For decades, our traditional healthcare system has relied on patients coming into the physician office to receive their care. Many of the workflows we know today were designed about that basic paradigm: The assumption that in order to receive care, patients have to come to the physician’s office.
With the Covid-19 health crisis this all changed and telehealth was catapulted into the limelight and now presents a viable, efficacious way to deliver care under many circumstances.
Most healthcare organizations with no prior experience in telehealth chose the “here’s a webcam and a video chat license” approach to telehealth in response to the public health emergency.
Workflows for the Telehealth Model
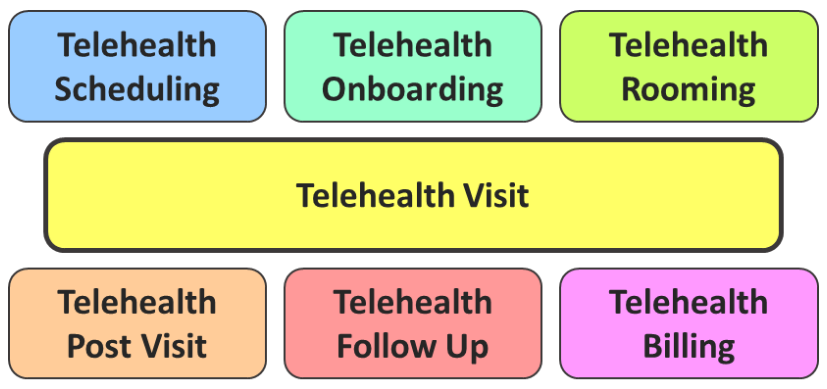
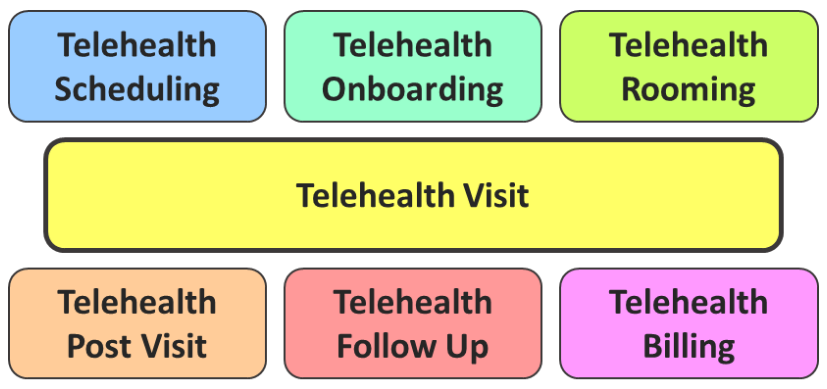
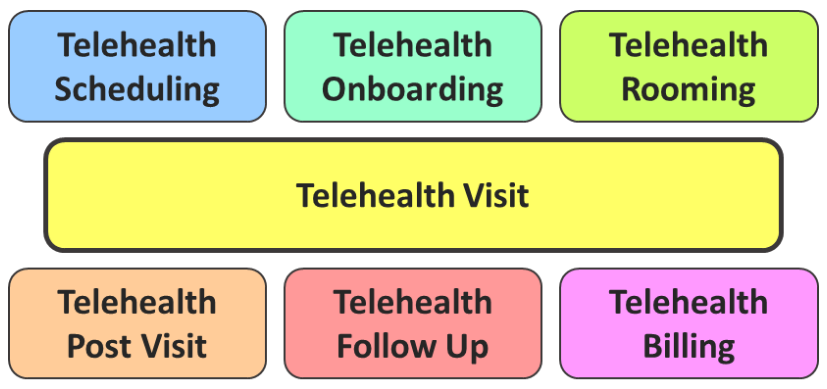
In most organizations, none of these workflows were consciously redesigned for a telehealth environment. Yet without physical access to the patient, many of the steps in the “in-person” world cannot be easily recreated in the “virtual” or “at a distance” world.
Including the collection of Copays.
Collecting Copays
Now that we are approaching the two-year mark of the health crisis many organizations realize that telehealth is here to stay and that a viable telehealth service must include the collection of Copays, especially when required by the payor.
Yet, with patients no longer stopping by the front office on their way out, the enforcement of a Copay policy has proven challenging to enforce.
Obviously it is not and neither should it be the clinician’s nor the nurse’s job to handle financial matters. It has long been a hallmark of our healthcare delivery process to clearly separate the administrative from the clinical – and for good reason, so that clinicians and nurses can focus on what they do best.
