For the longest time, physicians have been paid on a procedural basis: render a service, perform a task and get paid for it. Just like in the old horse and buggy days, from house visits that were paid with a meal, goodies from the farm, and whatever the family could afford, to cash pay for hospital procedures and office visits.
The introduction of healthcare insurance almost 100 years ago further reduced care delivery into a mere set of tasks and procedures with differing dollar amounts attached to it based on the qualifications of the one doing the task, an accounting for the consumables, and some vague recognition of the relative value of one task over the other.
About 30 or even 40 years ago, when with the advent of new scientific breakthroughs, new treatment options, and new technologies the cost of care spiraled out of control, the idea of “value-based care” was born. What if instead of “sickness care” we could pay healthcare providers for keeping patients healthy, for keeping them out the hospital, out of the ER, or shorten their stays in nursing homes? What if we could financially reward positive outcomes, vs. financially rewarding more procedures and more tests?
These days, most value-based contracts focus on capitated payments: assign a certain class or group of patients with the mandate to manage their care cost and cap the cost on a “per capita” basis, based on historical statistical analysis of what such a cohort would traditionally cost to care for. If the total cost of care for the total assigned population is lower than predicted, the healthcare organization can keep the money (at least most of it). If the actual cost is higher, that extra money has to come out of the healthcare organization’s pockets.
Activating Patients
The overall goal of value-based care is to keep people healthy, prevent the utilization of costly care, and eliminate the use of unnecessary care.
While I’m no clinician or epidemiologist, I’d venture it’s fair to say that for the majority of today’s illnesses the biggest contributing factor is the patients’ lifestyle: sleep, exercise, nutrition, stress and emotional well being. In short, in order to prevent the progressive decline of patients’ health over months, years, or decades, we as a health system must find ways to motivate patients to actively participate in and contribute to their well being. Yes, drugs, and surgeries are necessary – but, as they say in mathematical proofs, not sufficient.
As I’ve written about before, the participation of patients in their care has undergone quite the evolution over the last 25-30 years. From the early days of “compliance” (doing as you’re told) and “adherence” (sticking to the plan you’ve been given). over the past 15 years we’ve shifted our conversation to “engagement”: getting patients to find the motivation within themselves to proactively take steps to improve their health, to take a personal interest in the changes they need to make vs. simply relying on medications or procedures.
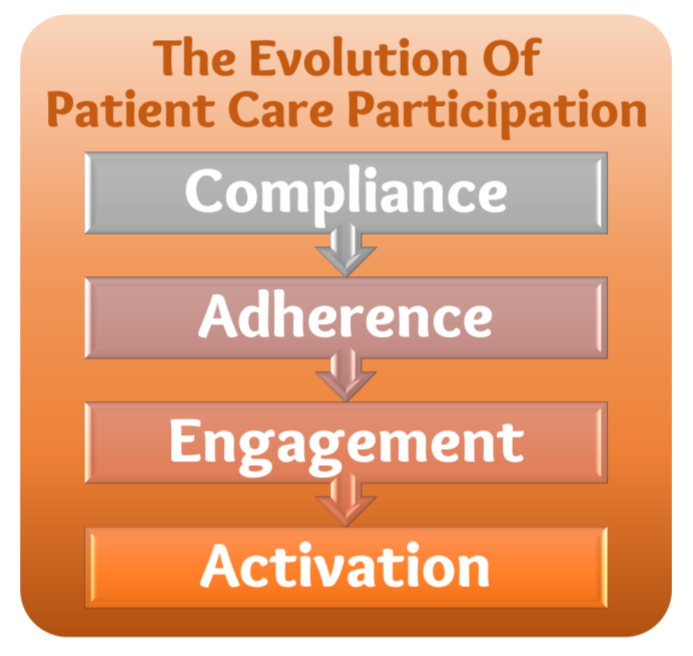
But ultimately it is the Activation of Patients that we need to be after: as a healthcare system, we need to empower and support and encourage patients to take an active and proactive role in making sure they get health and stay healthy.
