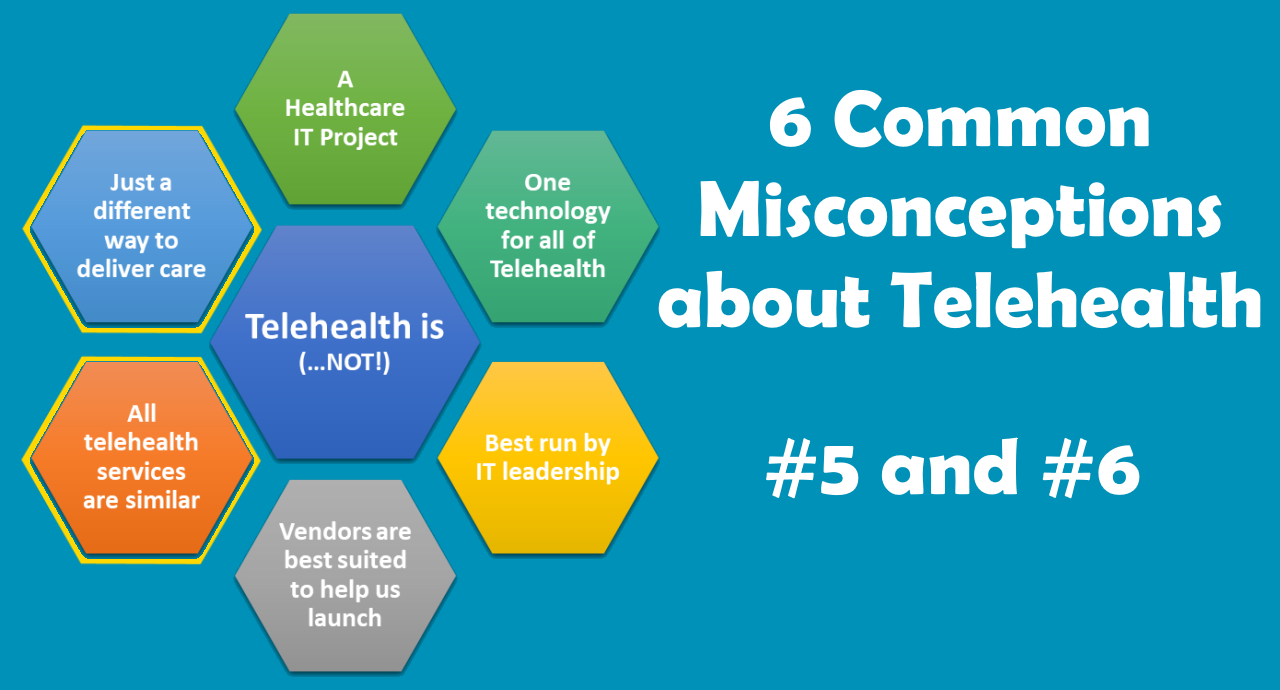
A few months ago, before the start of the Covid-19 health crisis in the US, I wrote a series of articles about the 6 common misconceptions about telehealth:
- That the launch of telehealth is an IT project.
- That there is one technology for all of telehealth.
- That telehealth is best run by IT leadership.
- That telehealth vendors are best suited to help launch telehealth.
- That all telehealth services are similar to each other.
- That telehealth is just a different way to deliver care.
Especially given that there are so many individuals who overnight had to become “telehealth experts” to launch telehealth in their organizations, I am finishing my series by focusing on the last two remaining misconceptions, #5 and #6.



Misconception #5: All Telehealth Services are similar to each other
Or stated in other words: Once we’ve established one telehealth service, we are doing telehealth.
The reality is, that “One swallow does not a summer make“. If you have established a single telehealth service, you have simply established a single telehealth service.
There are a great number of differences between the dozens or even hundreds of different types of telehealth services. And even if most things stay the same (same organization, same patient demographics, same geographic area), just moving from behavioral health to primary care or from pediatrics to behavioral health changes a lot of the key elements that make out a telehealth service, such as the workflows, policies, and the technology.
Most health systems will over the next months and years launch about 50-60 different telehealth services with smaller practices or rural community health centers looking at launching about a dozen different services.
Yet many organizational leaders and staff believe that since they launched one telehealth service, they are already “doing” telehealth, when in reality what they have is one or two telehealth services launched.
