The avalanche of digital health innovation caused by an investment of $100B dollars over the past decade ($60B just in 2020-2022) may be slowing down due to a slowdown in investments caused by the global financial situation, but there is nonetheless a huge mountain of valuable, proven, outcome-changing, cost-reducing, quality-of-life improving digital health innovation ready to be integrated in healthcares’ prevention, diagnosis, and treatment services.
As I alluded to in the last article in this series (“From Idea to Validation”), even the AMA recognizes the chasm between the potential of ready-to-use innovation and its low implementation rate. Many other industries have and are struggling to take full advantage of digital innovation, but no other industry is as slow moving with so much potential left unrealized as healthcare.
As I postulated in the first article on “Innovation in Healthcare”, we must focus on accelerating the adoption of innovation. As an industry and as a society expecting quality care, we must learn to evaluate and prioritize ideas in days, validate them in weeks and implement them in months.
The Roadmap to Implementation Success
This fourth article in the series will (in two parts) lay out the structure and approach to successfully and sustainably integrate digital health solutions in the traditional care delivery processes, simultaneously using a small number of proven tactics and best practices, long practiced and mastered by other industries.
To succeed, the primary mindset must come from an acknowledgement and realization of the small and big changes that clinicians, nurses, staff, and even patients have to accept. Secondly, and almost as important, as a service industry, the critical focus must be placed on workflows and operationalization. Given the complexity, the next approach on the road to success is to validate assumptions and adopt the solution to the environment in which it is implemented through a Proof-of-Concept.
With those three phases completed, training can commence to start the project-managed full deployment of the innovation. Lastly, to truly unlock the potential rewards of the innovative digital health solution, the organization must monitor and manage its performance. “Build it and they will use it” is just hope and not a solid strategy.
Change Management Planning
Healthcare changes its ways notoriously slow. Aside from humans’ innate resistance to change, here are two understandable and valid reasons specific to healthcare: first, changes can be risky and a mistake will not just result in an inconsequential wrong side dish of French fries vs. a side salad, but can impact a patient’s health, their quality of life, or even cost them their life.
Secondly, a physician’s foundational education takes about 15 years, during which they typically do not deviate much from their preceptors instructions, leaving little exposure to experience change on a larger scale.
While all the other elements described below greatly increase the chances of a successful, sustainable implementation, they are not sufficient in themselves with proper attention to managing the change.
Confusion, Resistance, Reluctance, Frustration, and going back to the old ways are all various forms of avoiding change. And they all have different root causes!
Confusion is the result of not understanding the rationale behind the change, the why — or in this case, the benefits of the new digital health innovation to be implemented. Confusion is caused by a lack of Awareness.
Resistance stems directly from a lack of motivation, a lack of buy in. While it could result from a lack of understanding the reasons behind the change, it’s simply a lack of Desire that results in resistance.
Reluctance is often caused by the desire not to look stupid. It is the lack of Knowledge that makes people hold back and not give “the new thing a try”.
So what about Frustration? This reaction is especially damaging, because typically Awareness, Desire, and Knowledge are all present — but the Ability to do it well is not. Which leads to frustration and to giving up on trying.
Finally, going back to the old ways happens all too often, when there is no accountability. Lasting change requires Reinforcement – providing support where it is needed and accountability where it is called for.
This model, called ADKAR® for the initials of the five change management tactics, was developed by the PROSCI Institute. It is a simple and effective framework for planning for and managing any organizational change.
So in order to prepare for the various forms of change resistance, the implementation team must first plan the following activities.
- Raise Awareness about the strategic, financial, and clinical value of the innovation.
- Create Desire of wanting to use the innovative solution, or at least to give it a chance.
- Supply sufficient Knowledge about the innovation and how it fits within the healthcare delivery workflows.
- Establish a proficient Ability by providing ample training and support.
- And finally provide Reinforcement by monitoring and managing the utilization and performance of the innovation.
Workflow Design
Healthcare is in essence a collection of interdependent, overlapping, and interacting service delivery processes. Aside from the conscious, proactive change management, the success of any successful innovation adoption depends on the team’s clear understanding of the future workflow required by the innovation — and the impact on the current, well-established workflow.
The successful rollout of a digital health innovation is to clearly understand and document what needs to happen prior to and after the innovation is leveraged.
For example with a televisit solution as the digital health innovation, prior to the actual televisit, the patient needs to be scheduled, prepared, and roomed. After the visit, the clinician must hand the patient off to the next step and properly document and code the visit. Others may follow up with the patient and the visit must be claimed for reimbursement.