Knowing, Doing, and Belonging
One of humans’ deepest desires is belonging. It’s probably hard to measure, but I’d venture to guess that loneliness kills more people than any other disease. One of our deepest needs as humans is to be heard, to be understood, to be listened to, to be taken seriously — to be loved. But our 90+ year history of fee-for-service coupled with a 30-year-old sometimes brutal fight to optimize care delivery and cut cost have turned the delivery of care for the most part into a cold, faceless, rushed service production system.
So if we want to restore people’s health and keep them healthy, we must create a sense of belonging — or actually a sense of (real) caring. And not just once every four weeks, or even once a week. No, to truly demonstrate that we care, to give our patients a sense of belonging, we must do so daily or even multiple times a day.
Before you fall into the fee-for-service trap of “but that’s too expensive”, let me cover the other two elements under this section’s heading, Knowing and Doing.
With preventive care and population health management, today’s healthcare has amassed tons of resources (most of them good or great) that should help patients to take care of their conditions. There are books and videos and recipe guides and exercise regimens and free health coaches that come with employers’ health plans, etc.
No patient who is at least a bit curious and involved in their self care, can claim they do not know what they should be doing. It’s actually the doing that is the hardest part, also known as the “Knowing/Doing Gap”. Which is why in a value-based environment, beyond the clinical care the care team also needs to provide support, encouragement, and accountability for the “doing” part of the patients.
So here is the perfect environment I envision: when we provide patients with the right knowledge (and in the right, small doses); when we let them know through our words and actions that we care, that they belong; and when we then support them and hold them accountable to put the knowledge into action: then we can — coupled with the traditional clinical expertise, medications, and procedure — make a real difference in the health and outcomes of those patients.
Virtual Care is the More Cost Effective Care
As a systems engineer I hold in high esteem to two core tenets: to find the most effective solution for a set of requirements and constraints; and to consider the impact of the solution in the context of the overall system.
On the latter point, we cannot simply look at the cost of care by only considering the expenses incurred by the healthcare delivery system. For a true value-based care value proposition, the societal cost borne by the patients needs to be taken into consideration as well.
In our traditional in-person care delivery environment, these costs are enormous. Starting with the patients’ and caregivers’ transportation cost and the overhead time it takes to go and see a clinician. Add to that the cost of lost wages or child care. While the visit may not “cost” the patient anything due to their commercial, Medicaid, or Medicare insurance, they still pay a high “system cost” for receiving care, preventing many from doing so more frequently.
So let’s talk about virtual care. And with virtual care (“delivering care at a distance”) I don’t just mean video visits. As I will lay out in the section below, this also includes the types of communication styles that nowadays we frequently use with our loved ones and friends: phone calls and texting. Because in order to create a sense of belonging, to demonstrate caring, or to provide compassionate accountability we need to communicate with patients and do so frequently — and we shouldn’t have to wait for them to come into the clinic to do so.
When you set up virtual care such that it provides a continual stream of interactions — a message here and a quick phone call there — then virtual care can create deep, effective connections between the patient and their care team. Which in turn can motivate patients and awakens their desire to actively participate in their care.
5 Virtual Care Modalities to Activate Patients
To provide truly effective value-based care by tapping into the power of virtual, we need to first redefine virtual care in this post-Covid world as more than video visits (or phone visits). We should no longer need to ask ourselves whether we can get paid for a service, but whether the service will create a stronger connection with the patient, whether it will compel the patient to actively participate in and contribute to their well-being; and whether it ultimately leads to better outcomes. Only then can we open the door partnering with patients and being there for them and with them.
