In the 2000s people would remember vividly where they were on 9/11/2001 when the news broke of the attack on the Twin Towers in New York City. In the 2020s many people will probably remember where they were when the realization hit, around March 18, 2020, that the threat of Covid as a global epidemic was real.
The week of March 16, 2020 I was in rural Vermont, working with a Federally-Qualified Health Center on their gradual improvement of their school-based telehealth program and their use of telehealth in behavioral health.
As the reality sunk in for the clinical leadership on Wednesday, March 18, the CEO turned to me and said: “Christian, by when can you have telehealth up and running for our five primary clinics?” Given what I had learned in working with the organization for a few months, I replied: “You’ll have it by Friday”.
I wrote about it in my Telehealth Tuesday on March 24, 2020, which you can revisit here: Covid-19: Launching Telehealth in 5 locations in 2 days
Revisiting the Lessons Learned
In my article from two years ago I highlighted 7 lessons that I’d like to revisit with the hindsight of two more years of experience in implementing and optimizing telehealth services.
- Emphasis on workflow is crucial.
- In a time of crisis, attention to detail is limited
- Training on telemedicine can truly occur in less than half an hour
- Capturing data is key.
- Designing the process for long-term is easy to do, but hard to sell
- Direct-to-Consumer Telemedicine is truly one of the most challenging telemedicine use cases
- Clinical Leadership involvement is key
Workflow & Process (#1, #2, #5)
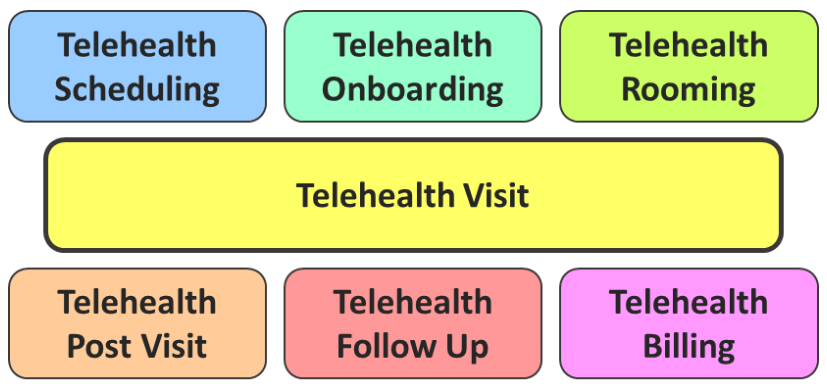
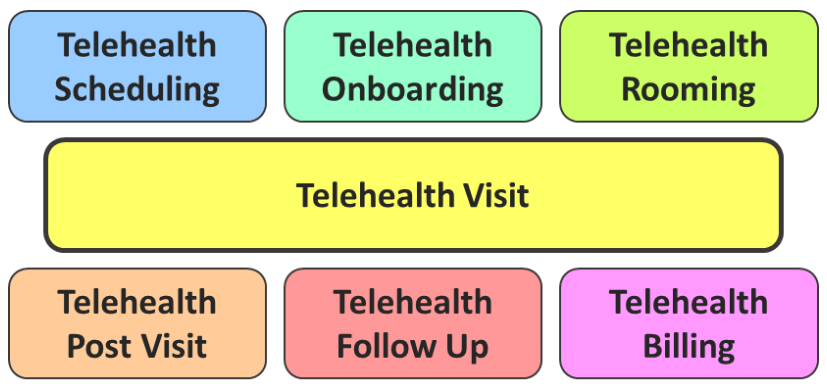
Workflow continues to be the single most important ingredient in telehealth success. Since there are at least 7 core workflows that need to be defined for telehealth, it is easy to relate that staff are frustrated when they do not understand what steps to follow, e.g., to schedule an appointment, “room” a patient, provide a referral, or how to bill.
I cannot stress enough the focus and time that each telehealth support team has to invest into designing, documenting, measuring, and optimizing telehealth workflows.
Even now, two years after most organizations rapidly launched telehealth, there exists great confusion in organizations who had little to no exposure to telehealth prior to the health crisis.
Limited Ability to Absorb Change (#2, #3)
While in 2020 I attributed the staff’s limited ability to pay attention to detail in the workflow to the crisis, I have now come to understand that most healthcare staff — support staff and clinicians alike — are in constant mild crisis or change overwhelm mode.
On the one side they are deeply committed to great patient care and great customer service; on the other side are the demands of new laws and regulations and an overall emphasis on doing better, on improving, initiated by leadership.
Thus between “doing the work” and “doing the right thing” it can be tricky to absorb yet another process communicated via email “in between breaks”.
What I have learned from these experiences in the past year is (1) that process design cannot be designed top down (or from the outside) and (2) that training cannot not happen through email or documented procedures. The latter may work for some personalities, but it’s ill-suited for most.
To bring about change, new information needs to be deliberately disseminated in digestible bite-sized chunks and communicated in a distraction-free environment (e.g., a training class).
#4: Driving in the Dark with the Lights On…
…may be exciting — but is also very dangerous.
It’s still astonishing how many telehealth programs are running without any good insights into its performance – whether that’s the simple statistics on the volume (and whether it was video or telephonic) or satisfaction levels of clinicians and patients. Most leaders are pretty much in the dark on how their telehealth services are doing.
Setting up an initial set of metrics can be daunting, but once established can easily be done on an ongoing or periodic basis.
The next holy grail of telehealth performance measurement is to see its impact on outcomes, which is what a few of the highest performing organizations are currently looking at.
#6: Direct-to-Consumer Telemedicine Remains Hard
Most of our work is in rural America and while suburban America, especially among the Medicaid population, is also experiencing technology access problems, the problems are exacerbated in the sparsely populated areas of the US (such as the North Central part of Washington State or the Southwest corner of Virginia).
But connectivity (characterized by access, bandwidth and latency) aside, the mere availability of suitable technology and the limited digital literacy are clearly posing great challenges.
For the first 12 years in telehealth, for video visits I exclusively implemented solutions where the patient (mostly for reimbursement reasons) had to present at a (remote) clinic to be seen by a (distant) clinician. The public health emergency’s lift on the location of the patient was a boon to telehealth – but also presented an unprecedented challenge: teaching patients how to use technology (right).
To address this problem (and to not waste the clinician’s time with technical trouble-shooting), all successful telehealth programs are now integrating their own flavor of a Telehealth TechCheck process. This ensures that both patients and clinicians can have productive visit – and it can also help in managing and setting patient’s expectations for the visit.
#7: Leadership is Key
In summary, not really much has changed in 2 years. While the sense of urgency to stand up telehealth rapidly has dissipated — for now — the challenges we had to overcome two years ago in a matter of days remain the same, as does the approach for overcoming them.
If anything, it may have become harder to motivate staff and clinicians to take on telehealth. At the height of the Covid-19 health crisis the alternatives were telehealth or no care. Now, we have a choice between “novel” telehealth and “familiar” in-person care.
Which is where leadership, both executive and clinical, comes into play.
As great leaders recognize, the telehealth landscape is already changing and is becoming more and more ubiquitous. And when modern healthcare consumers have choices, most will go for convenience first, cost second, and quality third. Thus telehealth, in some cases, may soon become an existential threat to current business models.
Once the clinical leaders of an organization fully embrace telehealth as a viable care delivery method in a hybrid care environment, then telehealth has a chance of succeeding, as clinicians will more likely follow the lead of a fellow clinician who believes in telehealth.
And that may be the biggest lessons learned – in 2020 and in 2022.
I’m curious: what additional lessons have you learned over the past 2 years?








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.









Leave A Comment