The Big World of Telehealth
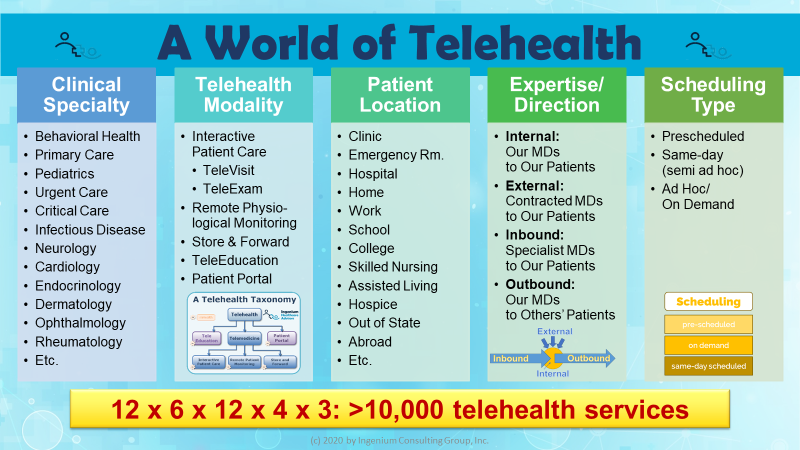
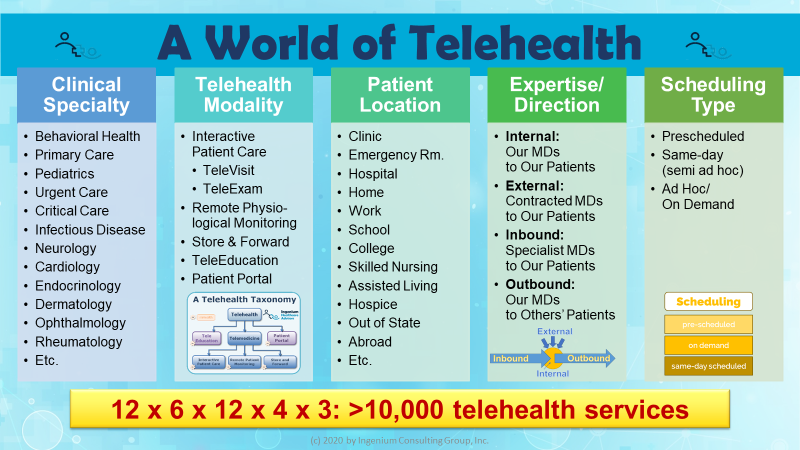
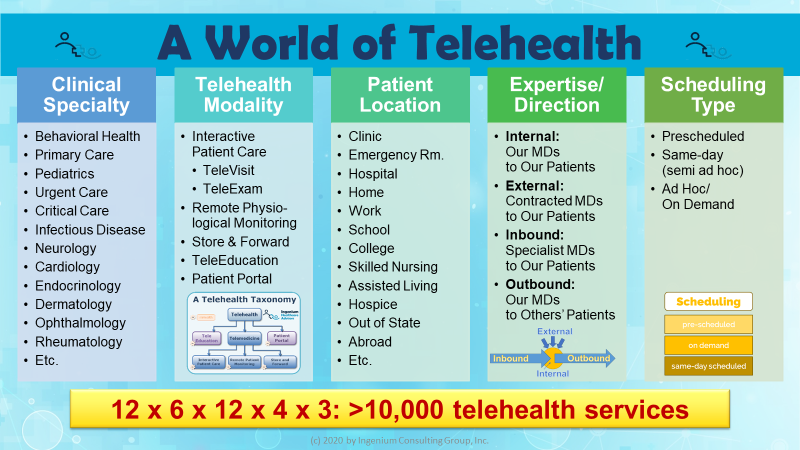
