A couple weeks back I wrote about improving mental & behavioral health at a distance. In the article I highlighted the different types of telebehavioral health and the various modalities that can be used to deliver behavioral health care “at a distance”.
In today’s column, I’d like to take things a little further, and point out the various tweaks and turns you or your organization can take to “take telebehavioral health to the next level”.
Start with the End In Mind: Telebehavioral Health Performance
In order to chart a course to the next level, we first need to know what level we are striving for. What is it that we want to achieve?
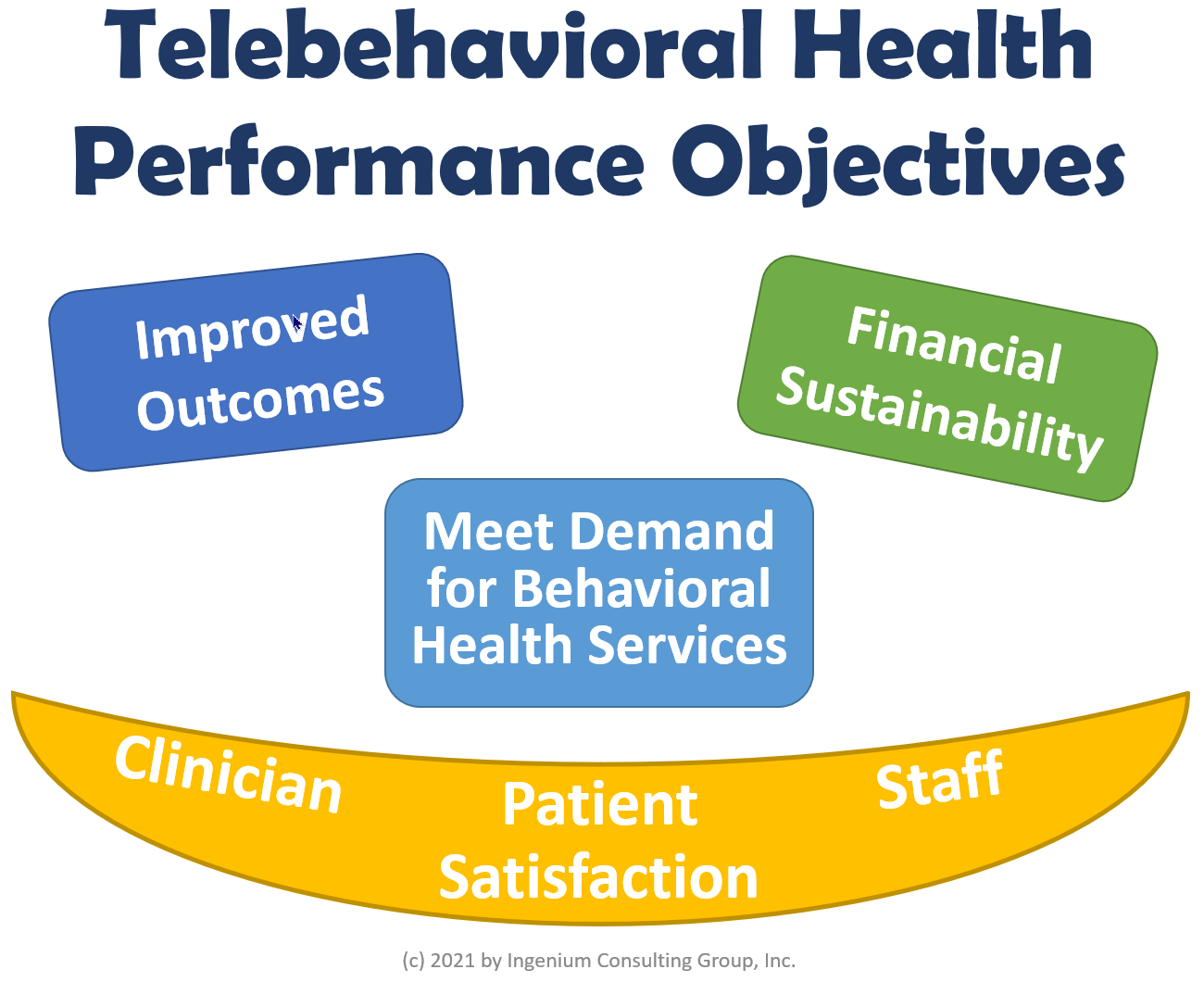
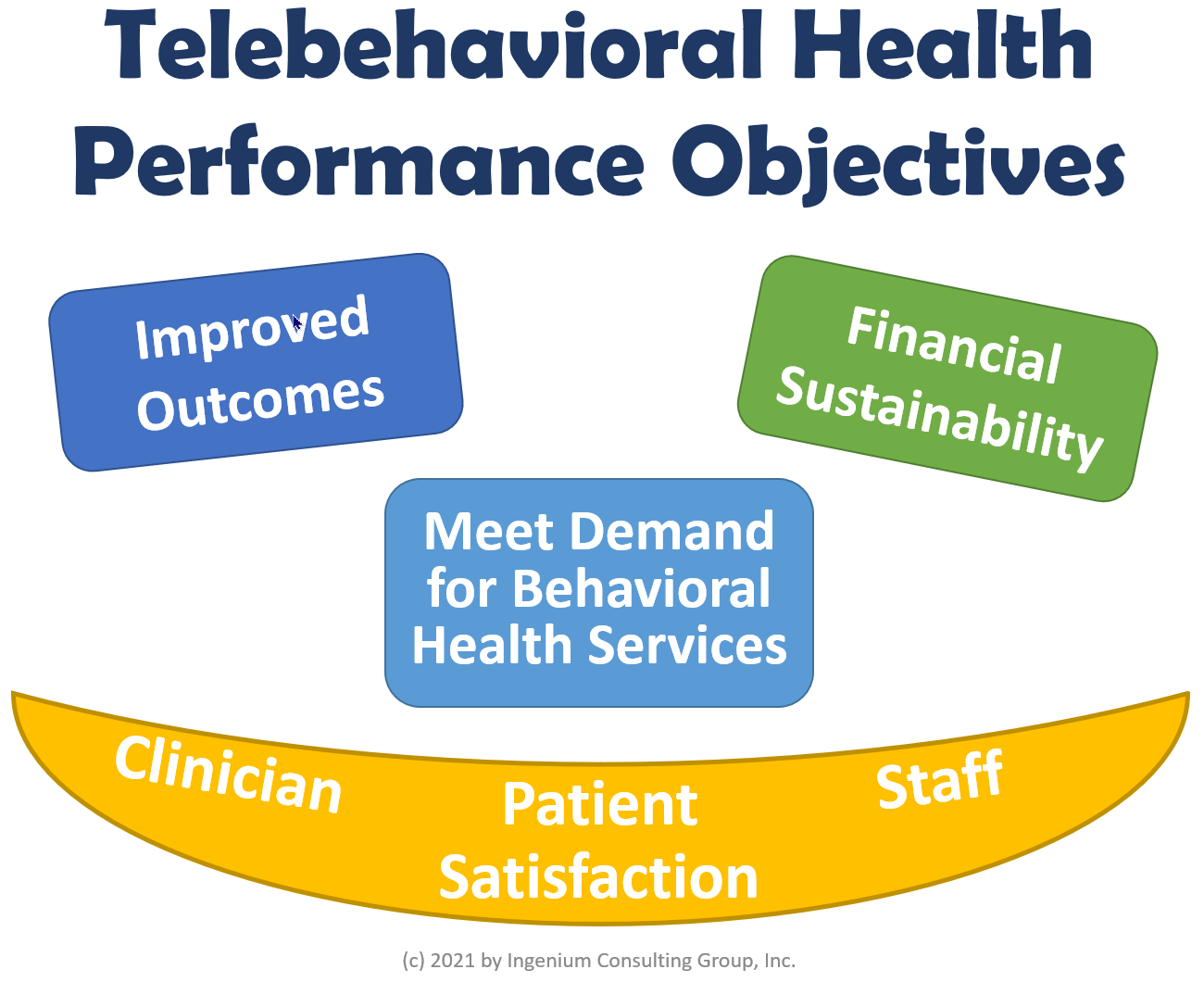
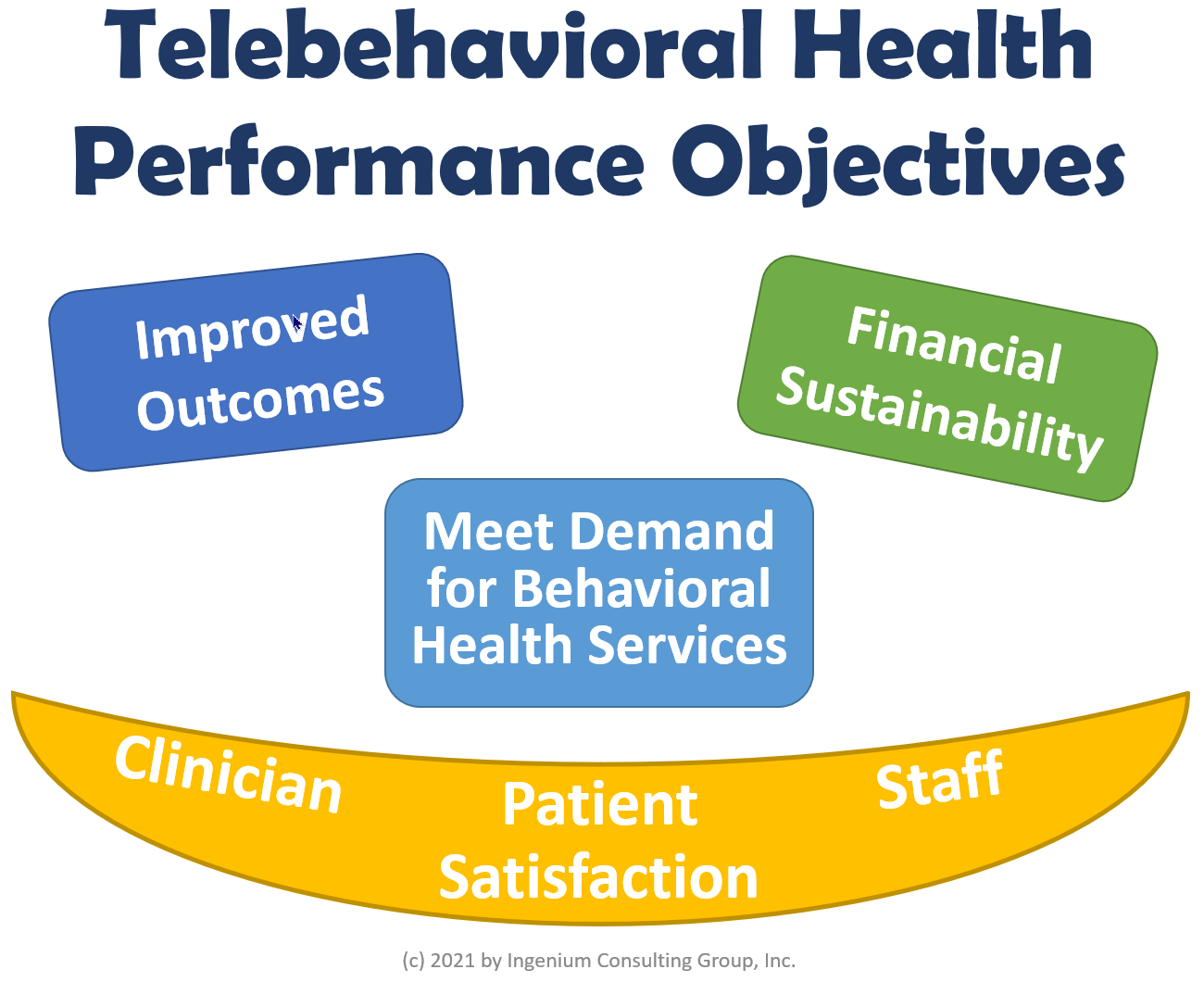
I suggest we focus on the following six aspects to assess the performance of your telebehavioral health services:
- Improved Outcomes — We’re all after the same goal, and that is to improve the patient condition.
