After many decades of slow progress, telehealth adoption is at last growing exponentially. According to a survey of 800 physicians, the number of physicians who have used telemedicine went from 5% in 2015 to 22% 2018 — an exponential increase of doubling the adoption rate every 18 months, which is quite an outlier in an industry which historically has achieved adoption rates only after 17 years.
Why prioritize?
Telehealth is most simply defined as delivering healthcare at a distance and with that definition telehealth practically is healthcare — the only difference being that the physician and the patient are no longer constrained by being in the same room or even having to interact at the same time. For any health system there are therefore dozens if not hundreds of use cases for telehealth, by multiplying dozens of specialties with a dozen or more locations where the patient can be (e.g., at home, at work, at another clinic, at an ER or an ICU, etc.), multiplied by the different modalities of interactive, remote monitoring, and store & forward.
For any healthcare organization adopting telehealth, the rollout of telehealth is first and foremost an exercise in organizational change management: workflows needs to be changed, new technology needs to be deployed and trained on, and more often than not, minds need to be educated about the merits of telehealth. With time and money being the key priorities of any enterprise, organizations need a robust process to identify the most important telehealth use cases to launch next.
How to prioritize telehealth use cases
It bears repeating that telehealth is not really about the technology: it’s about changing the way healthcare is being delivered. When these changes are financially sustainable, offer medical care of the same quality as in-person care, and improve access to care for patients, then the business case for telehealth is clear.
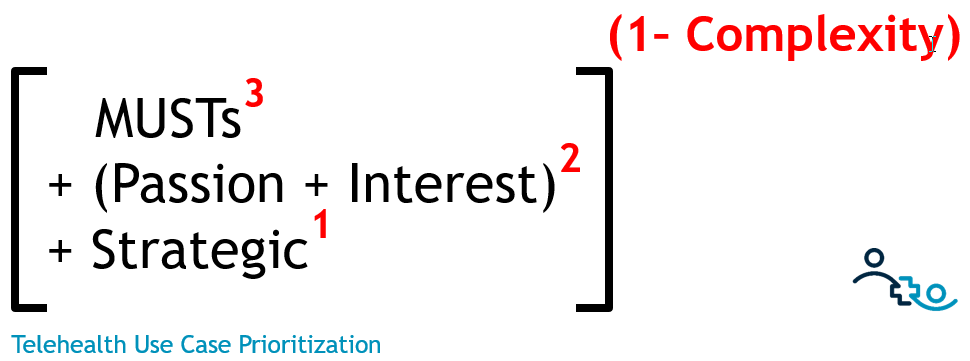
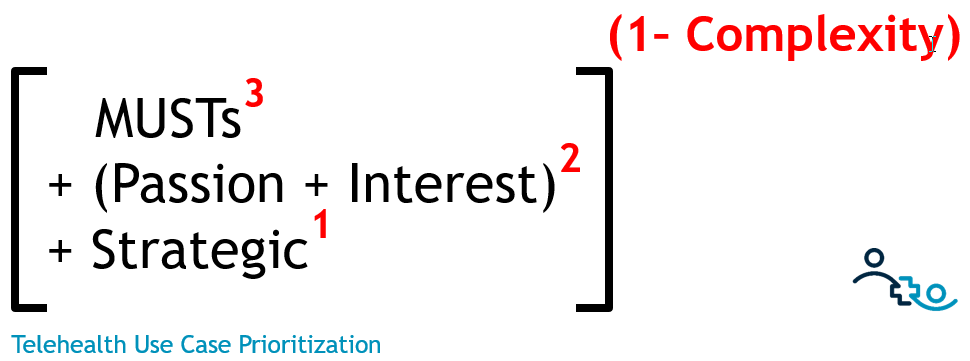
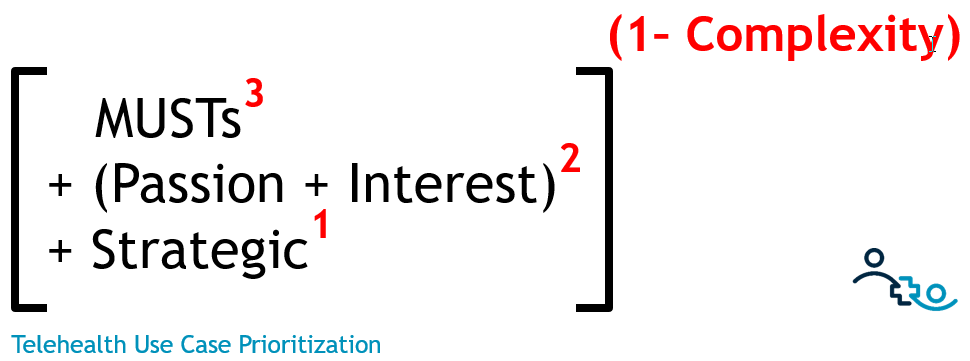
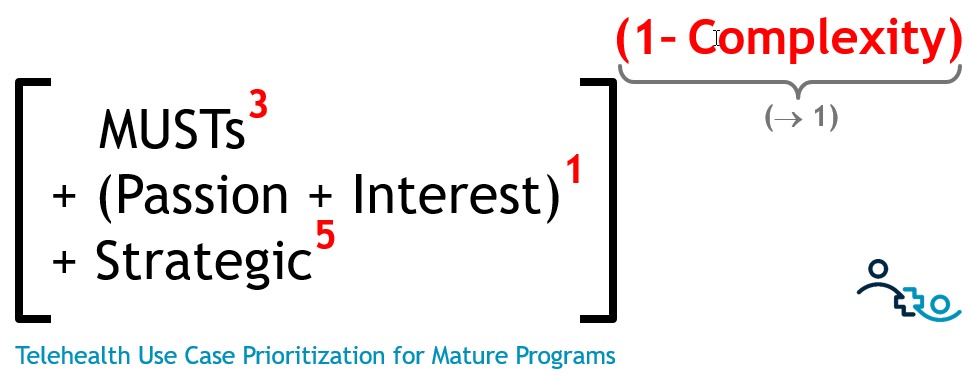
As an engineer, I like processes and formulas. As I worked with different organizations over the years, I developed a formula for prioritizing use cases. I recommend organizations consider four factors, which go into my formula with different weightings:
- The Musts, i.e., the contractual or legal obligations that require your organization to offer a telehealth service
