A bridge is typically a metaphor for creating a shortcut, crossing a chasm, or to overcome an obstacle like a river. A Telehealth Strategy serves the same purpose: to navigate you confidently across and through the uncertain future to get “to the other side”.
Unlike bridges though, plans and strategies are not created to last forever. They are temporary structures, intended to get you from where you are today to where you want to go.
As Dwight D. Eisenhower observed:
“In preparing for battle I have always found
that plans are useless, but planning is indispensable.”
Strategies and the accompanying business plans exist for the same reason: to provide indispensable insights into the various facets of what it will take to arrive at a better future.
The Case for a Telehealth Strategy
The Covid-19 crisis thrust many healthcare providers into telehealth overnight, oftentimes launching the new offering quite haphazardly. While many larger and mid-sized organizations had already launched a number of telehealth services, the unprecedented need to safely connect clinicians with patients resulted in an unprecedented demand for telehealth. This left no time for planning or coordination.
Now, six months into the health crisis, the best healthcare leaders are realizing the need for a well-defined and well-executed telehealth strategy. In order to make the most out of telehealth and to stay competitive in this new normal where over 90% of patients have had a great experience with telehealth, healthcare organizations must embrace telehealth across all clinical areas and become proficient at it.
The Imperative for a Telehealth Strategy
Now more than ever, healthcare organizations are in increasing financial distress and its leaders must ensure that they are focusing their limited resources on the most valuable opportunities. The fallout of a lack of a strategy can be crippling.
