At the core of every healthcare organization lies the mission to serve its patients by providing them with the care they need. In many cases, this care is provided by clinicians employed or affiliated with the hospital, health system, health center, or clinic. In some cases, certain clinical specialties are “outsourced”, most frequently for example in the ER.
With the increasing use of telehealth to serve more patients in a more timely manner, telehealth offers the ability to also increase the variety and the capacity of specialty services.
A Few Outsourced Telehealth Use Cases
Here are just a few of the many examples where organizations are using non-employee clinicians to provide their patients with the best care.
TelePsychiatry: Behavioral Health providers oftentimes have difficulty recruiting prescribing psychiatrists. Since the early 2010s, a multitude of vendors came into being that employ and manage psychiatric nurse practitioners or MD-level psychiatrists that operate exclusively virtually.
TeleStroke: Similarly, numerous neurology groups (sometimes as a standalone virtual only service, sometimes as part of a larger neurology group, or sometimes as part of a larger medical center) are providing TeleStroke evaluations to ERs where there is no neurologist on staff.
TeleCriticalCare: The model of a virtual ICU has been around for about 20 years, staffed “on the other side” by critical care nurses and physicians to enable smaller ICUs to keep and care for higher acuity patients.
TeleSpecialtyCare: Similar to Critical Care, access to cardiologists, rheumatologists, dermatologists, etc. can also be provided by numerous vendors and clinical groups that provide virtual access to licenses clinicians with varying areas of expertise.
TeleEmployeeCare: Household names such as Teladoc and AmWell (formerly known as AmericanWell) made big headlines for themselves as they went after the self-insured B2B market, targeting companies to lower their healthcare cost through virtual first model. Both organizations (and similar vendors) then shifted to offer their services to health systems for an outsourced virtual access to care — oftentimes with mixed results.
Selecting A Telehealth Service Vendor
In last week’s Telehealth Tuesday article I provided an overview on selecting a telehealth vendor.
I ended the article with this roadmap of activities which is the focus of this week’s article:
-
Verify the strategic, business & clinical case
-
Research the various service providers
-
Select a Telehealth Service Vendor
-
Onboard a Telehealth Service Vendor
-
Develop the numerous service workflows
-
Launch the new workflows
This process in itself differs from the standard way how organizations typically select and engage with a vendor in two key aspects:
The first critical and important distinction is to verify that outsourcing to a vendor is a sound idea (step 1). This is the first step where many organizations in the past have failed — and then blame the poor experience on the services vendor, when the whole idea did not make sense to begin with.
The second key distinction lies in the realization that in order to integrate the vendors’ clinical services, they have to be integrated into the existing care delivery workflows. This is a notion that is often overlooked, again leading to poor experiences for which once again oftentimes the vendor is blamed.
Verifying the Strategic, Business & Clinical Case
This first step is crucial and many organizations do not nearly spend enough time thinking it through, rather being oftentimes enamored by a brilliant sales pitch or by the stellar potential in one of these three areas.
The Strategic Case examines how the addition of the vendor’s clinical service aligns with and can support achieving the organization’s strategic objectives or — if it exists — the telehealth or digital health strategy. As they say, “Hope is not a Strategy” and for the outsourcing of care delivery to work well and sustainably, it needs to address one or more of the key strategic priorities. Otherwise the staff will not make the time to make it work.
The Business Case looks, realistically, at the short and long term financial return – not based on the vendor’s sales staff’s projections (ideally at this stage you haven’t even talked to any vendor yet), but on your own reality-based estimates of benefits and value, so you can better evaluate the requested fee structures of the vendor.
The Clinical Case assesses the clinical feasibility of the service. Obviously the service itself should be clinically sound, follow the standard of care (which you need to define here), and ultimately lead to better patient outcomes. Given the need for integration (e.g., through referrals or by simply requesting the service) you also need to build the clinical case to create the complete buy-in of the clinical staff that will be interfacing with the outsourced clinical service. Without it, utilization (and therefore the value) will be low.
