is needed if a clinic location is within reasonable driving distance of the targeted geographic area. Alternatively, a simple small office, e.g., in an abandoned Main Street USA store front, can be staffed for a few hours a week by a “telepresenter” (a medical assistant or a nurse) to facilitate video visits and virtual exams with providers, without the need of opening a full clinic. Another option are mobile units that can create virtual makeshift clinics on virtually(!) any parking lot with cellular internet connection.
Increase Revenue, Reduce Losses, Decrease Costs
Telehealth is not the panacea to all of healthcare’s problems, but in the hands of a strategic leader, telehealth is a formidable weapon to offset (or at least diminish) the effects of the many battlefronts that healthcare leaders find themselves fighting in these days.
If your organization does not have one yet, the first step is a sound Telehealth Strategy that outlines WHY the organization is investing in telehealth and HOW telehealth will provide a positive impact on the bottom line. From the resources section of our website, here is a set of articles and white papers to get you started with your organization’s Telehealth Strategy.
How is your organization consciously using telehealth to add to your bottom line?








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.