In a best-case scenario, individual clinicians or smaller departments will go out and use whatever telehealth solution they can find with whatever telehealth service workflow they think is best. With a wild growth of a plethora of technology, this creates a disconnected patient experience and increases IT support cost. Without the comprehensive expert input, this rogue effort also opens the organization up for legal exposures and may leave significant amounts of money on the table when it comes to reimbursement.
In a worst-case scenario, the lack of virtual care modalities will drive the modern healthcare consumer to simply take their care needs to a different virtual provider. Whether that is a “virtual-only” service like the ones offered by Teladoc or AmWell, or whether that is the virtual offerings of a regional provider that is putting appropriate emphasis on a telehealth strategy.
The Scope of Telehealth
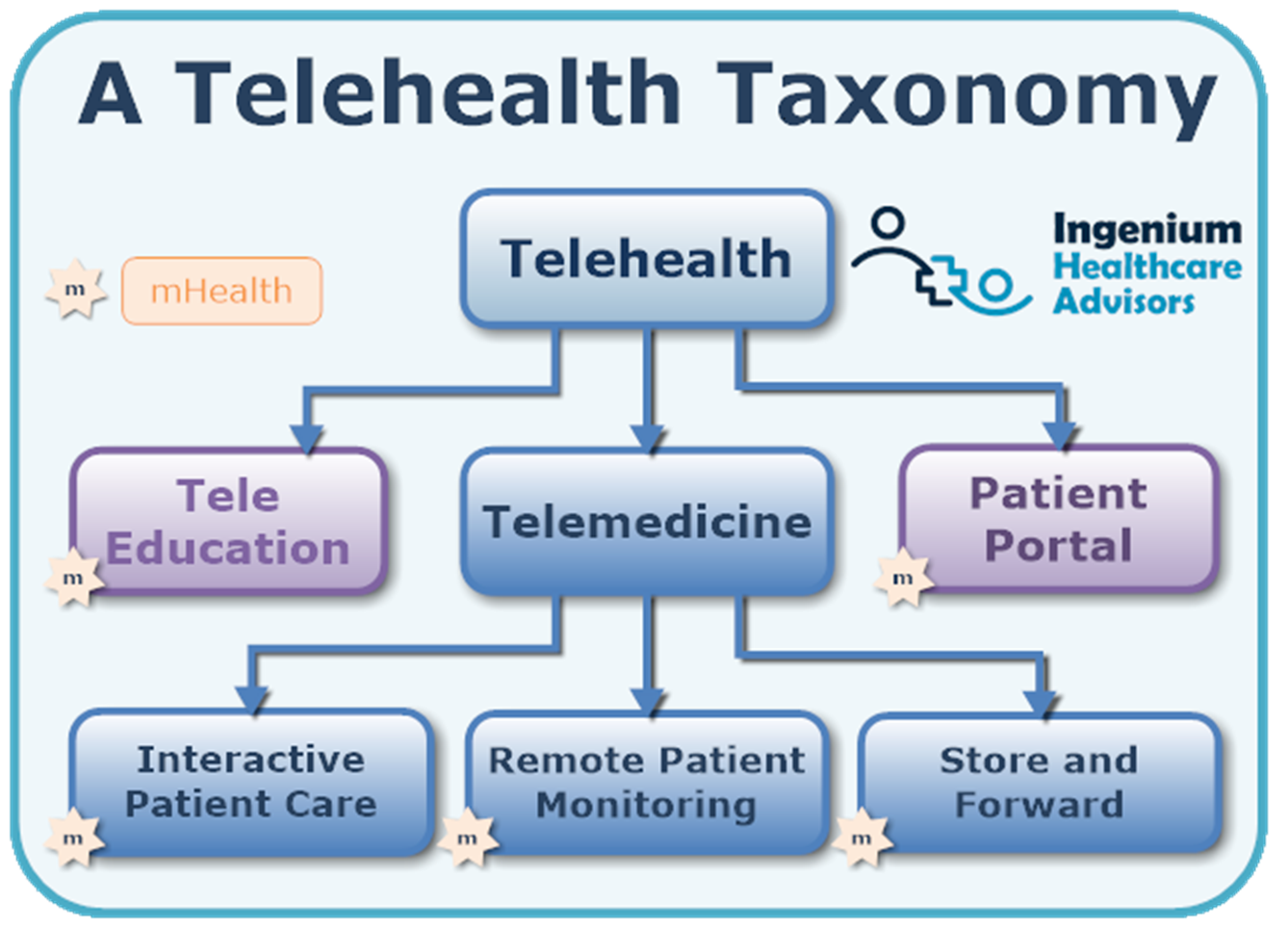
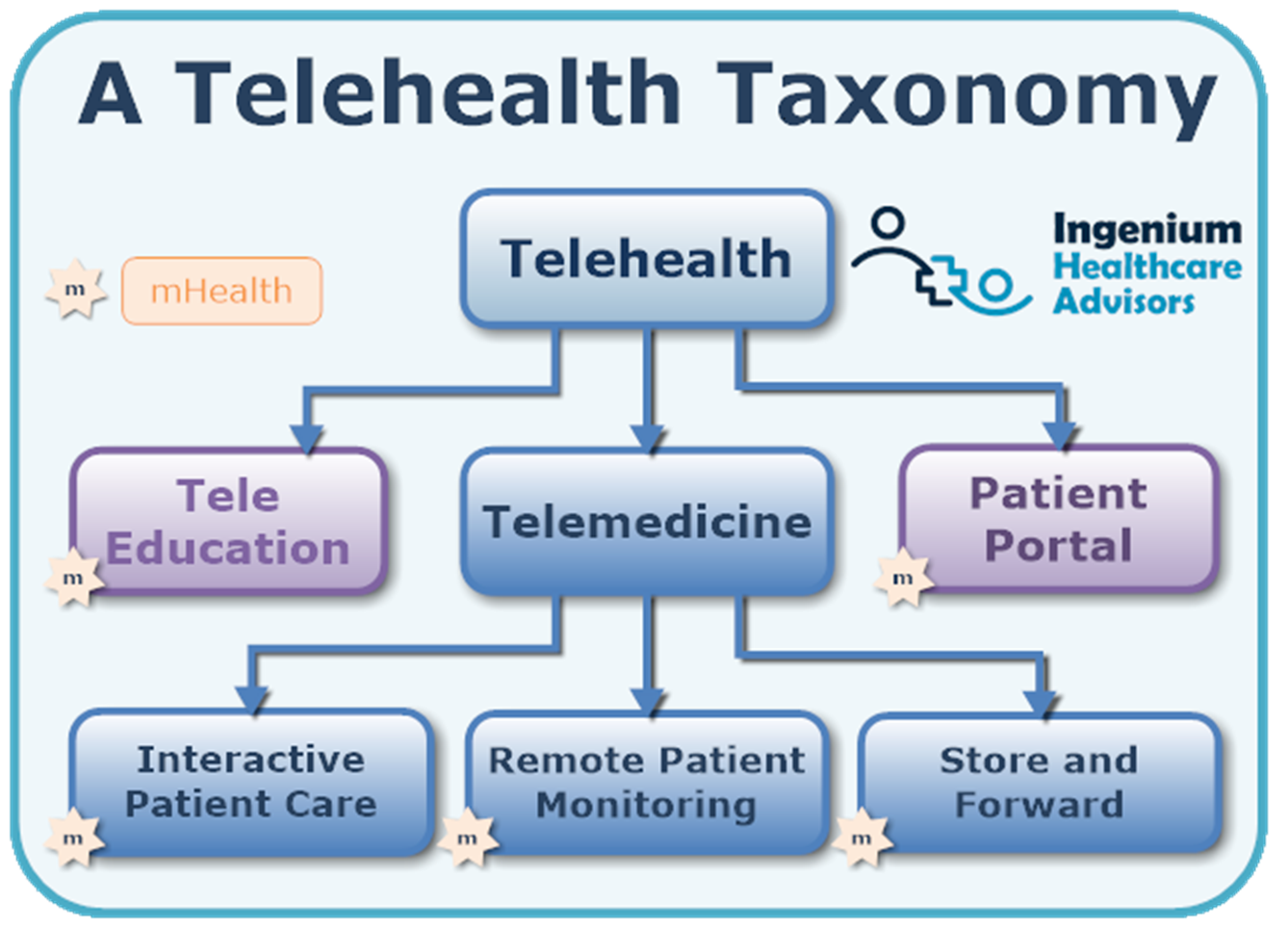
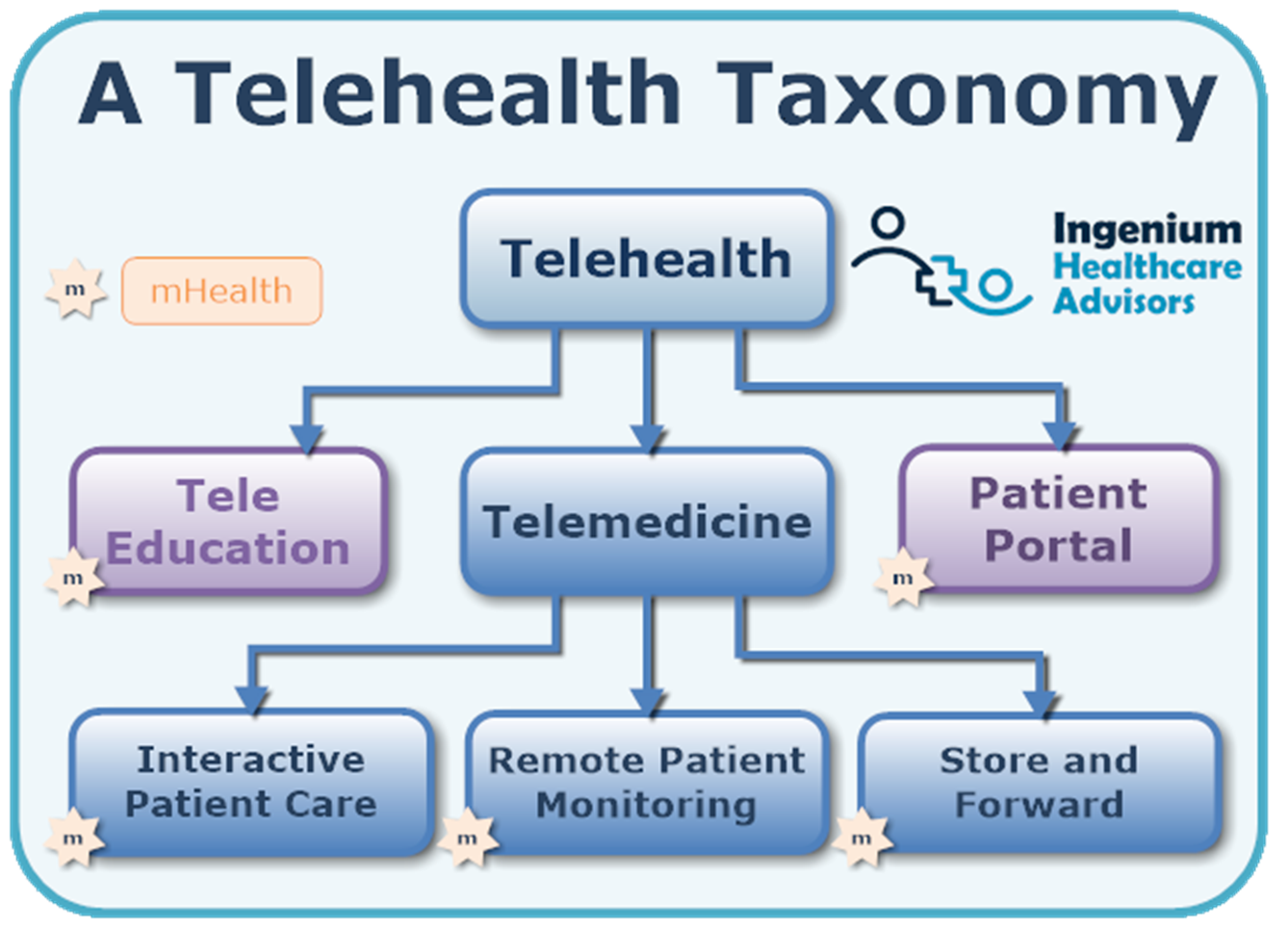
Telehealth is delivering care at a distance.
