With a systems engineering mindset I first look at the challenges at hand in the context of the larger system – what happens before, what happens after? Who else is involved, who else is impacted? How do the various “sub systems” impact and affect each other?
To design the best solution, engineers must take into account and weigh against each other the needs of key stakeholders including the users, the various functional requirements, the constraints, the technical limitations. Designing a solution is often an exercise in seeking sustainable compromises to satisfy as many requirements as possible.
In project management, project managers often like to “hide” behind the triple constraint of scope, time, and budget: you can have two of them fixed, but not a third one. With a timeline and a budget, there is only so much scope we can tackle. With a fixed scope and fixed timeline, we will have to bring in more people or better, more expensive people. But oftentimes it is a cop out. It’s not creatively looking at way to satisfy all requirements.
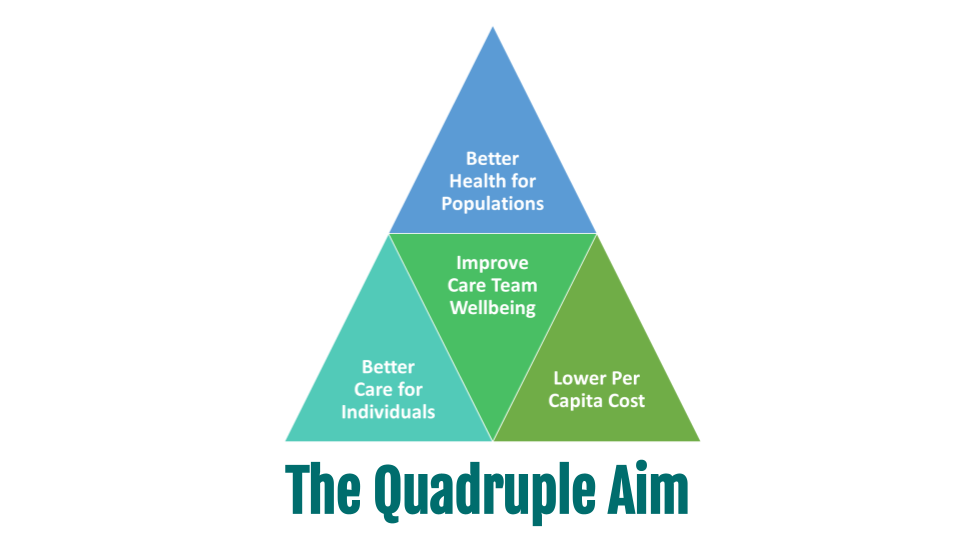
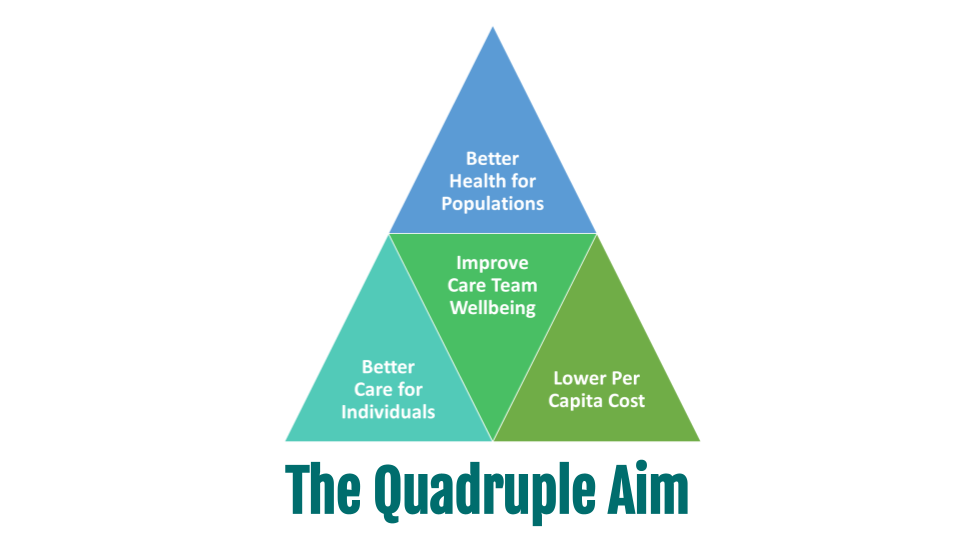
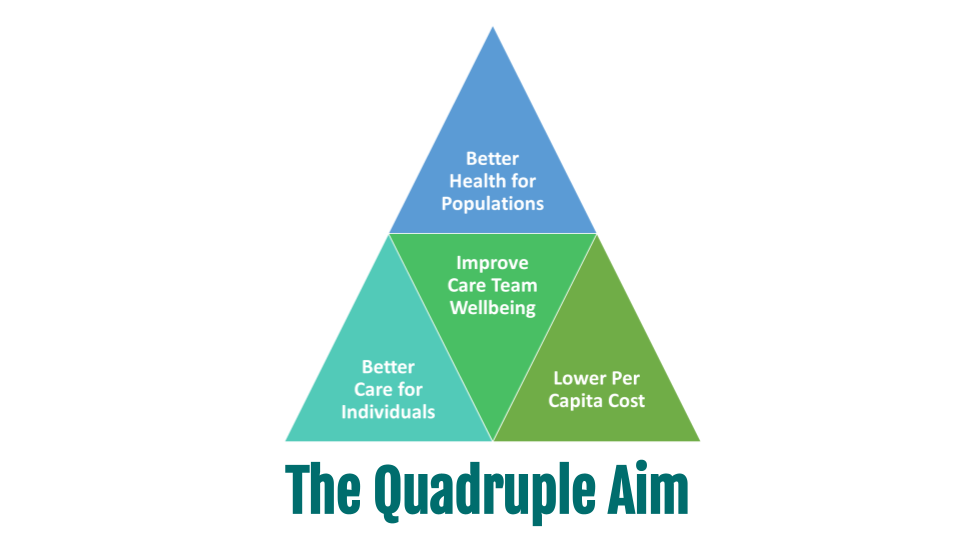
Healthcare’s Quadruple Aim
Healthcare, like project management, has its own “triple constraint”, albeit nowadays mostly in the form of a quadruple aim.
