Sometimes it’s a good idea to go back to the basics, the fundamentals. To go up to the 100,000-foot view and take a look from a distance, with a fresh eye, an outsider’s perspective.
So after over 175 editions of Telehealth Tuesday, I’m answering the simplest of all questions:
What is Telehealth?
Telehealth Defined
After way too many committee meetings at the Mayo Clinic, at which the previous meeting’s topics (or even decisions) were frequently rehashed, I arrived at two insights:
“Everybody agreed, until somebody wrote it down.”
“Everybody agreed, until somebody defined it.”
So before we start talking about telehealth (or telemedicine, virtual care, connected care and other synonymous phrases) let’s start with a definition.
While many different (and elaborate) definitions of telehealth exist, I’ve been going with this simple yet all encompassing definition:
Telehealth: “Delivering Care at a Distance”
As such, Telehealth encompasses all interactions that patients have to receive their diagnosis or treatment without having to set foot into the clinic.
A close cousin to telehealth (well, actually the descendent) is telemedicine, which focuses on clinicians interactions with patients:
Telemedicine: “Practicing Medicine at a Distance”
As depicted in the simple taxonomy below, telemedicine includes the various different modalities such as interactive patient care (e.g., video visits or secure messaging), remote physiological monitoring (periodic recording and transmission of vital signs, e.g., blood pressure or weight), and store and forward (e.g., faxing an EKG to a cardiologist or using a TeleRadiologist).
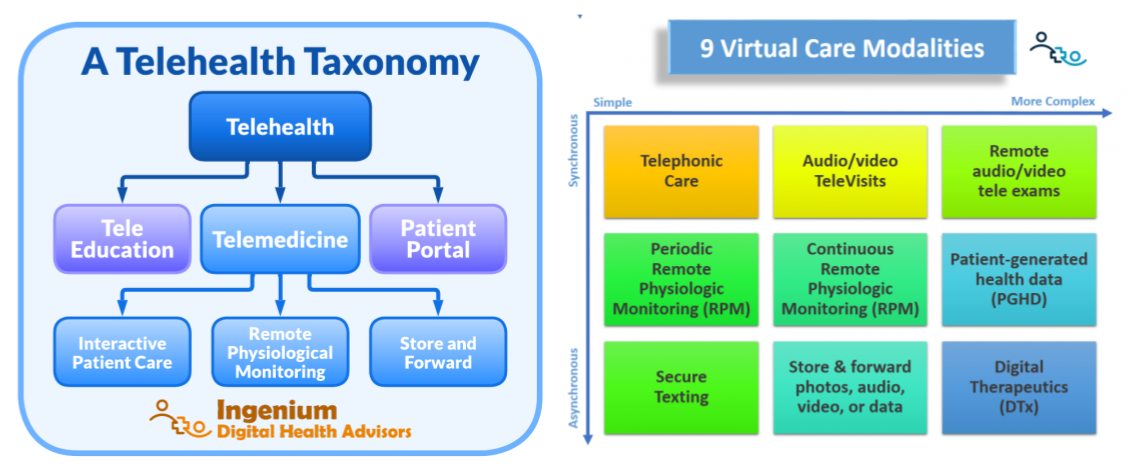
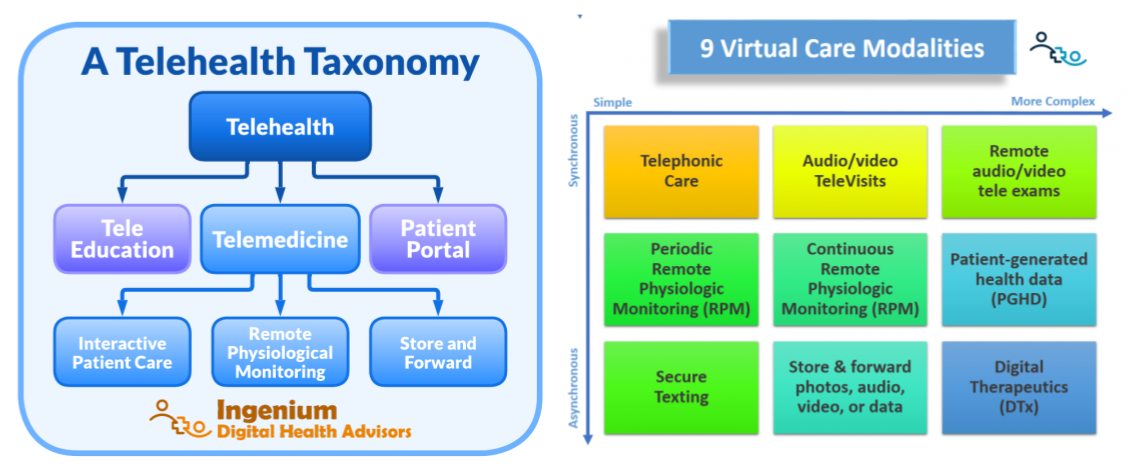
As can be seen in the chart of the virtual care modalities, telemedicine now includes a broad array of modalities by which providers can diagnose and treat patients “at a distance”. The whole world of digital health (including digital therapeutics) is only going to expand that more in years to come.