Researching Telehealth Service Providers
Armed with the confidence that outsourcing to a vendor makes clinical, financial, and strategic sense, it is now time to evaluate at least 3-5 vendors on a number of aspects.
Questions to consider include:
-
Are they a standalone/virtual-only service provider or a service offering by health systems or academic medical centers?
-
What is the composition and experience of their executive and clinical leadership team?
-
What is their funding situation? Venture capital (VC) funded startups often are forced to grow big quickly and may require unacceptable minimum services; VC-funded startups also can also quickly close down when no more funding is available.
-
Reference clients and implementations are part of good due diligence, but take testimonials and others’ experience with a grain of salt — your organization, your culture and your service implementation/integration team will be different.
Selecting a Telehealth Service Vendor
The third step is pretty standard fare — establish contracts, agree on financial arrangements and how performance will be measured and reported.
We highly recommend that you insist on launching the engagement with a proof of concept first to validate all assumptions, especially around the three cases established in the first step.
Onboarding Process
Aside from the typical administrivia, here are a couple of additional considerations for the fourth step, the onboarding of the service provider:
Interview and onboard the vendor’s clinicians: While the clinicians providing virtual care to your patients are employed by the vendor, ensure that your clinicians and especially your clinical leadership get to know those clinicians and share with them your organizational and clinical culture and value — because from a patient’s perspective these are “your” clinicians.
Establish access to your EHR: In most cases, the documentation of the patient care by the remote, outsourced providers should be documented in the EHR for continuity of care and care coordination. If the vendor is insisting to use their in-house EHR and is offering “integration”, you’d definitely want to validate that integration with your clinicians, by reviewing the “imported” data.
Ideally you can provide the virtual clinicians access to the EHR or, at a minimum, ensure that the clinical notes are also made available in your EHR if the service provider requires their clinician to document the encounters in their own EHR.
Designing Integrated Telehealth Workflows
This fifth step is truly the “secret success sauce” to make an outsourced clinical telehealth service work for your organization and your patients.
Here are the various workflows to consider and to design:
-
Referral process — how will you refer patients to the outsourced service?
-
Scheduling — how will you schedule patients and clinicians?
-
Onboarding (new patients) — how will you handle new patients differently than established patients?
-
Rooming — how will the virtual visit be started? are patients coming into your clinic to virtually connect to the virtual provider? are patients at home? is there someone from your staff or the services vendor’s staff that first meets the patient? is there a copay collection before, during, or after the visit?
-
Visit & clinical documentation & billing documentation — what is the proper protocol by which you want the virtual clinician to provide the care, as defined by your clinical leadership? how does the visit need to be documented in your EHR for clinical and billing purposes?
-
Post-visit & follow-up — what happens right after the virtual visit? will someone from your organization follow up with the patient? what communication is the services vendor responsible for? what happens in the following days, weeks? is there standard communication?
-
Billing — what documentation is required for billing (see “visit” above)? who is collecting the co-pay (see “rooming” above)? who’s billing whom (see “contract negotiations” above)? what other financial payments between your organization and the vendor are triggered by a patient visit in either direction?
For more information see the article ”Telehealth and the 7 Thworfs”. While that article focus primarily on in-house provided video visits, the principles still apply.
Launch The Outsourced Service
Finally, it is time to pull the trigger and let the newly engaged clinical care partner handle the first set of patients. Here the primary considerations are a Change Management mindset, focus on Training, designated Support and continuous Accountability.