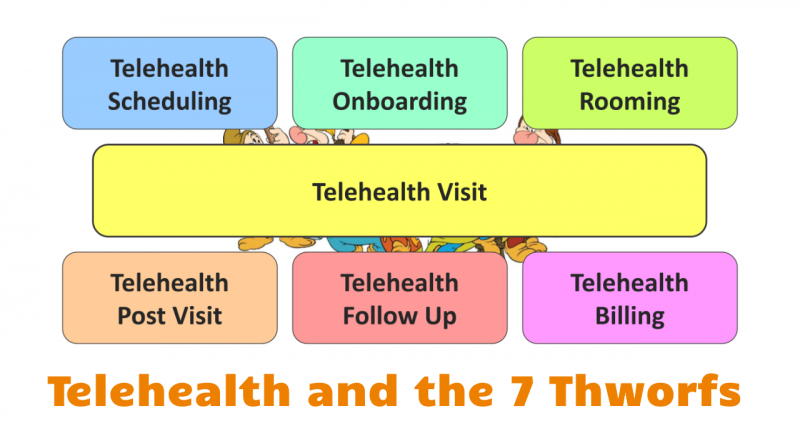
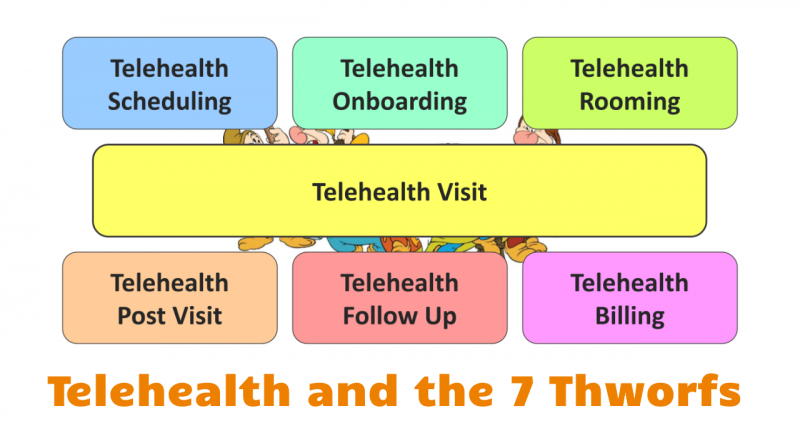
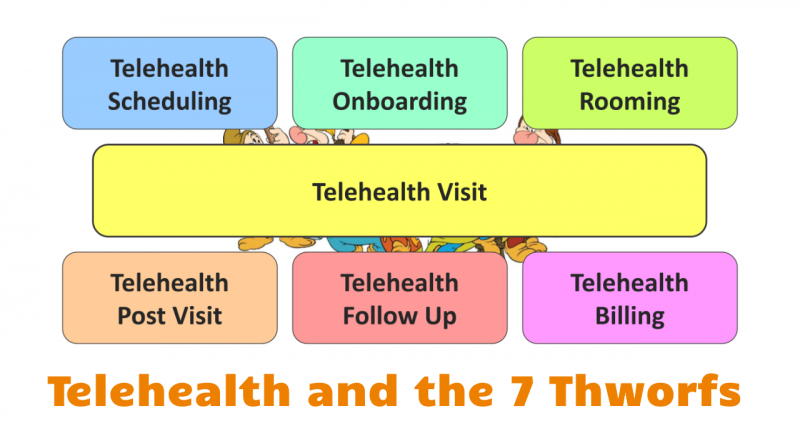
Given the multitude of interacting and interdependent workflows that are required for any digital health solution, it is important to clearly identify the hand-off and synchronization points between workflows — and appropriately train everyone involved in each process.
A great tool for successful workflow design is to start with defining the Happy Day Scenario — what should happen normally, 80% of the time. Oftentimes workflow design efforts get derailed because the team thinks about everything that could happen at every step, without ever designing the optimal experience that would be considered “normal”.
Operationalization
Once the workflows have been identified, it is time for the team to consider how the solution is going to be supported operationally in the long run. How do those workflows get implemented? Who trains the various participants in the workflow? Who provides support when something goes wrong? Who monitors the performance and intervenes if the solution is not performing as expected?
Whereas the Workflows focus on the use of the digital health innovation (e.g., the televisit platform), operationalization focuses on the peripheral aspects of making sure that the core and supporting workflows will run smoothly.
Proof of Concept: Validation and Refinement
The approach of testing the solution on a smaller scale is not new, and is often called a pilot. Most of the time it is either time bound (“let’s try this for 6 weeks”) or volume bound (“let’s run this on 30 patients”).
Ideally, the team uses a pilot for refinement: improve the workflows, identify new support needs and optimize the configuration of the solution. However, acceptance criteria (or exit criteria) rarely exist, and if they do are informal — did it work? did the clinicians like it/find it acceptable, useful?
While that approach is better than jumping right into a deployment, it still misses by far one of the severe omissions made: not validating assumptions, especially those assumptions that are hidden: implied and implicit.
During the design phase, most people (including the developers of the innovative solution) are making dozens if not hundreds of assumptions — e.g., about how physicians are going to use it, how patients are going to use it, the level of digital literacy, access to technology, availability of privacy, etc.
The goal of the Proof-of-Concept (PoC) phase, aside from refining and optimizing the solution, is to validate assumptions.
To launch a Proof-of-Concept, the team must first catalog all explicit assumptions and then identify the implicit, hidden assumptions. After a prioritization of which assumptions are most important, the team must then develop ways to validate the most important assumptions through a variety of objective and subjective measurements.
In a Happy Day Scenario, the PoC ends when all important assumptions have been validated. That can take a week or five months. But as long as tweaking and refinement is needed, the PoC creates a tremendous amount of value for very little investment.
Implementing Digital Health Solutions, Part 2
In the second part of this article we will address deployment project management, the various forms of training, and how to design a post-implementation performance monitoring and management system.
What else would you like to know about the successful, sustainable implementation of digital health innovation?








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.








