Check out this USA Today series on the full scope of the problem.
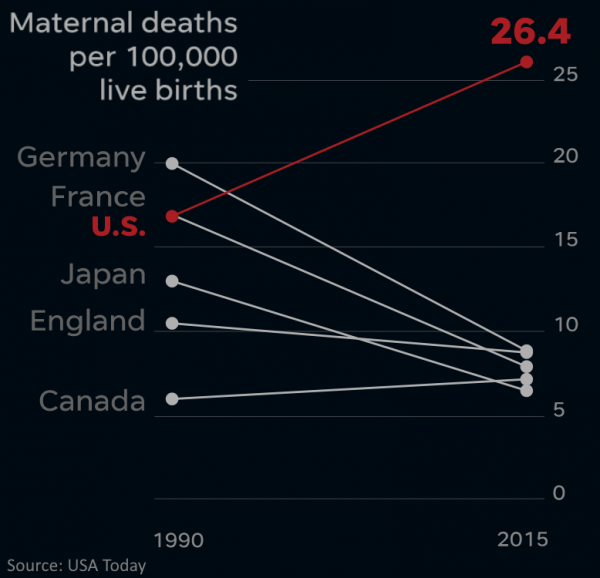
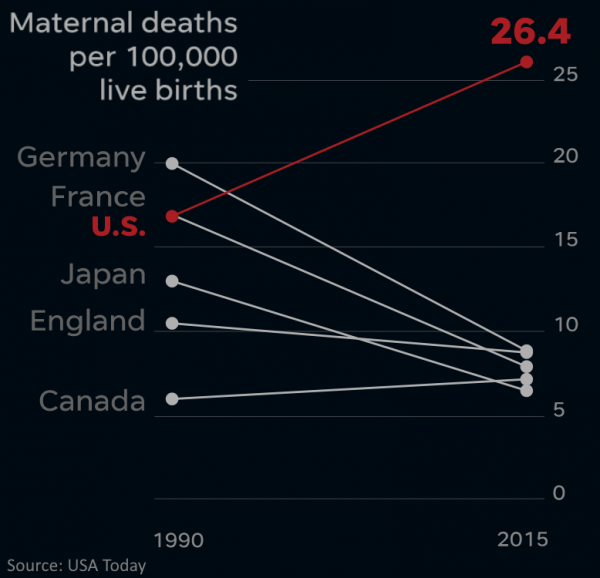
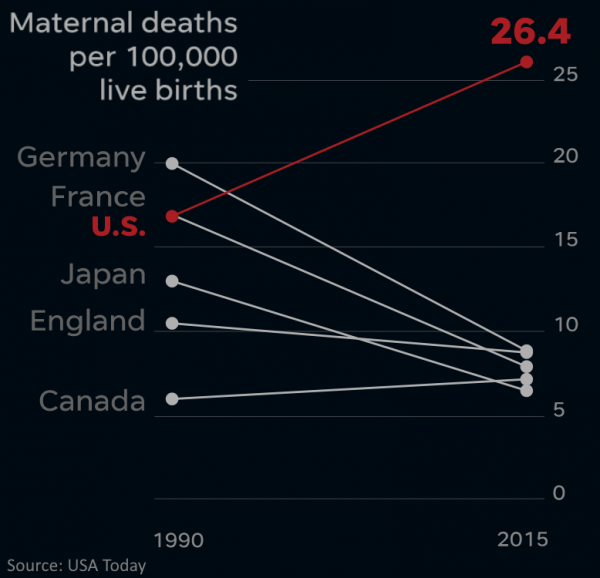
Of course the root causes for this are manifold and as much as I’m passionate about telehealth and it’s parent, Connected Care, as tool to enable the delivery of extraordinary care, it’s obviously not a panacea for the underlying conditions that are producing this crisis: including a shortage of midwives, shortage of qualified Maternal Fetal Medicine experts, widespread health conditions (obesity, diabetes, hypertension) in young women, and a rise of the age of the women being pregnant.
But if telehealth is good at one thing, it is to improve the possibility for timelier access to care, the possibility of detecting threatening conditions earlier and being more likely to stay on top of the expecting mom’s health.
The Vision of Connected Care
The simplest definition of Telehealth is to “Deliver Care at a Distance” and we define Telemedicine as “Practicing Medicine at a Distance”, with these two services falling under the larger umbrella of Connected Care.
In turn, the best definition of Connected Care is to describe it by its primary goal: To help achieve Empowered Wellness — to provide people with the ability to be well, get well, and stay well by taking advantage of digital health and distance care solutions.
So how does this apply to Maternal Health?
Oftentimes complex problems can be addressed by simple yet comprehensive solutions. Within the realm of Connected Care, there are a number of tools available to get care to and take care of patients — including expecting moms.
