Given the technical advances over the past 15 years, the modern healthcare consumer’s increasing demand for convenience, and the growing non-traditional competitive pressures, it is quite conceivable that within 5 years over 50% of all outpatient visits (primary care, behavioral health, and specialty care) will be conducted virtually – i.e, not in-person. This may include live video or just audio. Or it could be asynchronous secure messaging. Or even (in low percentages) a virtual reality space.
And my listing of “technical advances” does not just refer to the advances that make virtual visits a possibility. It also includes the technical innovation in diagnostics, that require physicians confirm their diagnosis or guide their treatment not solely based on their intuition or even a physical exam. No, most protocols now dictate that we need radiological tests or biomarkers. Which means that the interaction between a clinician and a patient is mostly focused on the conversation. Which can easily be done virtually.
The way I see it, the 50% mark is a given. What is not decided yet is whether it will be the Walgreens, CVSs, Teladocs, and Amwells (and literally dozens of well-funded direct primary care and virtual first care startups) or the “traditional” outpatient practices that will be offering patients this convenient form of access.
Once healthcare leaders understand, accept, and then embrace this premise, the next question becomes: how do I prepare my providers, nurses, and staff to embrace virtual visits more? And how would I know that we are making progress?
In short: What are the critical metrics to measure telehealth success?
Focus on Measuring Telehealth Success
At the current time, most healthcare leaders are completely in the dark as to the current telehealth utilization, let alone the providers’ and patients’ satisfaction with telehealth. Most assume that behavioral health is still using telehealth quite a lot and that primary care is using telehealth, but to a lesser extent.
So what is the critical set of metrics to measure the performance of a telehealth service?
The key metrics look at telehealth’s performance from three different lenses: service performance, technical performance, and financial performance.
Service performance examines the acceptance of the service by patients as well as by the clinicians. With a great service experience on both sides, telehealth is not sustainable.
Technical performance ensures that the technology (which includes connectivity) can support a seamless, painless experience, where the technology just fades into the background.
Financial performance ensures virtual care’s contribution to the bottom line of the organization.
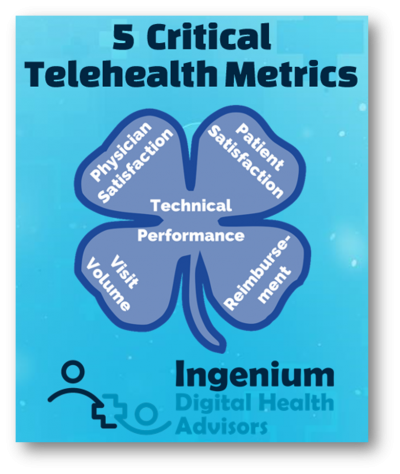
The 5 Critical Telehealth Metrics
Here are the 5 critical telehealth metrics that healthcare leaders need to pay attention to in order to ensure that their telehealth services are performing as well as they should:
Service Performance
1. Clinician Satisfaction
2. Patient Satisfaction
Technical Performance
3. Technical Performance
Financial Performance
4. Overall Visit Volume by Modality
5. Overall Reimbursement by Modality
Let’s review the nuances of these 5 critical telehealth metrics.
Service Performance Metrics
The most critical metric of all (and the one most clinics ignore) is the satisfaction of the clinicians. When we work with clients we ask the clinicians, for example, “the telehealth visit was as good as an in-person visit” and we repeatedly get 4.3 or 4.4 on a 5-point Likert scale, so high satisfaction across the board is possible.
The second metric under service performance is patient satisfaction. Typically, the acceptance of telehealth across all demographics is very high. Patients love the convenience and appreciate the efficacy with which care can be received. With our clients, we typically ask the patients “How likely are you to recommend telehealth with this provider to your friends and family?” and have gotten Net Promoter Scores (NPS) in the 70s, which is considered world-class service.
Here’s the reality: If the physicians do not like delivering care via telehealth, none of the other metrics matter much. The most prevalent root cause of statements such as “patients don’t like telehealth” is that physicians don’t like it. Even with the slickest technology and full reimbursement, if the physicians’ mindset is that telehealth is not as good as in-person care, they will find self-fulling evidence to support their sentiment.
It is therefore imperative that healthcare leaders frequently measure physician satisfaction – and then act on the data to improve satisfaction.
A powerful question we’ve started using in recent months is: “How comfortable are you offering telehealth to a patient when clinically appropriate?” While that question does not measure satisfaction directly, it gets at what we actually want: for clinicians to use telehealth when it is clinically appropriate and acceptable to the patient.
Technical Performance
While telehealth is not about the technology (but about the workflows and managing the organizational change), it certainly is about the technology when the technology is not working.
With regards to telehealth technology, there are a few “givens” that we assume: that the technology is reasonably usable, that it is secure and also reliable (assuming good internet connectivity).
The metrics to capture under “technical performance” should simply be on whether the clinician and patient could easily connect and that there are no audio/visual problems.
Any deviation from those goals is mostly the cause of individual circumstances on the clinician’s or patient’s side. Most user experience problems (on either side) can easily be compensated by workflow or process interventions, such as Pre-Visit TechChecks, and by training and coaching, e.g., on “webside manners”.
Financial Performance
Of the 5 critical metrics, the first 3 can be measured intermittently, whereas the financial metrics should be measured continuously.
The “overall visit volume by modality” metric is critical in providing a good overall picture of the performance of your healthcare organization. It should include attributes such as date, time, provider, visit type, show/no show, and modality (one of: inpatient, outpatient, video visit, telephonic visit).
Semi-automated analysis of this metric can reveal a multitude of insights: comparison to prior year volumes, distribution (and shift across all modalities), adoption by individual providers or provider groups), change in no-show rates, etc.
The “overall reimbursement by modality” metric provides critical insight into the financial performance of the organization. It should include similar attributes, including date, time, provider, modality, CPT code, payor/health plan, and actual reimbursement.
Here, semi-automated analysis of this metric can reveal an additional set of insights: e.g., comparison to prior year revenue, “the cost of telephonic vs. video telehealth”, average reimbursement per visit, usage by CPT code and modality, etc.
Using the Metrics to Drive Improvement
As I’ve stated in a prior article, “Action is the Ultimate Value of Measuring Performance”.
To implement “paying attention to”, all 5 metrics should be reported on a regular basis (weekly first, monthly later) in the form of a telehealth performance dashboard. Each metric must have a target goal along with a predefined action list in case the metric falls short of the goal, meets the goal, or exceeds the goal.
Driving in the dark without any feedback about direction, speed or the fill-level of the gas tank can be a very dangerous undertaking, especially if you are going 80 miles an hour. It is thus crucial for healthcare leaders to invest in establishing a telehealth performance dashboard that at a minimum includes these 5 critical telehealth metrics:
- Clinician Satisfaction
- Patient Satisfaction
- Technical Performance
- Overall Visit Volume by Modality
- Overall Reimbursement by Modality
Which telehealth metrics are your healthcare leaders evaluating on a regular basis? What predefined actions have you identified to overcome the challenges you are encountering?








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.