- Financial Sustainability — the times when telehealth grants funded the clinician time are over. We need sustainable ways to deliver behavioral health care at a distance that is economically sustainable.
- High Patient Satisfaction — patient engagement and continuity of care only happens if patients/clients are satisfied with their experience.
- High Clinician Satisfaction — without clinician buy-in, we don’t have good outcomes, any high turnover directly affects the bottom line, and patient satisfaction is directly proportional to clinician satisfaction.
- High Staff Satisfaction — there are many other key stakeholders involved in ensuring a pleasant, professional experience for the patient, though it is imperative that staff are increasingly satisfied with all things telehealth as well.
- Meet the Demand for Telebehavioral Health Services — this performance goal is unique to behavioral health and challenging to accomplish, but nonetheless crucial.
The Power of Subspecialization
Before we dive deeper, I want to highlight one aspect of telebehavioral health that is often overlooked, primarily because for all intents and purposes we are very new to all of this telehealth.
I started my career in healthcare at the Mayo Clinic and after having been there for a while, finally began to understand what made the Mayo Clinic so great. It was not their brilliant marketing. It was definitely not the location (more like the city of Oz in the middle of corn fields). And though it was the people — the greeters, the receptionists, the nurses, the physicians (and even most of the surgeons) — it was the fact that at the Mayo Clinic you could find the physician who for most of their career had specialized their expertise on the condition that you were seeking treatment for.
That subspecialization is the draw for the majority of the patients who seek care at the Mayo Clinic. My favorite example is a transplant surgeon who focuses on nothing but small bowel transplants (already a niche in itself) for infants and toddlers. Given the rule of 10,000 hours, (giving your expert status), this surgeon became incredibly proficient and excellent in this niche of transplantation surgery.
Needless to say, if your child needs such a procedure, you’d fly into the middle of the corn field (even in the middle of winter) immediately. You don’t someone who knows how to do it. You want someone who has done it hundreds of times.
The same opportunities of subspecialization are now arising across all specialties for many clinicians, but especially in behavioral health. Given the much larger geographic reach and the wide-spread need, telehealth now affords clinicians to build a practice around their particular area of interest, virtually with no limits to how narrow the scope could be.
This mindset shift alone can take your telebehavioral health program to the next level.
Improving Performance by taking Telebehavioral Health to the next level.
Let’s take these six performance objectives one by one to explore what happens when you are taking your telebehavioral health services to the next level.
1. Improved Outcomes
When Telebehavioral Health is executed really well, a number of (good) things happen:
With an increased level of satisfaction on the client side, the willingness to engage more increases. We have also seen a dramatic drop in no shows, since the “care at a distance” aspect eliminates many of the reasons why people don’t make it to appointments – e.g., couldn’t get off work, mini emergency with the kids, too tired to drive, etc. A lower number of no shows, increases the continuity of care (and engagement), leading to improved outcomes due to more frequent touch points.
The second angle on how Telebehavioral Health can improve outcomes is to look at the flexibility (as covered in the last article) that it affords. Clinicians can now more easily match different modalities (e.g., video, phone or chat) to the client’s preferences. Different treatment and assessment tools (even from subspecialized providers) can now more easily be administered and integrated into the remote care giving.
Telebehavioral Health also enables a much better “live” and personal care transition from the hospital to the home, from the home to the Nursing home etc. Without the barrier of patients having to come in, care can now follow the patient. 3-way video calls also make it easier to integrate medical interpreters
Finally, as outlined above, when clinical expertise becomes subspecialized, clients can be better matched to experienced clinicians that have thousands of hours of experience treating the client’s condition, thus making improved outcomes much more lightly.
2. Financial Sustainability
Obviously the concern for financial sustainability in healthcare has always been there, but now that the Covid-19 health crisis catapulted us into the virtual care world, the question about how long and at what level reimbursement will stay “as is”, is consistently on the minds of the CFOs.
