Optimization is commonly defined as the act of making the best use of a resource. Optimization is also a mindset to continually improve: not to pursue perfection, but to continue to reduce wasted time or resources.
If we were living in a static world, optimization would be akin to putting the finishing touches on something: to buff and polish make minute adjustments and corrections to achieve the desired state. Alas since our world, especially in healthcare, is very dynamic, we constantly need to adjust and modify to keep things “optimized”.
In either case, you need a solid set of tools that can help you to optimize your telehealth performance. If you’re optimizing engine performance you need a special set of tools to do so. Same for optimizing an athlete’s performance (e.g., high-speed video recordings) or a singer’s performance (e.g., auto tune, reverb).
Basic Optimization Tools
To optimize the performance of telehealth at your organization, you need a solid set of tools. Telehealth affects and is impacted by at least a dozen teams – from scheduling to billing, from IS to networking, from compliance to marketing, from nursing to providers; including a number of leaders.
The first set of tools are your basic tools that would need in almost any kind of service improvement project: leadership engagement, optimization vision, and project management.
Leadership Engagement: Any optimization effort requires the support and engagement of leadership for a multitude of reasons. First off, optimization requires resources such as staff time and investments and it is typically leadership that okays or supports the spending of those resources.
Optimization Vision: As the old adage goes: “If you don’t know where you’re going, any road will get you there.”. Without a clear understanding of what optimization will look like when it’s done, the effort will probably be over the minute it begins. Without clear objectives, the team will not know what to focus on and when to declare success.
Project Management: Project Management can take on many different forms of formality and most improvement efforts do not require a lot of “project management” overhead. Still, with so many stakeholders involved and different people working on different parts, the communication created through project management is the glue that will hold the team together. Besides, if you’re failing to plan, you’re planning to fail, so Project Management can prove its value quickly very early on in the planning phase.
Essential Telehealth Optimization Tools
Simply put, an optimized Telehealth Service should like the phone or the building: you don’t even notice anymore that it is there. The next set of tools aim to improve the chances of quick success of getting your organization’s telehealth offerings to this experience. The essential tools include:
- A Vision for Telehealth’s place in your organization
- Clinical Leadership to ensure acceptance across all providers
- A Telehealth Performance Measurement System to know where you are
- A Telehealth Governance Team to provide accountability
- Clinical Guidelines to direct the use of telehealth as a clinical tool
- Video Visit Training to improve providers confidence with this new modality
- Pre-Visit TechChecks to ensure that patients are well connected
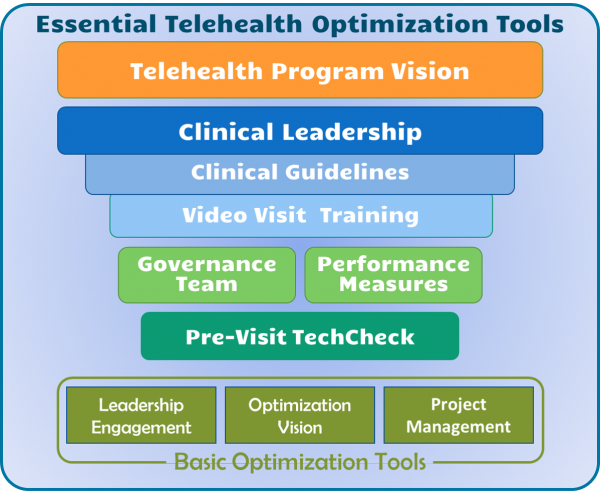
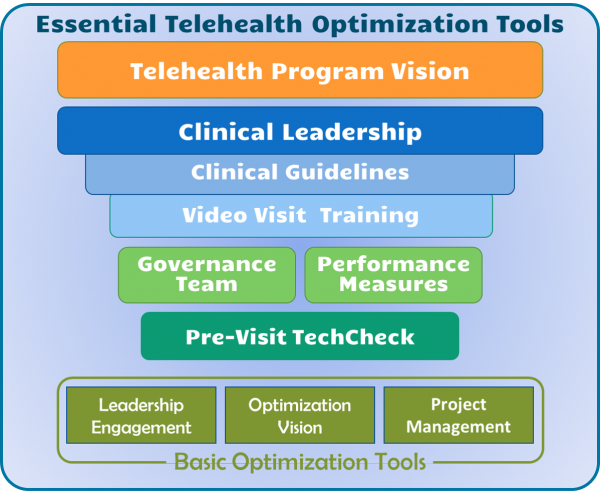
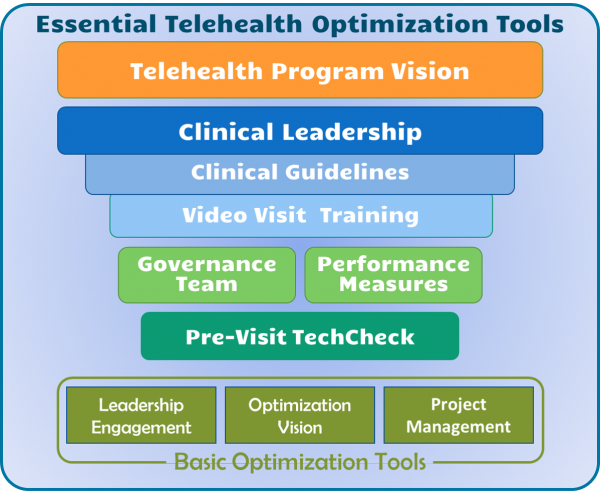
Telehealth Vision: Similar to the optimization vision, a telehealth vision paints a picture of the future that the organization wants to achieve. The best telehealth visions are closely aligned with and supportive of the organization’s overall strategic objective and they inspire the team to work hard on optimizing the individual services, so that the vision can be achieved.
