About 2 Million babies were born in the US from the beginning of the Covid-19 health crisis and the end of September 2020. Based on pre-Covid statistics at least 200,000 of them were born prematurely. There is a growing concern that due to the increased social distancing and expecting moms’ concern about getting infected with the coronavirus, that many more moms had an unnecessarily more risky pregnancy. Can telehealth help provide better prenatal care?
The many facets of telehealth
These days most people think first about video visits when they hear the term telehealth or telemedicine. We use telehealth to refer to all services that “deliver care at a distance” which includes patient visits, but also remote education (e.g., pre-surgical or post-diagnostic education) and patient portal interactions, such as ordering refills, reviewing physician notes, or downloading immunization).
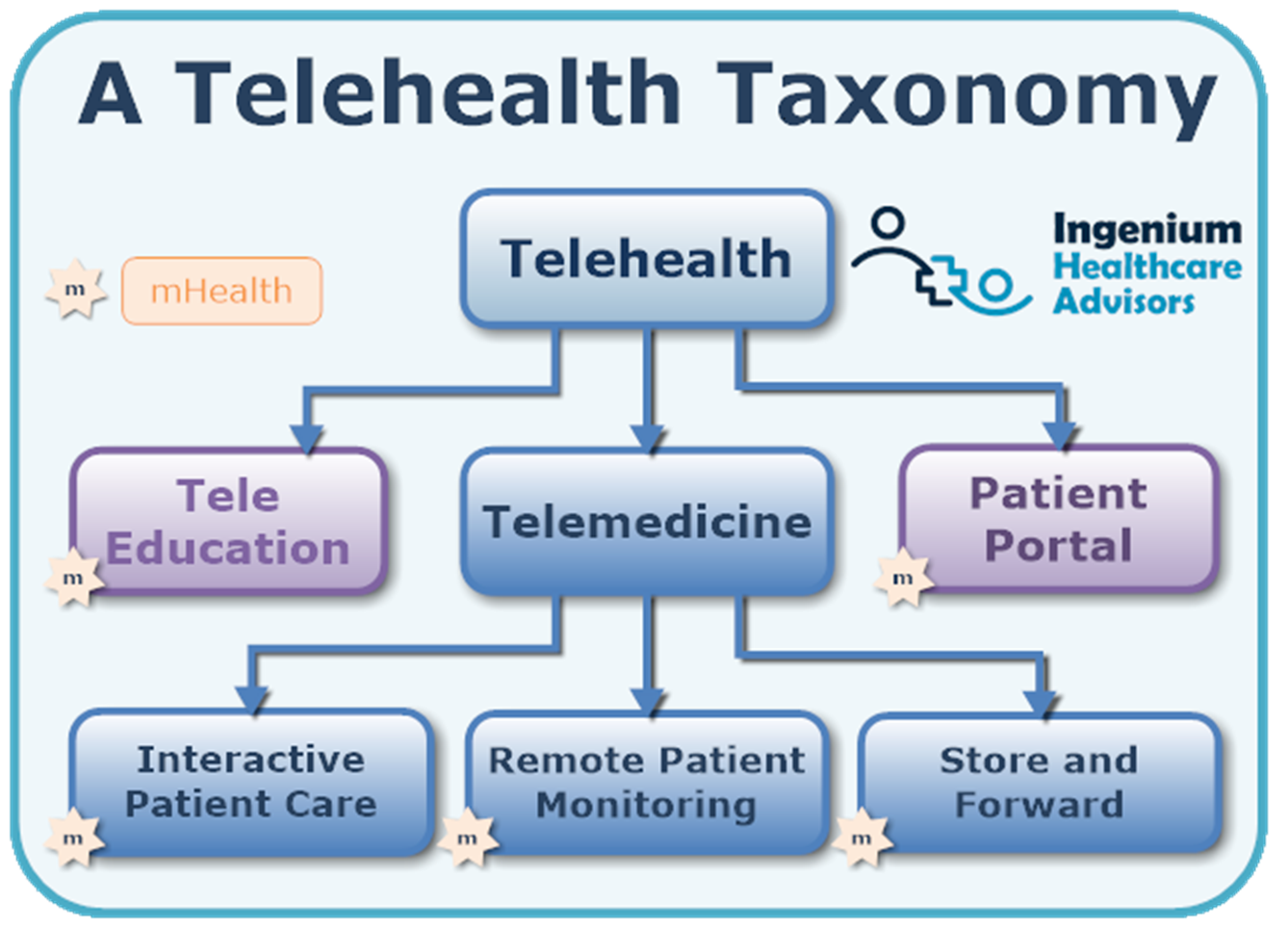
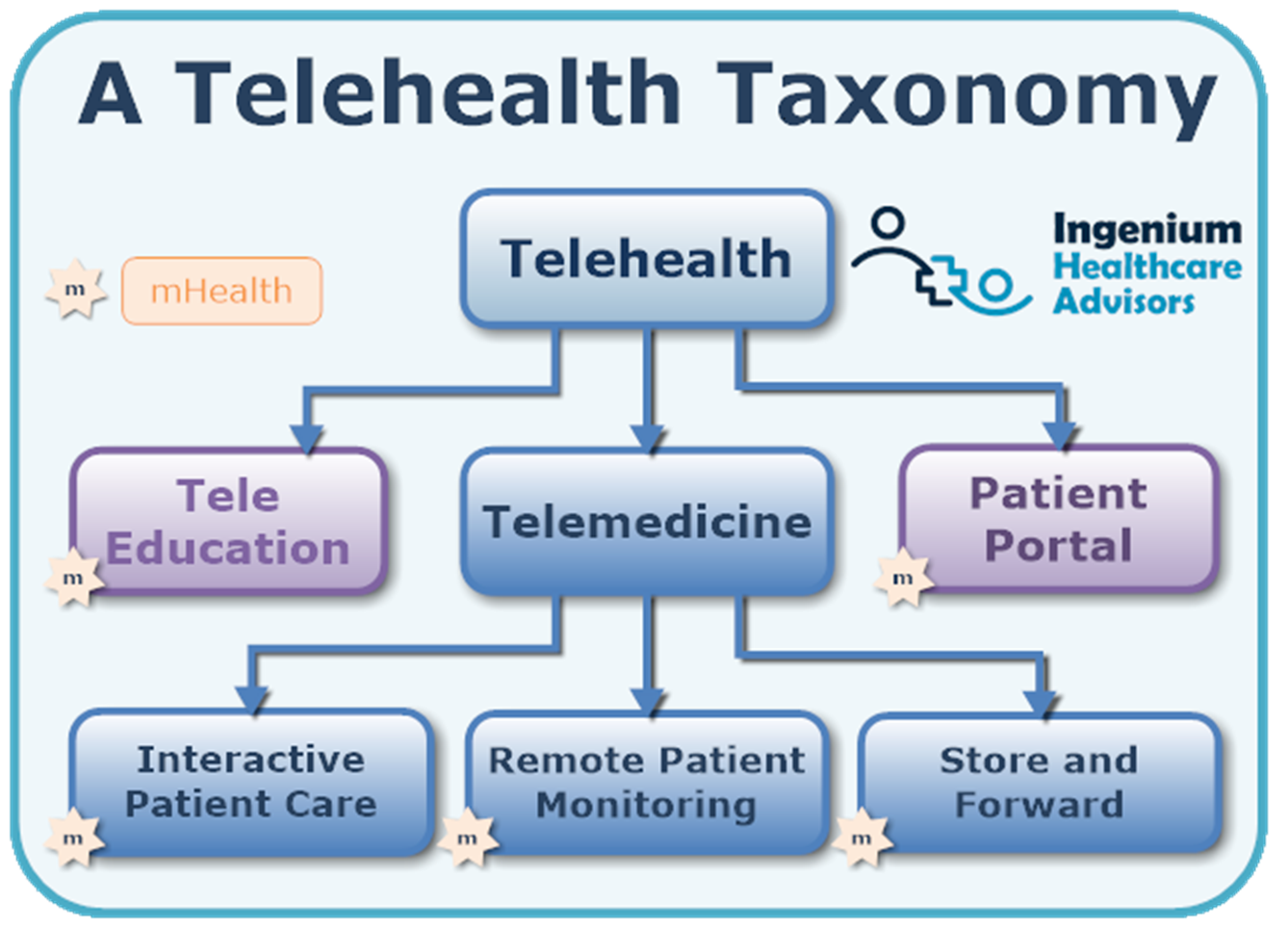
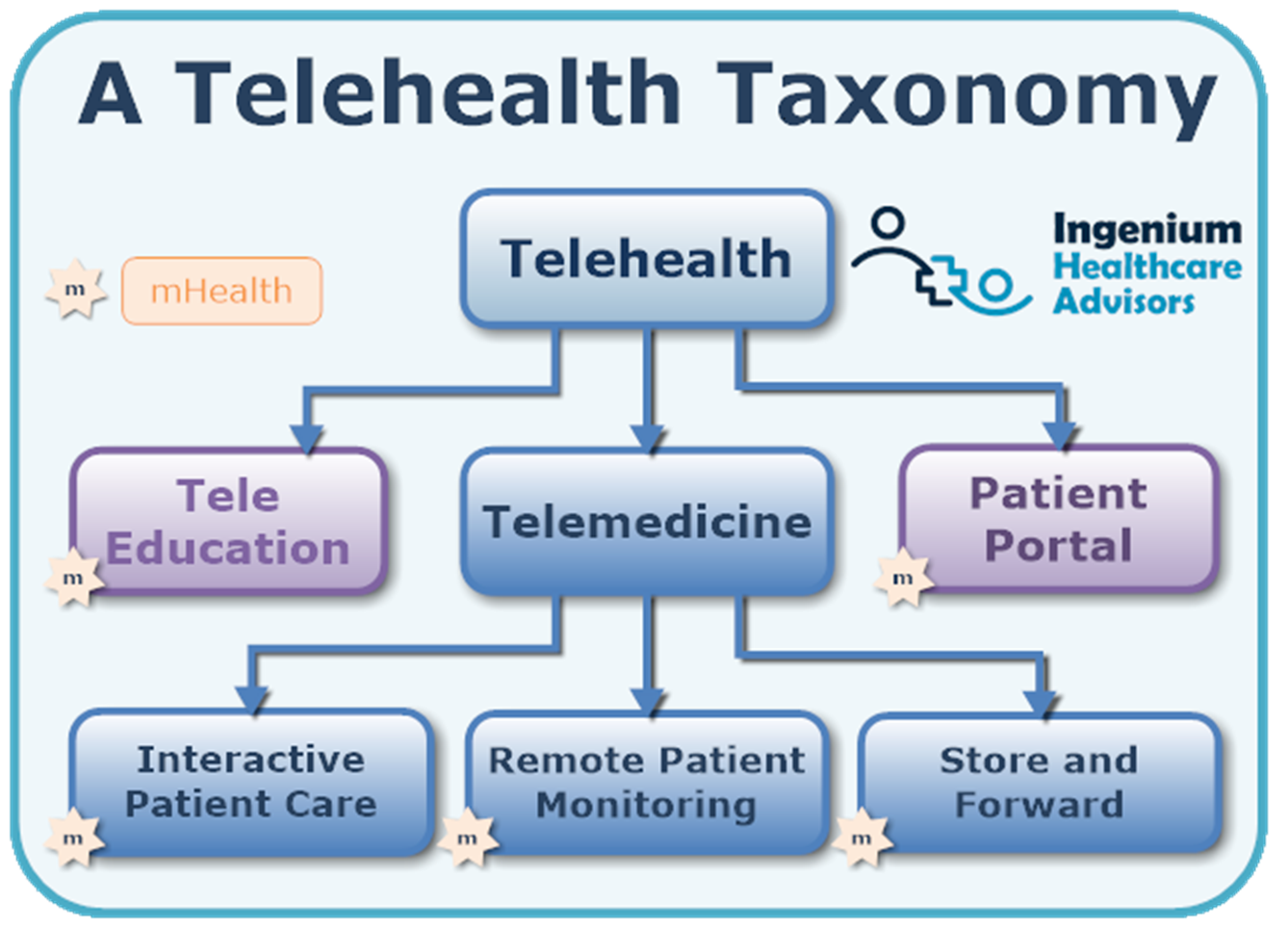
Within the domain of telemedicine, interactive patient care — including video or telephonic visits — is the service that most people associated with telehealth. But as the graphic shows, telemedicine also includes RPM and store and forward services.
RPM can stand for remote patient monitoring or remote physiological monitoring and is concerned with the long-term periodic or continuous collection and display of key patient vital signs, such as weight, temperature, blood pressure, heart rate or blood glucose levels.
Store-and-forward services include the faxing of an EKG or taking and sending a photo of a tick bite or skin rash to a primary care physician or dermatologist for review and evaluation.
All three subsets of telehealth — live audio/video visits, remote physiological monitoring, and store and forward — add tremendous value to the virtual/remote care of expecting moms:
- Using live audio/visits for prenatal checkups, for depression screening, for pre-labor preparation etc.
- Using RPM to periodically monitor weight, blood pressure, heart rate and, for moms with diabetes or gestational diabetes, the automatic transmission of blood sugar levels.
- Using pictures or videos to convey more detailed information about an ailment
Achieving better prenatal care through telehealth
There are a number of different conditions under which remote access to care can make a significant difference for the health of the expecting mother and the unborn child. In this article we’ll be focusing in on the following four.