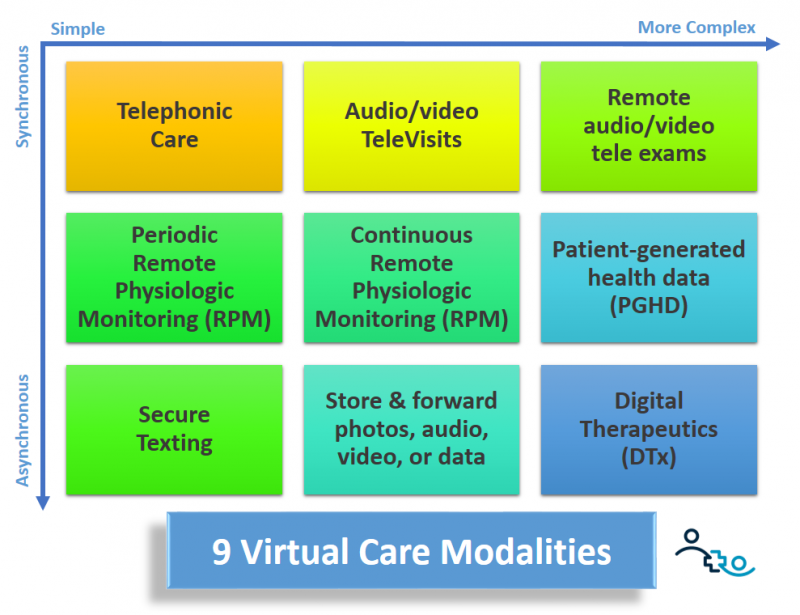
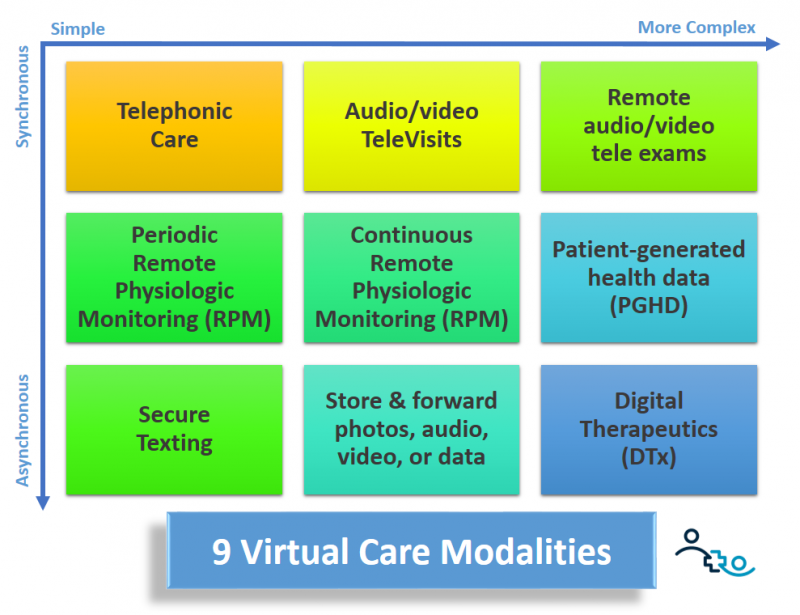
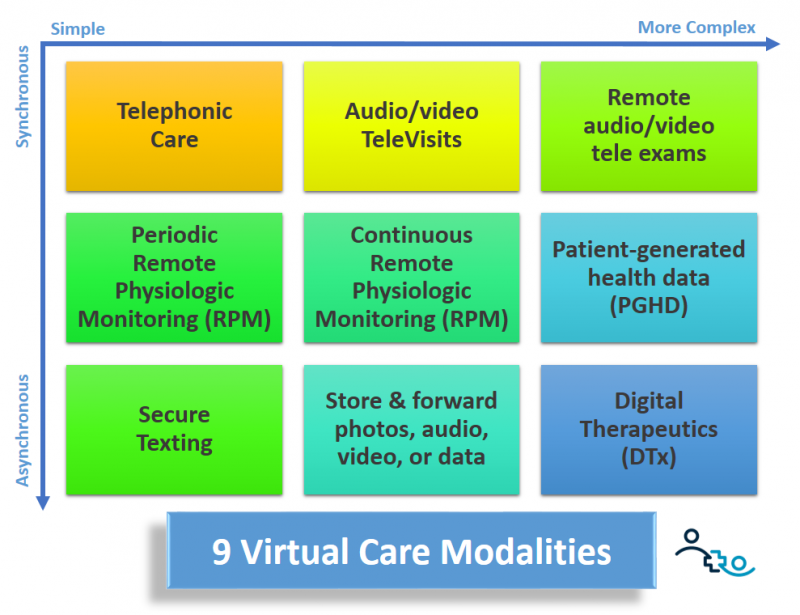
Of the 9 virtual care modalities that I laid out in a previous article and in the graphic above, there are 5 that play the most important role in a value-based care environment:
Phone: The phone has had for decades a longstanding role in the most dedicated clinicians toolkit to make sure their patients are okay. In a world freed of fee-for-service thinking quick 1-2 minutes check ins with the patient by anyone on the care team can now become the norm. For not-so-tech-savvy folks, this is still their preferred way to communicate with their friends and family. To prevent overuse from the patient side, systems have to be put in place that allow the care team to take more control over the timing of the phone-based interactions.