With the definition out of the way, let’s focus on another answer to the question: What is telehealth?
Telehealth is a Clinical Tool
The definition we use for Telehealth already connotates it, but it bears repeating: Telehealth is not about the technology, not about “by means of telecommunications technology” as is often embedded in other definitions. No, telehealth is about delivering care, which emphasizes an important distinction which is often forgotten:
Telehealth is a clinical tool.
Telehealth is not a set of technologies nor is it a Covid-19 stop gap measure.
Telehealth is a care delivery method as an alternative to in-person care. It can be used for health maintenance, for diagnosis, and for treatment. With the right training on virtual physical exams, it can actually be used in way more circumstances than most clinicians are currently comfortable with.
As a clinical tool, telehealth should be wielded by clinicians. I.e., it should be up to the clinician to decide whether this modality of care delivery is appropriate for the patient.
As I’ve written about before, 100% telehealth (especially video visits) means that you deliver care via telehealth every time when three criteria are met: (1) it’s clinically appropriate, (2) the patient wants it, (3) the patient has the technical capabilities to do it.
Telehealth as a Strategic Tool
While telehealth is first and foremost a clinical tool, it has also increasingly become a strategic tool — i.e., a tactical tool that healthcare leaders can employ to help achieve most if not all of its strategic objectives.
Here are a few examples from the 6 pillars of a typical healthcare strategy:
- People – telehealth can contribute to the retention of existing staff and the recruitment of new staff, especially those who want to stay up to date on the latest technologies, with a long career still in front of them. Telehealth also offers easier opportunities to work remotely from home or to work part time.
- Finance – telehealth can open up new revenue streams, avoid losses from cancellations and no shows, and be used (through RPM) to avoid readmissions or to achieve population health goals in value-based arrangements.
- Service – The availability of telehealth services is always a delighter to patients, and never a detractor, as long as in-person is still an option for those who prefer it. Over time, the ability to do telehealth will become the default expectation of the modern healthcare consumer.
- Quality — When clinical quality is dependent on patient’s follow through, then frequent touch points can be used to create patient activation. Telehealth is a great set of tools to provide feedback to patients (e.g., through remote physiological monitoring), provide health coaching (through video calls) and regular touchpoints (through secure messaging and tele education).
- Community — many health systems, health centers, and behavioral health agencies serve a wide geographic area. By given patients the option to stay in their community (i.e., by eliminating the need to travel) healthcare organizations are now virtually providing a “local” community service, reduce miles traffic (and resultant traffic fatalities) and sometimes even keep “shopping dollars” in the hometown.
- Growth — Last but not least Telehealth can greatly contribute to growth through the many facets already outlined above: expanding the geographic reach, recruiting more clinicians, keeping clinician schedules filled, etc.
Telehealth is Here to Stay
In the spring of 2014 I was invited to speak at the annual conference of the Mid-Atlantic Telehealth Resource Center (MATRC, matrcsummit.org) and daringly thought it would be cute to render my own version of “Our love is here to stay” with the lyrics “It’s very clear, Telehealth is here to stay.” Thankfully I was not escorted from the stage, but there were also no Grammy’s handed out that day…
Little did I know back then, that 6 years later we’d get a boost for the adoption of telehealth through a deadly worldwide pandemic. But even before it was well understood by everyone (even those who have worked tirelessly on telehealth adoption in earnest since the mid 1990s).
But by now the world has seen and experienced how much of care delivery can actually be done “at a distance” — and patients, as service consumers, are all about convenience and whatever can save them time and money.
And, as I’ve written about numerous times, non-traditional competitors are fully invested in digital health and telehealth. The “virtual first” model is also promoted by many healthcare insurers and larger clinics as well. The days of outpatient brick-and-mortar clinics are counted. And Telehealth? Well…
It’s very clear, Telehealth is here to stay
not for a year, but ever and a day.
The internet may crumble, the ATA may tumble,
they may soon make way,
But, Our Telehealth is here to stay.








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.








