Many in healthcare still see telehealth primarily as a technology.
That is not surprising, since the name “telehealth” invokes a first association with other technologies that have advanced human kind in the last 50 to a 100 years: the television, the telephone, even the telescope, or in medicine, telemetry.
In addition, many organizations seem to have an ongoing battle with the technical aspects of telehealth, such as connectivity and bandwidth issues, patients’ digital illiteracy, and technical integration and interface challenges, e.g., with exam peripherals or integration with the EMR.
Given that experience, many clinicians, especially in primary care, are reluctant to fully embrace telehealth. Which is unfortunate, since the potential for telehealth to do a lot of good for the patient population is very strong.
Telehealth is a Clinical Tool
So, if telehealth is not a technology, what is it then?
First and foremost telehealth is a clinical tool. Just like other clinical tools (e.g., lab tests or imaging tests), telehealth can be consciously selected as the right tool for patient care, if clinicians are aware of their choice.
Telehealth is also a care delivery modality – just like an in-person visit, a phone call, a letter, or a secure message. It’s a different avenue to interact with patients during diagnosis, treatment, and health maintenance.
And telehealth is a great tool in the quest toward improving Population Health.
Population Health, defined
While virtually every larger healthcare organization typically has staff designated toward supporting population health, a commonly agreed on definition is hard to come by, especially when contrasting it with public health.
In simple terms, public health is concerned with creating an environment where people can be healthy, whereas population health focuses on overcoming the problems that drive poor health conditions in the population.
Public Health focuses on policies, research and injury prevention, whereas Population Health focuses on a multi-disciplinary, organization-transcending, collaborative community approach with a focus on health outcomes.