- The Passion/Interest of the affected clinical and medical staff
- The Strategic alignment of the telehealth use case with your telehealth strategy
- The Complexity in setting up and rolling out that particular telehealth use case
Combined, the formula reads as follows:
Breaking it Down
So what do you need to consider when assessing the four factors for prioritizing Telehealth Use Cases?
- MUSTs^3 (0-10, cubed): This assessment relates to regulatory or contractual compliance – the obligations that your hospital or health system must meet. Many of the new programs coming out of Medicare or Medicaid now stipulate the use of telemedicine (e.g., ET3 or Maryland’s Comprehensive Primary Care Model).
- Passion/Interest^2 (0-10, squared): This factor links your priorities directly to the attitudes of the affected healthcare professionals. A physician who is excited to integrate telehealth into her practice will go a long way to make the telehealth service rollout a success.
- Strategic alignment (0-10): If you have a defined telehealth strategy, every telehealth service under consideration obviously needs to align strongly with the strategy. If you do not (yet) have a strategy, you need to assess the impact of the telehealth service to achieve the organization’s overall strategic objectives (e.g., ‘reduce readmissions’ or ‘improve access to care’).
- Complexity (0-1): This factor, which carries the most weight in the formula by going in as an exponent, represents the anticipated difficulty of rolling out the telehealth service. It’s the combination of three factors: the technical complexity (i.e., a TeleICU solution requires more complex technology than a behavioral health televisit), the complexity of the new workflow and the complexity of the change, i.e., how many people will be affected and their level of buy in.
The one factor everyone forgets when prioritizing Telehealth Use Cases
Can you guess which of the four factors most organizations ignore?
Most organizations, especially those with telehealth programs lacking central coordination, prioritize merely based on the interest and drive of a single physician. Many organizations are also opportunistically techno-centric, wanting to simply find additional use cases for the technology they have already in place, which could be considered strategic, if it is done consciously. Others, who are CFO-driven, look primarily at the financial drivers, which can be considered strategic or a ‘must’.