This includes any interactions of the modern healthcare consumer with the healthcare organization – from scheduling appointments to downloading immunization records; from post-surgical just-in-time education to obtaining a refill.
Telemedicine, which we define as practicing medicine at a distance, is a subset of Telehealth and includes any synchronous or asynchronous interactions between patients and clinicians – either via video or telephonic visits, remote physiological monitoring (RPM), or through the store & forward mechanism, such as sending images of rashes, etc.
With such a broad and encompassing definition, it is not surprising that there are over 10,000 potential use cases for telehealth using Interactive Patient Care alone. Without a strategy, it can be overwhelming to decide which telemedicine services to launch first.
Driving Lasting & Successful Change with a Telehealth Strategy
The Covid-19 health crisis has made it rapidly clear to even the most conservative leaders, that it is impossible to imagine a future of healthcare without the delivery of care at a distance.
But healthcare is conservative and only changes slowly. And despite the many Covid-related waivers, financial and cultural(!) telehealth sustainability are far from being a “given”. In my experience only a comprehensive plan, a telehealth strategy, will help you succeed in getting telehealth established and making it last.
A Telehealth Strategy systematically helps to guide your organization’s efforts and is the difference between failure and success.
In the early 2010s in one rural health system, the senior leadership team spent a few months upfront to develop a strategic plan and went from 0 to 700 annual televisits in 13 locations and across eight different medical specialties in under two years. Yet another, very large and renowned healthcare organization without an overarching plan continued to spend resources all over the place with many initiatives fizzling out after just a few years. And a mid-sized integration health system in the same region took over 15 years to bring its numbers up to 1,000 visits a year.
The difference between those three examples? Investing in a strategy developed by the senior leadership team.
A Telehealth Strategy’s Core Elements



Next, the telehealth strategy must demonstrate how telehealth will be used to drive the organization’s strategic objectives – again, to drive the buy-in by everyone in the organization.
Given the financial situation for most healthcare organizations, the next logical step is to ensure that the telehealth program overall has a financial case that creates a positive overall ROI across the program of all telehealth services – from direct revenues as well as indirect revenues, taking a systems point of view .
Embedded in the first three elements of the Telehealth Strategy is also the assessment of the demand as well as the competition, creating another compelling argument for the “why” of telehealth.
One of the most important aspects of a telehealth strategy is to define and apply the process by which current and future telehealth use cases can be evaluated and prioritized. With hundreds of potential use cases each mature organization must develop its own rubrik to quickly assess a proposed telehealth service’s fit with the organization’s overall telehealth strategy.
Far less important, but nonetheless essential is the definition of the principles behind the decision making process on new telehealth technology solutions and strategies to reign in and consolidate any wild growth of unofficial technologies.
The embracing of telehealth as a care delivery mechanism is first and foremost a change management effort and only secondarily a “customer education” effort. Internal resistance, frustration, confusion and sometimes outright hostility is by far the key reason behind the failure of most telehealth programs. As such, a telehealth strategy must outline the strategies and principles behind engaging the clinicians and staff.
Last, but not least, the telehealth strategy, like any good business plan, must lay out the staffing model to support the launch of new services; support the ongoing operations; and guiding the organization through leadership.
Driving Buy-in Through a Telehealth Strategy
The primary value of a telehealth strategy lies in increased buy-in resulting in a much smoother implementation and fewer false starts. This also results in fewer wasted resources, such as the investment in the wrong technology, or the failure to establish a service because a key champion leaves the organization.
Without a telehealth strategy, the implementation of a telehealth service has numerous opportunities to encounter resistance from many sides: IT, finance, billing, nursing, providers, and even patients. Without a plan, implementations can drag on forever, especially if the opportunity of a good “first impression” is missed.
In my experience, a well thought out plan however, engages key opinion leaders and is the key reason for immediate and lasting, sustainable success; especially if the long-term goal is to incorporate elements of telehealth and telemedicine across the organization.
Telehealth Tuesday Trigger
Does your organization have a Telehealth Strategy? Has it been updated since the beginning of the Covid-19 health crisis? Which elements does your strategy not cover? What elements does it contain that I did not address here?
For a complimentary consultation on how to create or improve on your organization’s telehealth strategy, contact Christian per the options below.








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.









Leave A Comment