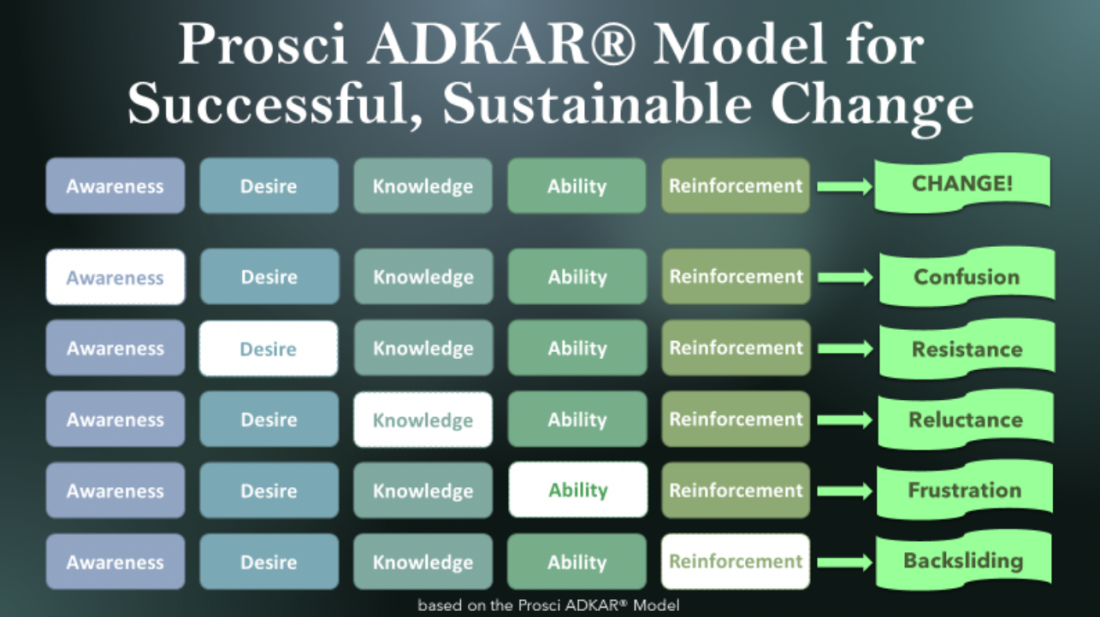
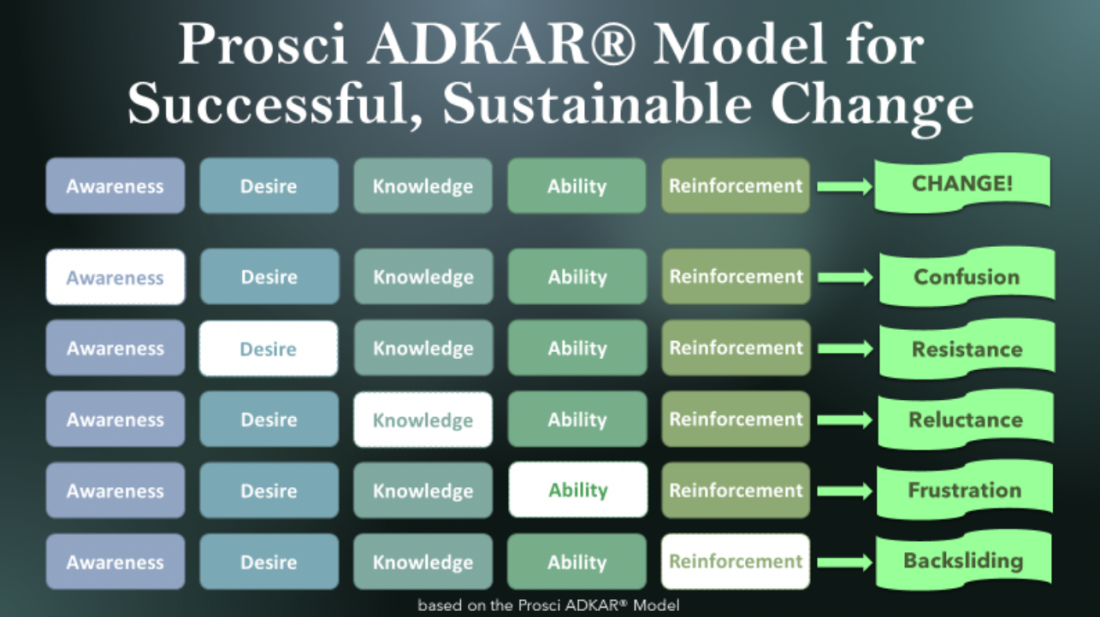
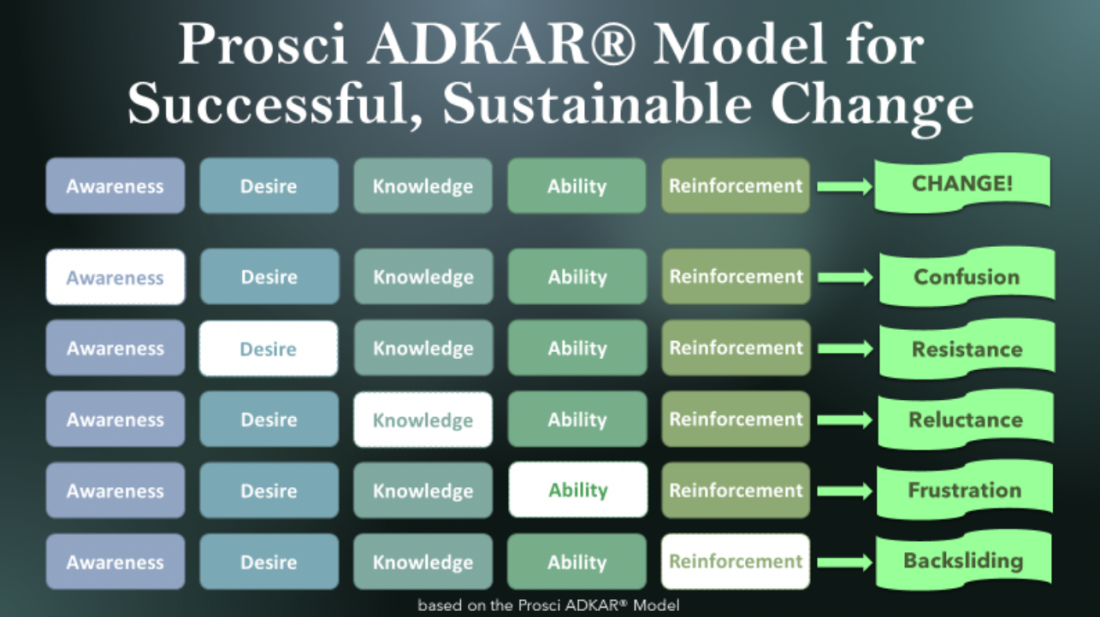
Change Management — For a successful deployment, it is crucial to understand the integration of a new telehealth service as an exercise in change management. Change is oftentimes uncomfortable to some and scary to others. One proven change management model is the ADKAR model for successful, sustainable change. For more information see the article “Telehealth Success through Conscious Change Management”.





Training — workflow deployment mostly happens through the review of the workflows (if the users were not involved in the design of the new processes). This can include the review of the various happy day scenarios (what will happen 80%, 90% of the time) and the alternate scenarios (things that are expected to happen and how to react. Training mostly focuses on providing the Knowledge and the Ability for users to follow the new process. For more information see the article “A Proven Recipe for Telehealth Workflows”.
Support — the successful rollout of a new process depends on the availability of support if things do not go as planned. This includes administrative, operational, and logistical support as well as technical support.
Accountability — last but not the least, in order to ensure success leadership must “trust but verify”. This is also the final step in the ADKAR model, which requires the provision of accountability to ensure that the newly implemented services are actually being used as intended in order to provide the promised or expected value.
Successfully Outsourcing Clinical Telehealth Services
Armed with the knowledge covered in this article, you should be well prepared to select and integrate your own outsourced telehealth service.
Next week, we’ll cover three other types of Telehealth Service vendors: Telehealth Staffing Vendors, Telehealth Law Firms and Telehealth Consulting Firms.
Don’t want to go at it alone? Then reach out to us to explore how we could coach, advise, or consult on your idea to expand your clinical care offerings for your patients.










To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.