I certainly don’t have a reliable crystal ball and can only make a few predictions confidently: that over time reimbursement for virtual behavioral health will be less than in-person care and that reimbursement for telephonic care will (for now) go away (except for check ins). We should, however, over the next 2-3 years see a push to reimburse text-based care and telephonic care reimbursement will see a renaissance, once data gathered in 2020/2021 demonstrates the efficacy of telephonic and text-based care under certain circumstances. But that may just be my rational wishful thinking, too, so don’t bank your business growth on it just yet.
On the commercial side, we may however in some states see a push for payment parity in the wake of politicians’ newly found appreciation and understanding of the power of telehealth (Go Telehealth!). Arizona just passed a law ensuring payment parity and I’m sure other state legislatures will follow (despite the immense pressure exerted by the powerful and rich healthcare payor lobbyists).
But reimbursement is not the only concern when it comes to ensuring financial sustainability. Another positive side effect of a high degree of clinician satisfaction is that retention rates are higher and, for most clinicians, the burn out rates are lower. This leads to less turnover and as we know, replacing a behavioral health clinician can take months if not years and can be very costly in the interim.
The other trend we’ll be seeing soon is the downsizing of the physical brick-and-mortar footprint of behavioral health clinics and behavioral health departments within FQHCs or health systems. While telehealth cannot cover 100% of the patient population, the suitability of telehealth is nowhere greater than in behavioral health. This reduces overall operational expenses and can be used to prepare for those times when virtual care reimbursement does drop below the payment for in-person care.
Telebehavioral Health Business Models
Before we wrap up this week’s column, I want to leave you with this laundry list of various business models that we will explore more in depth in next weeks’ column.
- Fee-for-Service for Commercial, Medical, and Medicare — this is the obvious business model pursued by many. The reimbursement landscape will be shifting, so it’s not as reliable a business model as one would like.
- Direct to Consumer (DTC) Cash Pay — a seemingly lucrative model (because you “cut out” the middle man), but a highly competitive environment that is seeing a lot of influx of venture capital.
- Text-based Counseling — by now everyone is familiar with (and has formed their own opinion on the efficacy of) services like Better Help. There is no rule that says why you couldn’t offer this modality to your clients as well, as your clinicians see fit. That way you add a revenue stream and you don’t lose a client to the competition.
- Subscription Models – Similar to concierge primary care but also similar to many healthcare and non-healthcare business models out there (cf. Amazon Prime, Netflix, and Better Help). Provide the comforting impression of unlimited access and the peace of mind that brings clients.
- Outsource Clinicians (Tele Locum Tenens) — if you have a pool of talented and sought after clinicians or if you are really good at recruiting, maybe the more lucrative (and professionally more rewarding) opportunity may be to offer to other organizations to fill their vacancies with your clinicians. There is ample precedent for this business model.
- Regional or National Specialization — along the lines of what I said above on Subspecialization, find or declare your niche and market your clinicians as the experts as they are to attract more clients and increase the clinician’s experience even more.
- 24×7 ER Pysch Evals — backlogs of psychological evaluations in ERs are a big challenge for ER operators, as is access to psychiatrists at the bedside. The need is greater than what the current in-person demand can satisfy.
- Productization: Assessments, Testing — the Covid-19 health crisis has forced all of us to think outside the box and when it became obvious 3-6 months in, companies pivoted or accelerated their development efforts. By becoming an expert in computerized testing or digital therapeutics, you can carve out a unique niche market.
- Data Monetization (Big Data) — Data is healthcare’s most ignored and most undervalued asset. There are numerous stakeholders who have a vested interest in identifying the most efficacious treatments, so anonymously collected data that can be shared is incredibly valuable for drug makers, treatment designers, and politicians alike.
Our Tele is Here To Stay
Telebehavioral Health is definitely here to stay (“forever and a day”) and there are a number of great reasons why investing in building out and optimizing your telebehavioral health program will yield a high return on investment.
If you’d like to explore how you can optimize physician, client/patient, and staff satisfaction to reap those benefits, schedule a call with me at your earliest convenience.
In the last article in this 3-part series (see part 1 here), we’ll explore the remaining four Telebehavioral Health Performance Objectives.








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.









Leave A Comment