Given that telehealth is not going to go away, what options do healthcare leaders have to ensure that copays can be collected in the context of a telehealth visit?
Workflow Solutions
Looking at the chart of workflows above, the best time to collect a Copay before the visit would actually be as part of the TeleRooming process – i.e., when the nurse prepares the patient and clinician for the visit by taking/recording vital signs and the chief complaint.
Now that the patient is actually having the visit, a simple phone transfer to patient services before or after talking to the nurse can take care of the Copay right before the visit via credit card — just as many practices are doing in the “in-person” world.
Based on some anecdotal stories we’ve heard over the past year, it appears that in some patients’ minds a telehealth visit is actually quite different from an in-person visit. This may result in resistance or outright refusal to pay the Copay for a telehealth visit. To determine the best course of action in this situation, rather than reinventing the wheel, consult your traditional Copay collection policy to explore how you would handle such a situation in an in-person encounter and then transfer the same rules into the virtual care world.
Should you run into resistance from patients frequently (resulting in cancellations), the best first solution is to update your communication to the patient at the time of scheduling and when sending out visit reminders, to include language that explains the expectation to provide a Copay prior to the visit. Oftentimes patients are merely caught off guard, never having had a telehealth visit before that required a Copay.
If the tradition in your practice has been to collect copayments after the visit during the checkout and follow-up scheduling process, then you could implement a similar process for the virtual visit, though it bears more risk of not being able to reach the patient after the visit.
The best solutions here are a timely follow up call (within minutes) or, even better, a true virtual hand-off back to the nurse (e.g., audio-only) and then on to the patient service representative is the best way not to “lose” the patient, ensure collection of the copay and along the way provide extraordinary customer service by addressing their needs (e.g., for scheduling lab tests, obtaining referrals) and their questions.
Technology Solutions
Such a specialized solution can provide a more reliable, patient-friendly and much less resource-intensive approach than the workflow solutions described above. While traditional healthcare organizations are only slowly opening up to leveraging the online world (such as social media or online scheduling), secure and reliable ePayment collections have now been around for over two decades. And hardly anybody could claim they have not bought anything on Amazon yet. These days, many healthcare organizations are still relying on either simple, consumer-grade video chat solutions (hopefully in a HIPAA-compliant way) or on their EHR’s telehealth add-on functionality. But these tools were either never designed for the healthcare environment or often-times quickly cobbled together to provide a quick solution in response to the Covid-19 health crisis. As we have learned over the past 10 years, most EHRs’ core capability is to improve billing and billing accuracy, not the support of the patient or physician experience, though the collection of Copays would fall into the purview of an EHR vendor.
As any surgeon and as any carpenter or mechanic knows, the best investment is into tools that were specifically designed for the task at hand. The same holds true for software solutions that were specifically designed to support telehealth visits and exams.
The video conferencing aspect of telehealth software is actually the easiest part. It is much harder to design a solution that integrates into and supports the clinical and administrative workflows. From screen sharing (to share lab results or websites), file sharing (to send forms, brochures, or reports), secure chat, or the transfer of patient-related information into the EHR, telehealth-specific software can support a smooth telehealth experience much better.
But such custom-designed telehealth solutions are not an oddity. Even before the Covid-19 health crisis we were tracking more than two dozen software solutions specifically designed to support telehealth. Nowadays we have lost count, but my guess is that there are about a 100 different dedicated telehealth solutions available in the US.
The best of these solutions provide support for an easy scheduling, for an easy intake process, for secure communications before, during and after the visit and much more. Many are moving into the integration of remote patient monitoring devices and patient-generated health data, further enhancing the value of these specialized solutions.
In case you were looking for examples — as a technology- and vendor-agnostic consultancy we do not promote specific vendors, since we do help healthcare organizations to identify and select a telehealth solution that best fits their needs. To get started on your own, a simple Google search yields about half a dozen software review sites that list 180 or more solutions.
Conclusion
Depending on your patient population, their openness and responsiveness to provide a Copay at the time of the visit, you may explore in small proof-of-concept projects the viability of any of the aforementioned solutions:
- Workflow Solution A: Collect Copays right before the visit
- Workflow Solution B: Collect Copays at the time of a follow-up call.
- Technology Solution A: Switch to specialized Telehealth Software that includes Copay collections (and many other features)
- Technology Solution B: Explore your patient portal’s capabilities to collect payments
- Technology Solution C: Provide an online payment portal that you can direct patients to








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.









Leave A Comment