Over the past years, telehealth has proven itself to be a viable approach to delivering care safely and effectively in many cases, under many circumstances. While telehealth will never replace 100% of in-person care, we can and we should get to using telehealth 100% of the time — when appropriate.
While a future is imaginable where all of our care and in fact many services supporting daily living are delivered virtually, this is not the purpose of this article 3 ½ years out from the Covid-19 health crisis.
Rather, this week’s column is about getting healthcare to use telehealth as a clinical tool judiciously yet much more often than currently is the case.
100% Telehealth, defined
Getting to 100% Telehealth does not mean that there will be no more in-person care, not even in the outpatient setting. Rather, 100% Telehealth% means using telehealth 100% of the time when it is appropriate.
100% Telehealth — Using Telehealth when all criteria are met:
- The patient desires, prefers, or is open to telehealth.
- The patient has the technical capabilities and digital literacy.
- Telehealth is clinically appropriate for the patient.
The broader term telehealth here refers to “delivering care at distance” which includes “practicing medicine at a distance”, including video visits (with or without exam capabilities), remote physiological monitoring of key vital signs (RPM), or the store and forward analysis of data, images, video, or sound.
Customer Service First: First off, healthcare, as an industry, has an increasing mandate to cater to the desires and the wants of the “modern healthcare consumer”. Gone are the days where the local clinic was the only choice. Nowadays, patients have options — whether it’s urgent care, convenience clinics, or online care options. The monopoly of traditional healthcare has been dismantled. Thus if patients desire accessing their care virtually, healthcare organizations that want to stay in business must offer those services to patients.
It’s not about the technology: Secondly, the patient (and of course the clinicians) must have the technical capabilities of participating in virtual care. This primarily includes the patient’s digital literacy, availability of the appropriate technology, and sufficient and reliable connectivity. While the technology can and should quickly fade into the background, it does have to work and be operable in a user-friendly way.
Do No Harm: Last, but certainly not least, based on the patient’s situation or condition, the type of care or medical service to be provided must be clinically appropriate for the virtual care environment. No one would argue that in order to schedule an appointment for getting a copy of the lab results anybody would have to come in person. But at times, e.g., for a visit that requires closer examination or specialized tools, in order to confidently make a diagnosis or assess progress toward health, telehealth may not be the appropriate modality.
It’s All or Nothing
For telehealth to be an effective alternative to in-person care, all three of the above criteria must be met.
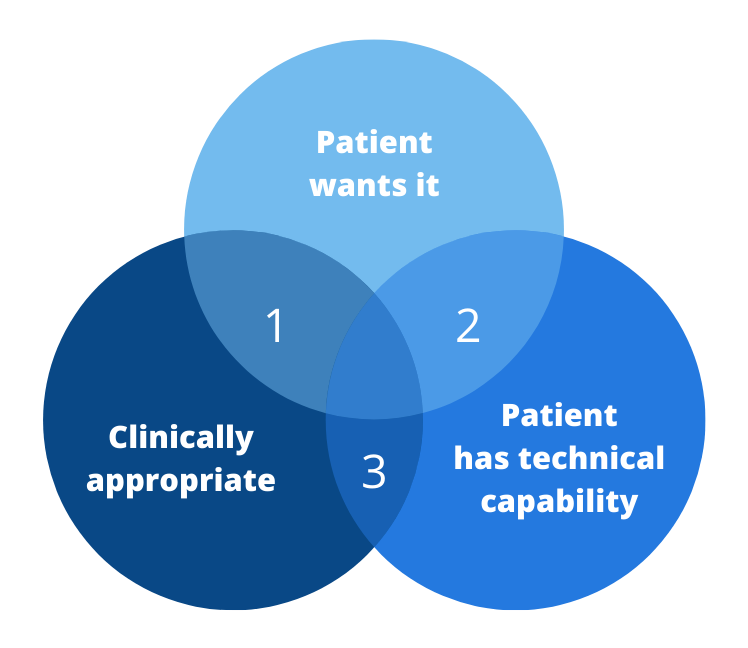
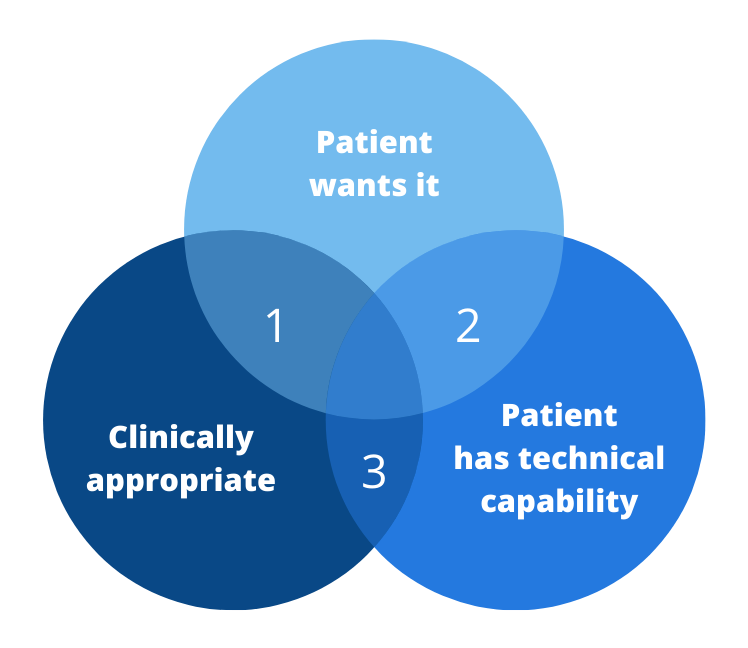
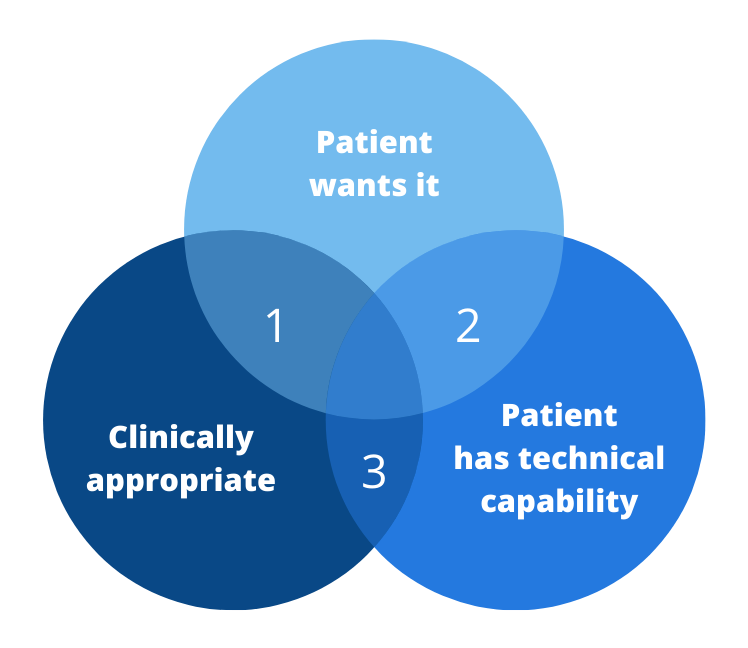
If only two of the three are met, the results are highly unsatisfactory, as the diagram shows.
Intersection 1: The patient wants telehealth and it is clinically appropriate, but the patient does not have the technical capability.
We all know from the experience in 2020 and even now what that experience is like: Pure Frustration. When the connectivity causes the video to stutter, when hours of technical troubleshooting on how to connect the Bluetooth blood pressure cuff to the remote monitoring hub yield no results, then we know that telehealth was not the right solution for this patient.
Intersection 2: The patient wants it, has the technical capability but it is not clinically appropriate.
In this case, using telehealth in this case could be considered as malpractice – most likely not in the legal sense, but more as in using an ineffective approach to diagnosis or treatment, which ultimately will have to result in an in-person visit. But at times, especially in a value-based environment where there is less concern about reimbursement for every service rendered, a triage via a video visit may very well be the best first course of action if the patient cannot be easily seen in person.