Here are nine different relatively simple Connected Care tools that are available for maternal health care:
- Telephonic visits for quick check ins
- Live audio/video visits (“televisits”) with and without exam tools
- Text-based, secure communication — for asynchronous interactions
- Remote Physiological Monitoring — the periodic and continuous monitoring of vital signs such as heart rate, heart rhythm, blood pressure, weight, glucose, etc.
- Store & Forward — the capture and transmission of electronic information, mostly medical imaging such as photos of the skin, EKGs, or radiological tests.
- TeleEducation — just-in-time and on-demand information around diagnoses and self care
- Patient Portal — scheduling appointments, viewing notes and lab results and secure messaging
- Personal Wellness — apps and other devices to track and maintain personal wellness (from activity trackers to mindfulness apps)
- Health Information Portability — sharing of health records and other information across different care providers
In a comprehensive approach to providing maternal health care, each of these 9 tools can be leveraged to ensure the best care possible.
Common Connected Care Use Case in Maternal Health
So how can you leverage these 9 tools during and after pregnancy, especially for those moms that, for a variety of reasons, may not be able to see the OB/Gyn as frequently as needed?
Here is a sample of 21 uses for connected care that can be set up relatively easily:
- TeleEducation (#6) on pregnancy care
- Routine pregnancy care video visits (#2)
- Perinatal 24-hour helpline via phone (#1) and text (#3)
- Telephonic (#1) check-ins
- At home nonstress tests (#4) with novel fetal heart rate measurement solutions
- Care navigator / social worker secure messaging (#3) and video visits (#2)
- Remote physiological monitoring (#4) for higher-risk pregnancies
- Urine Dipstick Tests (#3, #4 or #5)
- Postpartum depression screening (#5, #6)
- Telebehavioral health counseling (#2, #1)
- Telepsychiatric treatment (#2, #1)
- Remote chronic care management: physiological monitoring (#4) and video visits (#2)
- Postpartum follow up visit (#2)
- Pediatric televisits (#2)
- TeleLactation education (#6)
- TeleLactation consultation (#2)
- Remote nutrition education for individuals or group (#2 and #6)
- Medical interpreter translation services (#2)
- Public health nurse video visits (#2)
- TeleMentoring (doctor to doctor) with MFM specialists (#2 combined with #9)
- Project ECHO for community primary care specialists
Given the high maternal death rate, especially high-risk pregnancies require increased attention. Here some of the most common conditions and risk factors that occur during pregnancy and increase the risk of complications:
- Gestational Diabetes — diabetes that presents after the onset of pregnancy in otherwise non-diabetic moms. Here glucose monitoring (RPM, #4) along with proper education (#6) and potentially access to nutrition counsellors via video visits (#2) can assist.
- Gestational Hypertension — another condition triggered by the pregnancy, again aided by blood pressure monitoring (RPM, #4) with education (#6) and periodic discussion (#2)
- Preeclampsia — a combination of hypertension and increased protein in the urine that can be detected and managed via blood pressure monitoring (#4) and urine dipstick tests (#4 or #5).
- Fetal Growth Restriction is a condition where the fetus is not growing at the expected rate. This can be detected by instructing the mom to take and report the fundal height (#3 or #4).
- Multiple Gestation (i.e., twins, triplets, etc.) — a pregnancy with more than baby at time which would warrant more frequent check-ins (#1, #2) and potential RPM (#4) if other conditions mentioned above develop.
- Pregnancies with Comorbidities – such as chronic hypertension, diabetes, obesity, etc. which also would warrant increase remote physiologic monitoring (#4) and frequent visits (#2) and check-ins (#1).
Connected Care is Not Futuristic
As you can see from the list, the use of connected care tools is not as futuristic as one may think. A solid set of proven tools from video visits to remote physiological monitoring can do wonders for improving the conditions for mother and child.
Many moms, especially those working multiple jobs, being a single mom, or living more than 30 minutes away from their OB/Gyn provider can greatly benefit from receiving “care at a distance” that can empower their wellness.
Next month I’ll be working with a HRSA-funded program to improve maternal health by establishing a perinatal telehealth network that will include access to MFM experts at the larger hospitals in the state directly from doctor to doctor as well as directly to the expecting mom’s home.
And the month thereafter, I’ll be helping a startup validate their comprehensive RPM solution that eventually will include a fetal heart rate monitor so that expectant mothers can conduct the 30-minute nonstress tests at home without having to come into a clinic.
As the American-Canadian writer William Gibson wrote “The future is already here — it’s just not very evenly distributed”: If you can think of it, someone in the US or the world is probably already doing it. Therefore we don’t necessarily need more innovation but, more importantly, we need an accelerated adoption and dissemination of innovation.
But that’s a topic for another Telehealth Tuesday column.








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.









Leave A Comment