- Rural/Shortage: Regular access to prenatal care for expecting moms living in rural areas and/or far away from their nearest OB/Gyn provider.
- High-risk pregnancies: Pregnancies considered high risk due to the health condition of the mother (e.g., multiple chronic diseases, etc.) or other factors.
- Covid-19 infected: Access to care for moms infected with the virus, but only showing mild symptoms.
- Coronaphobic/Precaution: Expecting moms concerned about a Covid-19 infection and/or high anxiety levels or underlying mental health conditions making normal, in-person care difficult or even unfeasible.
Rural/Shortage
As with quite a few medical specialties, there is a general shortage of OB/Gyn providers, especially in rural areas that may not be as attractive for young physicians to set up a practice. For these moms, telehealth provides the opportunity to easily stay in touch with their OB/Gyn provider.
Even before Covid-19, leading healthcare providers, such as the Mayo Clinic, implemented remote access programs during pregnancy, only requiring moms to come into the practice 3-4 times during the pregnancy. The health crisis has now accelerated the adoption of such a program.
The key benefits of this approach lie in the continuity of care and the virtual absence of now shows. Oftentimes the logistical challenges of getting to the OBGyn in time seem insurmountable.
High-Risk Pregnancies
When the health of the expecting mom is compromised or not well managed, the mom’s underlying health conditions can pose a severe risk to the unborn child. A combination of remote monitoring of the mom’s health as well as regular video visits can ensure that mom’s health is well managed to allow for an uneventful pregnancy and delivery.
Especially during the last trimester, additional digital health tools can be brought to bear, such as a fetal heart rate or a contraction monitor, providing additional valuable insights into the unborn’s health.
Covid-19 infected
Obviously nobody wants to inadvertently infect others, especially not healthcare workers, and therefore virtual access to care can be, just like in other clinical specialties, a great tool to keep potentially or actually infected moms at home.
Coronaphobia/Precaution: For some expecting moms the motivation to stay home and not go to a clinic may stem from precautionary measures, such as an immunocompromised family member. Or it may be driven by a general state of anxiety or concern about their health or the health of their unborn child.
Measurable Parameters
The combination of virtual video visits and electronic transmission of key vital signs allows for pretty decent care management of expecting moms who, for a variety of reasons want to or need to stay home.
As indicated above, a “virtual prenatal care” solution can be used to collect and track a number of parameters. Here are a few of the most common ones being collected.
- Weight: tracking the mom’s weight over time – oftentimes with a bluetooth scale that automatically captures the weight – can be helpful in assessing the healthy progress of the pregnancy.
- Blood Pressure: track the mom’s blood pressure over time, as some expecting moms are at risk for gestational hypertension or preeclampsia or need their blood pressure managed in general.
- Temperature: obviously during this Covid-19 health crisis accurate body temperature data can be very helpful to effectively manage any infection or illnesses, especially any conditions that could harm the unborn child.
- Bloodsugar: Especially for diabetics or moms developing gestational diabetes accurately and periodically measuring glucose is valuable in keeping the expecting mom’s blood sugar within acceptable ranges.
- Mental Health/Mood: many RPM solutions also include the ability to periodically have the patient complete a questionnaire. For expecting moms that could include proactive screening for postpartum depression or other mental health states that could have a bearing on the outcome of the pregnancy.
The future of Prenatal Care
Both Virtual Video Visits and Remote Physiological Monitoring have been around for decades but traditionally have not found much application in women’s health in general and OB/Gyn care in particular. The positive experience gained from using this technology during the Covid-19 health crisis can hopefully open the door to a more frequent use of these technologies to improve prenatal and postpartum care.
For now, Covid-19 has unfortunately exacerbated the absence of clinically valuable remote care solutions in prenatal care, with some care protocols being limited to the occasional phone call with very little exam capabilities or insights into the expecting moms actual health.
For the general patient population, the first wave of telehealth in response to the Coronavirus was the use of telephonic care at first, then video-based remote care visits. The next wave now is to get better access to vital signs to complete the medical picture.
We can do the same in prenatal care.
Both technologies (video visits and RPM) can and should be used for prenatal care – and with most prenatal care being paid for as a bundle, healthcare providers have a strong incentive to minimize potentially avoidable utilization, such as urgent care and emergency care visits or hospitalizations.
Thus telehealth should be used to enable better prenatal care.








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.









Leave A Comment