About 20 years ago, the Institute of Medicine in its landmark report “Crossing the Quality Chasm” suggested six “aims for improvement” which were then simplified by the Institute of Healthcare Improvement (IHI) into a triple aim of healthcare:
-
Better Care for Individuals
-
Better Health for Populations
-
Lower per Capita Cost
Soon thereafter, others added a fourth one, which especially in the wake of the Covid-associated burnouts rings very true:
4. Improve Care Team Wellbeing
Our mission at Ingenium is to enable the sustainable delivery of extraordinary care, and from our perspective, extraordinary care is care that satisfies all four aims.
To achieve our mission, we apply a multi-pronged approach: defining and training on well thought through processes that not only prescribe what usually should happen, but also clearly lays out what happens when things are not as usual; keeping a user-centric view of the mindsets of the care delivery team and the patients; and providing well-configured, highly useful technologies to aid in the delivery of care.
Patina: A systems approach to Primary Care for Seniors
In this context, it was refreshing to come across an article (sent to me by one of Telehealth Tuesday’s readers) about Patina Health, a provider of primary care to seniors in their home.
While there are many home-care agencies, Patina focuses on actual primary care – delivered both virtually and, if needed, in person to patients in their home. Because, as they state, this is about seniors getting the care and the dignity they deserve. When you’re sick, contagious, not feeling well, and can’t get around easily — dragging yourself to the doctor’s office is not a very dignified experience and Patina understands that.
As I wrote about last week, virtual care with all of its modalities can truly make a difference in a value-based care business model and Patina is using a similar approach of “technology-assisted-first” care in a medicare advantage business model.
The leadership team of Patina, by the way, is headed by someone who already was at the frontlines of an earlier attempt at revolutionizing care delivery: CEO Jack Stoddard briefly served as CO for the joint venture of Amazon, Berkshire Hathaway, JP Morgan Chase formed in 2018 to create “better outcomes, greater satisfaction, and lower costs for their U.S. employees and families”. Do those aims sound familiar?
Patina is in a sense no different than Haven – only that the target patient population is not the (mostly) healthy workforce, but the population with the most chronic diseases, most comorbidities. A challenge that can be costly and not for the faint of heart.
From my perspective, the cleverness of their business model lies in aligning themselves with the clear objectives of the next generation of Medicare Advantage plans that are “highly motivated” to keep costs down — and are increasingly realizing that patient experience and patient satisfaction are driving outcomes (i.e., patient activation).
And if you’re looking for “social proof” that they’re onto something, they are backed by a $50M Series A round led by venture capitalists such as Andreessen Horowitz (a16z), Google Ventures (GV), F-Prime (Fidelity’s VC arm) and more.
According to the article about them, they first partnered up with Independence Blue Cross Blue Shield in Philadelphia, and have now established partnerships with United Healthcare, Cigna, and Aetna. Seems like everybody wants in on the game.
Delivering Multi-Modal, Technology-Enabled Care
Patina’s care delivery model includes a three-pronged approach of virtual visits, phone calls, and at-home visits. And I’d venture to guess they are also integrating remote physiological monitoring in their “virtual care” services.
What Patina is addressing is what health plans have never really implemented: care coordination and continuity of care, two of the core quality of care hallmarks at my “healthcare experience alma mater”, the Mayo Clinic.
Many health plans have launched and are marketing a number of offerings — from telehealth and urgent care to health coaching and remote monitoring equipment. But few, if any, of these services feed into the primary care doctor’s EHR and thus provide patients with a very fragmented care experience that may be cheaper in the short run, but will prove much more costly in the long run.
My perspective is that most MCOs grew out of traditional healthcare insurance plans, where typically there is not so much long-term concern about caring about the patient until the end of their life. Unlike, e.g., in Germany, where patients typically stay with their health insurance for life, even though they can choose from about still five dozen options today. And unlike in MCOs, where poor care provided in the 60s (or the lack of care provided) can lead to severe illnesses in the 70s and 80s, most health plans lose their patients when they switch employers or switch over to Medicare.
The Future is already here
I often like to quote author’s William Gibson’s “the future is already here, it’s just not evenly distributed” and it applies here as well. Patina’s model is a sign of things to come, paving the way for the future in a large-scale proof of concept.
While Haven (surprisingly still in existence), Amazon Clinic (which replaced Amazon Care), and others are aiming at lowering the cost of care for employees, Patina (and I’m sure dozens more) are focused on tapping into a multi-pronged approach that includes virtual care to ensure continuity of care and care coordination.
And therein lays the near-term challenge and threat for many traditional primary care practices that are not fully embracing virtual options for their Medicare population: that Medicare patients enrolled in a programs such as Patina will no longer visit their clinic, thus further eroding the already fragile business model, especially that of primary care in rural America.
It is thus time for all of us in healthcare to reinvent our care delivery model that is truly optimized for a great care experience and better outcomes at lower cost.
Do you know the leadership of a primary care clinic that has not fully embraced virtual care? Maybe it’s time for a talk with us about what can be done about that. Otherwise in a few years they may not be around.
P.S.: This article marks the final article in the 4th year of Telehealth Tuesday. Next Sunday, October 8, Telehealth Tuesday will enter its 5th year. Stay tuned for a “best of” top 10 list or nominate your favorite article here.








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.