Specifically, the two most important Population Health objectives are Chronic Disease Management and Preventive Health Promotion:
- Chronic Disease Management: ensure that people with chronic diseases live longer with a higher quality of life.
- Preventive Health Promotion: promote a healthy lifestyle, including weight loss, higher activity levels, smoking and drinking cessation, meditation & mindfulness, etc.
Bring in the Telehealth Power Tools
So how can telehealth help to achieve Population Health goals?
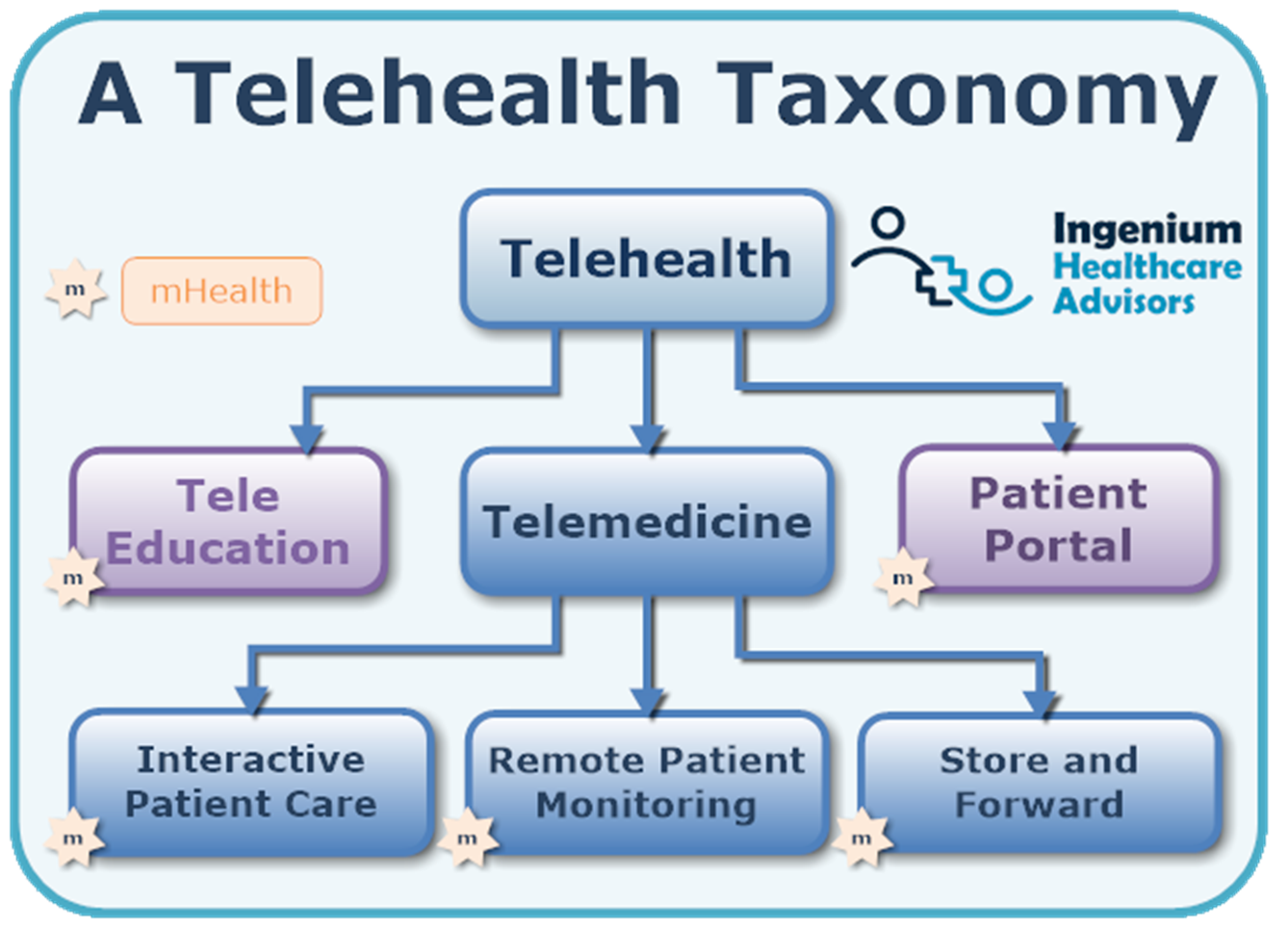
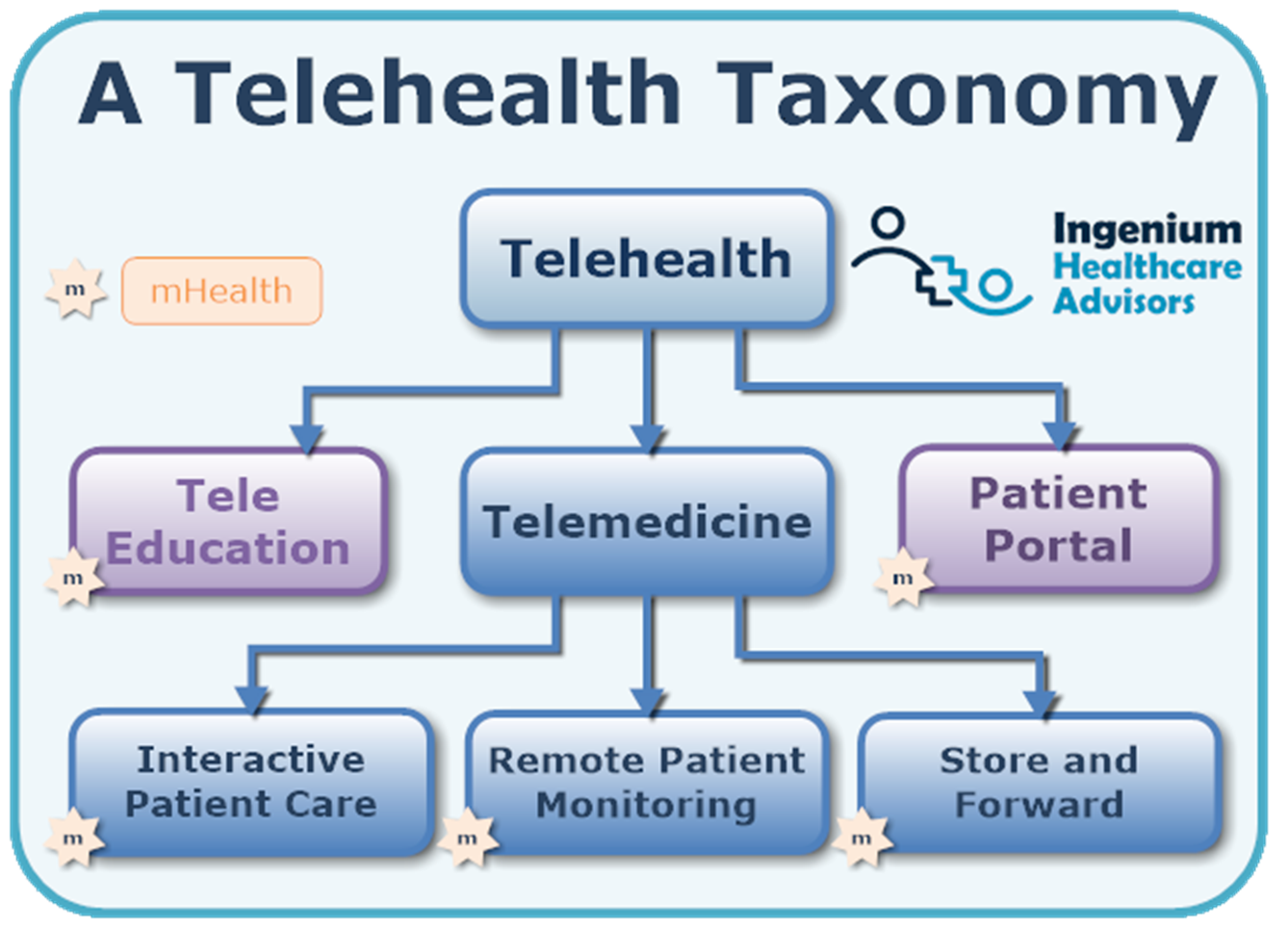
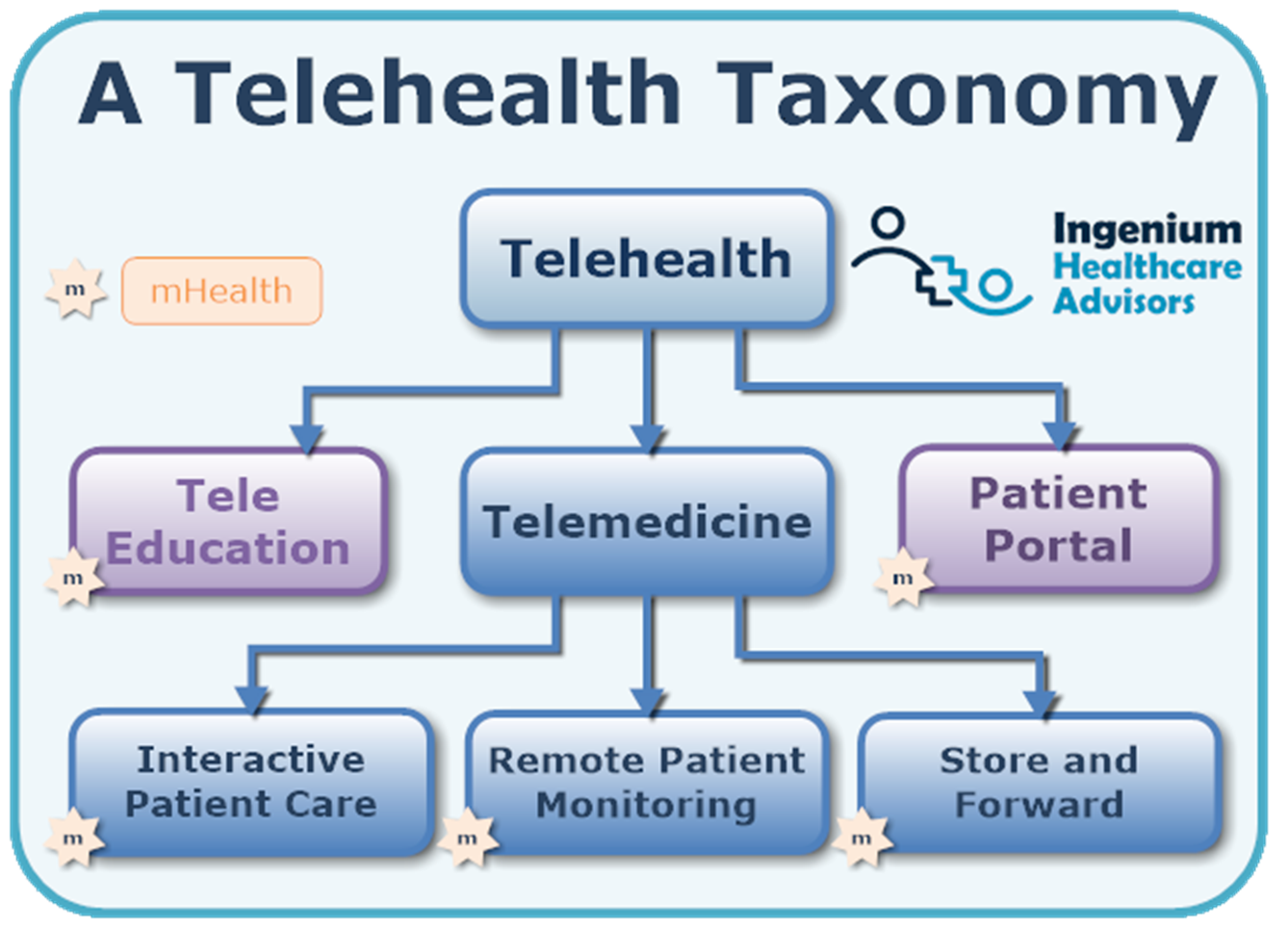
It first starts with a mindset shift about telehealth – namely that it is a clinical tool for “delivering care at a distance” that comes in a multitude of flavors:
- TeleEducation – live or on demand information to assist with self-care, lifestyle changes, presurgical education, post-diagnostic information, etc.