Intersection 3: Telehealth would be clinically appropriate and the patient would have the technical capabilities, but simply does not want to use telehealth.
This scenario is often overlooked by ambitious, techno-loving services that favor a “virtual first” approach, resulting in doing patients a disservice. But even under those circumstances a brief virtual triage could go a long way in most cases and the experience may help to overcome patients’ reservations, even if the outcome of that telehealth service is that “we’ll have to see you in person”.
Three Key Changes to Get to 100%
To be clear: Unlike some slogans that tout that “healthcare = telehealth”, I’m not proposing (quite yet), that all in-person care (or, all in-person outpatient care) must be replaced by telehealth to get to 100%.
Rather, I’m encouraging healthcare leaders to approach this opportunity from three different angles that are present quite a shift from the “traditional” approaches and attitudes of the past.
1. Focus on customer service
This speaks to the first two patient-centric criteria for ”100% telehealth”. And it’s not just about putting the needs of the patient first, but about making the experience or receiving care an extraordinary one.
Thus first, in order to find out whether patients desire, prefer, or are open to telehealth you first have to ask them. In the past decades patients were seldom asked about their preferences, especially not about how, when, and where to receive care.
Secondly, and this is often a bigger stretch, healthcare organizations have to get involved in setting patients up for “technical success”. That means getting involved in improving digital literacy, advocating for better connectivity and preparing patients for telehealth, e.g., through a pre-visit Telehealth TechCheck℠.
2. Define Your Own Clinical Guidelines
While many national organizations and associations are working on the appropriate telehealth guidelines and standards, the different nuances of telehealth are too vast, for now, for these “national” efforts to address all circumstances.
In our work with our clients we facilitate a process for the clinicians to discuss among themselves to identify what the appropriate standard of care should be under various circumstances. When is telephonic care appropriate? When do we need video? Which remote exam tools should we be integrating? When is in-person care the strongly desired choice? Which patients are suitable for RPM?
3. Declare, Educate and Train
To get to 100% telehealth, clinical and executive leadership must declare it as a strategic priority to serve patients the way they want to be served, when appropriate.
Next follows a series of communications to clinicians and to staff along with marketing to the patients to encourage patients to enquire about the availability of telehealth for their next visit or for their care.
This is then topped of with training — on the technologies (e.g., how to use a remote exam tool), on the policies (e.g., what are the appropriate webside manners), and on the workflows, including the scripting for schedulers to use to offer telehealth as an alternative to an in-person visit.
It’s all about Outcomes
The goal of 100% Telehealth is not about Telehealth itself.
It is the delivery of extraordinary care that leads to quick and accurate diagnoses and engages patients in the appropriate care.
Because if patients cannot come to an in-person appointment, a video visit will “beat” no visit any time, leading to continuity of care, possible early detection of conditions, and timely interventions.
Telehealth is a clinical tool that when wielded correctly can offer a whole new world of caring for patients appropriately. And ultimately that’s what it’s all about.
Do you want to start a conversation among your leadership team and clinicians on how to get to 100% telehealth? Contact Christian for free guidance on how to facilitate that discussion.








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.