Clinical Leadership: Whereas Optimization in general requires executive support, Telehealth, as a clinical tool, requires the strong leadership of a respected, effective clinician. Many organizations regard telehealth as a technical or operational workflow challenge when in reality it is a revolutionary way to deliver care that virtually no provider had ever encountered before the Covid-19 health crisis.
Telehealth Performance Measurement System: As another saying goes, “You can’t manage what you can’t measure.”, so especially in an optimization effort metrics are key. Typically these days a common set of key success metrics includes the satisfaction of clinicians and patients, technical issues, volume by modality, and financial performance.
Telehealth Governance Team: The primary role of such a steering team comprised of representatives from a variety of departments impacted by telehealth is to provide accountability and leadership. It is this team that establishes the goals for the performance metrics and holds the various teams accountable. When accountability is provided, the pace and quality of optimization is the highest.
Clinical Guidelines: Most specialties or subspecialties got thrown into telehealth in merely no time. Typically changes in the care protocols, best practices, and proven approaches take at least one decade to manifest themselves across many practices. Telehealth threw us into a complete new world and now clinicians are trying to align patients’ expectations with their own expectations as to the quality of care delivery and what is technically possible. While the official clinical telehealth guidelines are being developed, optimization can reach maximum levels when there is consensus among the clinicians when and how to wield telehealth as the right clinical tool.
Video Visit Training: Similar to breaking new ground on clinical guidelines, most clinicians were never appropriately trained on how to master the use of the audio/video technology. Clinicians in their exam room are in their comfort zone, because that’s where they trained, where they “grew up”. The virtual environment takes that comfort away and leaves many a provider uneasy. A quick 20-30 min one-on-one training on the salient points of “webside manners” often restores that confidence which will also boost the care experience for both patient and provider.
Pre-Visit TechChecks: Last but not least, even though telehealth is not about the technology, when it does not work, it is all about the technology — at least on the patient end. There are a number of things that can go “wrong” on the patient end – no or insufficient connectivity, inadequate devices, lack of awareness around lighting or sound quality, etc. All of these can typically be addressed in a quick 3-10 min call the day before by a friendly, knowledgeable representative to ensure that both the patient and the physician can have a great care experience where telehealth quickly fades into the background.
Optimizing Telehealth
Telehealth as a care delivery vehicle is here to stay and more and more patients are going to be expecting or demanding it. With the healthcare landscape changing quickly fueled by new innovation brought to healthcare by new players such as AmWell and Teladoc on the telehealth side and Walmart Health and Amazon.care on the self-insured employers side, all healthcare providers must offer telehealth in a satisfactory way. Because for patients to switch healthcare providers is as simple as a mouse click.








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.








Leave A Comment