- Patient Portal – a virtual self-service kiosk to access various, mostly administrative, services, such as scheduling appointments, sending secure messages, requesting notes or records, etc.
- TeleVisits: live audio/video conversations between a clinician and a patient (what most people think of telehealth)
- TeleExams: a live audio/video visit with the ability to remotely examine the patient either directly or through the assistance of a telepresenter or the patient themselves.
- Telephonic Care: a lesser, but under many circumstances still clinically feasible
- Secure Messaging/Texting: asynchronous but interactive communication between clinicians and patients.
- Remote Physiological Monitoring: the periodic or continuous monitoring of vital signs, including blood pressure, weight, heart rate, blood glucose, etc.
- Store & Forward: sending pictures, video, or voice recordings for asynchronous review by a clinician
- Digital Health Apps: 15 years after the introduction of the iPhone, the adage of “there’s an app for that” is truer than ever for health apps. Most apps fall in one of three categories: educational, tracking, and therapeutic.
Using Telehealth to Advance Population Health Goals
When telehealth is understood and used this broadly (vs. reducing telehealth merely to video visits) the possibilities to augment traditional approaches to address population health are only limited by imagination.
The most critical advantage of telehealth is the ability to remove barriers to access.
Many of the patients targeted by population health measures often don’t have the time or the means to make time for their care. Depending on the circumstances, a 10-minute doctor visit can take up to 2 hours, requiring patients to take time off from work, pay for transportation or arrange for a babysitter. With telehealth, a 10-minute visit can be completed in less than 15 minutes – while never leaving home or seeking a private place at work to have a 10-minute conversation.
Similarly, the use of TeleEducation or Remote Patient Monitoring services makes it much more convenient for patients to take care of their health. At least they can do so much more regularly than without such offerings.
One of the biggest advantages of telehealth is the convenience factor. Remote education, especially one that is on demand, is much easier to take advantage of than an in-person seminar in the evening.
Getting a reminder message to step on the scale and take a blood pressure reading in a remote physiological monitoring program is much easier than having to go into the doctor’s office to capture those vital signs on a regular basis.
So here are some common applications of telehealth to achieve the two most common areas of population health:
Telehealth Use Cases for Chronic Disease Management
- Periodic Remote Physiological Monitoring of vital signs for the management of chronic conditions such as hypertension (blood pressure), heart failure (weight and blood pressure), diabetes (blood glucose), COPD (Peak Flow/FEV1), etc.
- Follow-up visits (e.g., lab result reviews) and medication adjustment via TeleVisits.
- On demand TeleEducation about diagnosis, treatment and self-care.
- Integrated, supportive behavioral health counseling via TeleVisits.
- Live TeleExams in remote environments, such as nursing homes or assisted living facilities, with the help of a TelePresenter.
- etc.
Telehealth Use Cases for Preventive Care
- Simple Remote Physiological Monitoring or Digital Health Apps for tracking, monitoring, and management of weight, activity level, or caloric intake.
- On demand or interactive TeleEducation to provide knowledge (e.g., food, cooking) or peer support.
- Supportive behavioral health counseling via TeleVisits to remove psychological barriers to lifestyle changes.
- Digital Health Apps for meditation or mindfulness guidance and tracking.
- Case Management or Social Worker TeleVisits to provide support, assist in care navigation, or provide access to resources.
- etc.
Once the paradigm of only treating patients in the four walls of a clinic has been shattered, telehealth in its many forms offers a plethora of opportunities to help an organization achieve its population health goals, typically with a much higher degree of engagement than in traditional programs that require patients to go somewhere.
And therein lies the superpower of telehealth as a power tool for Population Health.








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.








Leave A Comment