But very few organizations have the awareness, or even the skills, to assess a telehealth use case’s complexity. And as you can see from my formula, it is the most critical factor, in particular for new programs.
So, when you are deciding which telehealth service(s) to launch next, make sure you spend adequate time with the right people to accurately assess and predict each proposed use case’s technical, workflow, and change complexity.
Only then will you be able to allocate your priorities of time and money most effectively and efficiently to the launch of a successful telehealth service.
How does the formula change over time as our telehealth program matures?
I’ve referenced a few times above that this particular formula is mostly applicable to organizations starting out in telehealth. But over time, as programs mature, the weighting of the various factors will change.
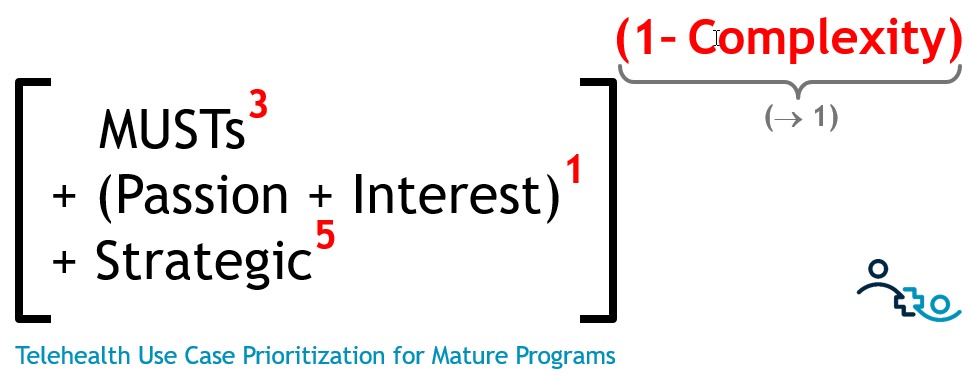
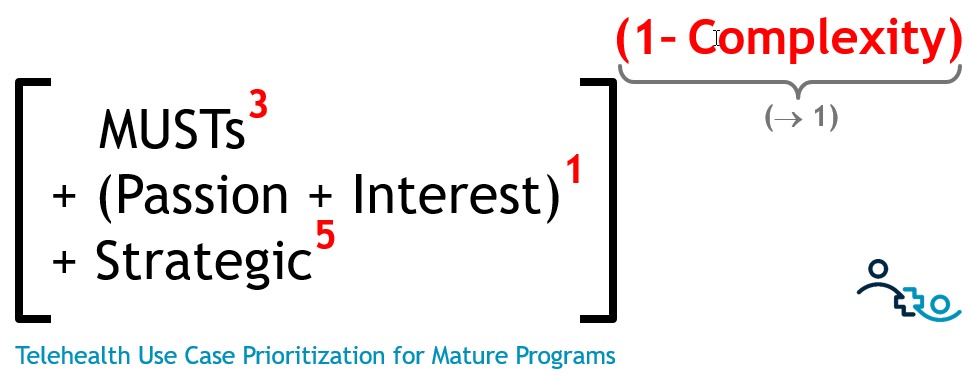
While passion/interest is a determining factor at the very start of a program it will become less critical as telehealth becomes the accepted norm.
Once an organization has a dozen or two telehealth use cases under its belt, the complexity factor will asymptotically approach 0, thus losing it’s domineering grip on the prioritization formula. But as you venture again into unknown telehealth territories (e.g., ad hoc direct to consumer telehealth or telestroke) the complexity factor will still dominate the prioritization.
On the other hand, your contractual obligations (the ‘musts’) are likely to grow as government programs reward the use of telehealth.
The biggest change for mature programs is that they are clear about their strategic direction of their digital health/telehealth programs and thus ‘strategy’ becomes the most dominant factor in the formula.
Prioritizing Telehealth Use Cases
The most pragmatic way to use the formula is to discuss a newly proposed telehealth services using formula’s four factors to guide your decision making process, with special consideration given to the complexity so you can increase the likelihood of a successful rollout.
What prioritization mechanism are you using in your organization? What other factors are you considering that are not listed here? Share your experience with other readers in the comments below.








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.









Leave A Comment