Secure Messaging: While texting and chatting have now become ubiquitous for most of our daily interactions, healthcare has long had a big problem with text messages. On the one side there are security and privacy concerns and many clinical message systems are therefore put behind a user-unfriendly web-based portal wall. Better solutions exist for Smartphones and Tablets to make it as easy as a chat with the family but as secure as it needs to be.
On the other hand there also have been in the past concerns about overuse and unpaid clinician time, since some patients can get very verbose or demanding. But even if they are not, with no payment in a fee-for-service world, clinicians would rather not have to handle 20+ messages at the end of their already busy day.
But in a value-based environment that time spent is valuable – though here as well safeguards and processes have to be put in place to keep the interactions valuable and focused on health outcomes and not as a substitute for counseling.
Video Visits: Video obviously adds a full layer of richness to the communication between the care team and the patients. 85% of all communication is non-verbal and video with a picture and better sound allows clinicians to pick up on many more cues, enabling them to provide better care and establish better personal rapport than over the phone. In addition, the video element also creates more trust and more connection from the patient’s perspective.
Again, in a non-fee-for-service world video visits don’t have to be 12 minutes. They can be ad hoc and may only last 3-4 minutes to answer the patient’s questions or give them guidance on some changes they need to make.
Remote Physiological Monitoring (RPM): For most chronic disease management scenarios insights into the patient’s vital signs such as weight, blood pressure, heart rate, pulse ox, glucose levels, temperature, etc. are key, especially when most of their care interactions do not require patients to come into the clinic. But not only does RPM give clinicians insights — failing to adhere to the care plan is usually reflected adversely in some of the physiological parameters, e.g., weight gain, unmanaged blood pressure or glucose, etc. This deviation from the patient’s desired normal provides excellent just-in-time teaching opportunities which increase “knowing” and provide opportunities to support “doing”. For more information peruse the numerous articles where I’ve written about RPM.
Digital Therapeutics: Digital Health innovation (including tens of thousands of “Apps”) has been funded to the tune of $100 Billion of venture capital money over the past 10-12 years. There are now a number of vetted and validated digital health solutions that can augment traditional care plans across a wide spectrum of ailments – from tinnitus to insomnia, or from hypertension to physical therapy: You name it, there’s “an app for that”.
Value-based patient population are the prime opportunity for healthcare organizations to start dipping their toes into these novel Digital Health tools, because like it or not, they will become the norm to augment traditional care, even if that care is delivered virtually.
Back to the Roots of Whole Person Care
When care for patients is provided in a comprehensive way that not only addresses the body (medical care) and the mind (behavioral care), but also reaches the heart of patients (compassionate care), then we have come more then full circle back to our roots when house visits and doctors that treated the whole person were the norm.
And virtual care can help us get back there again.








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.