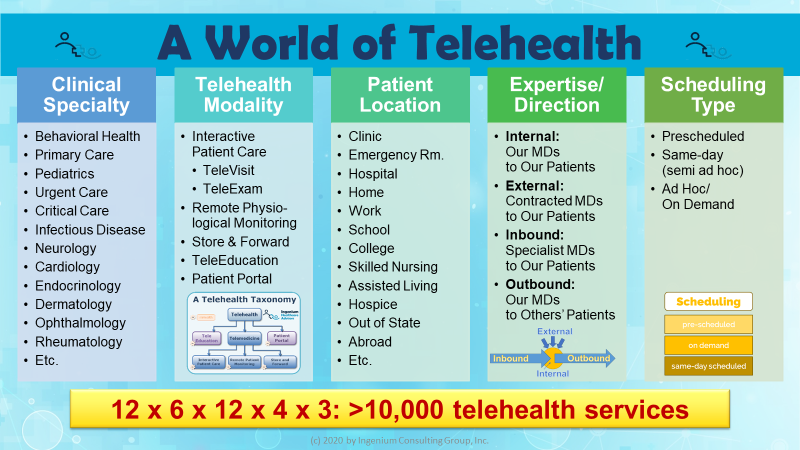
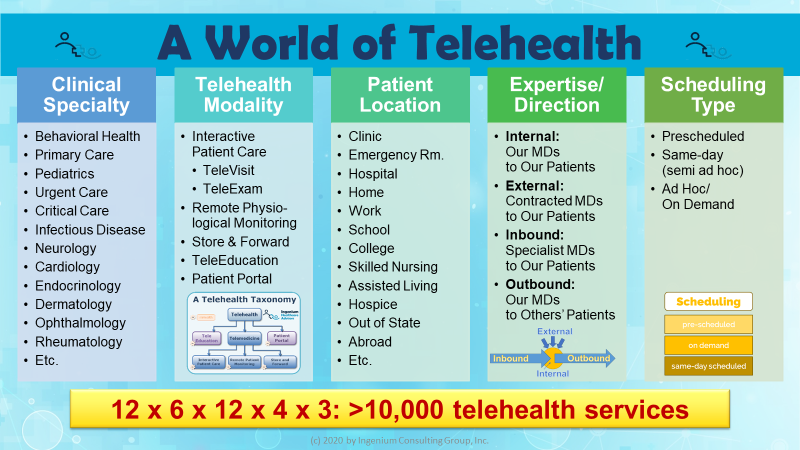
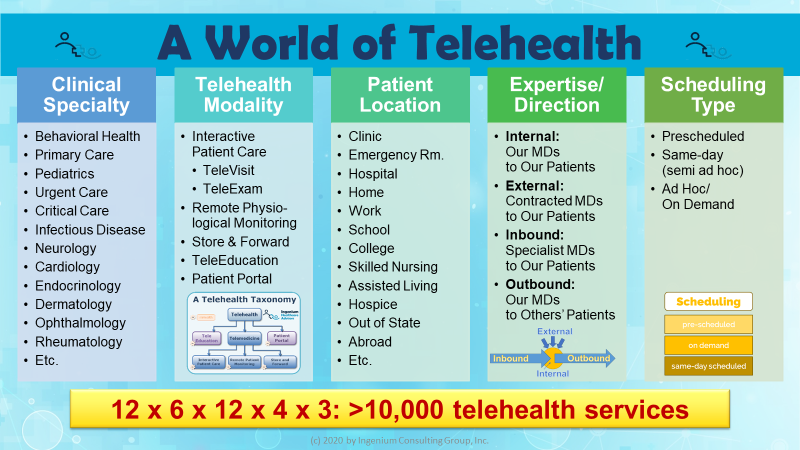
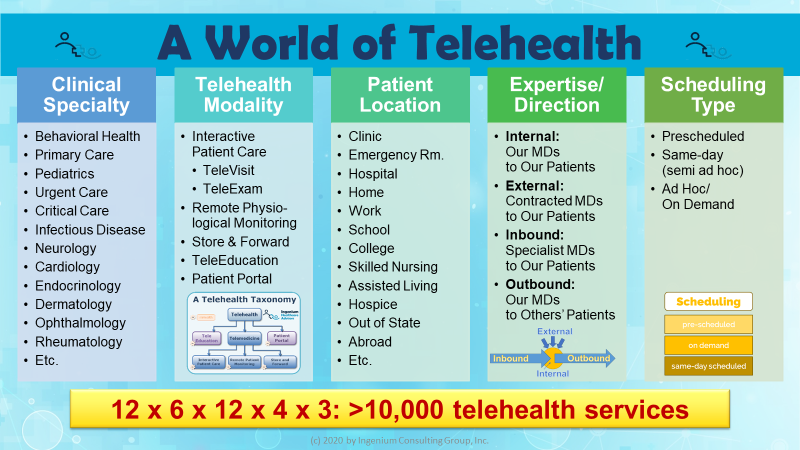
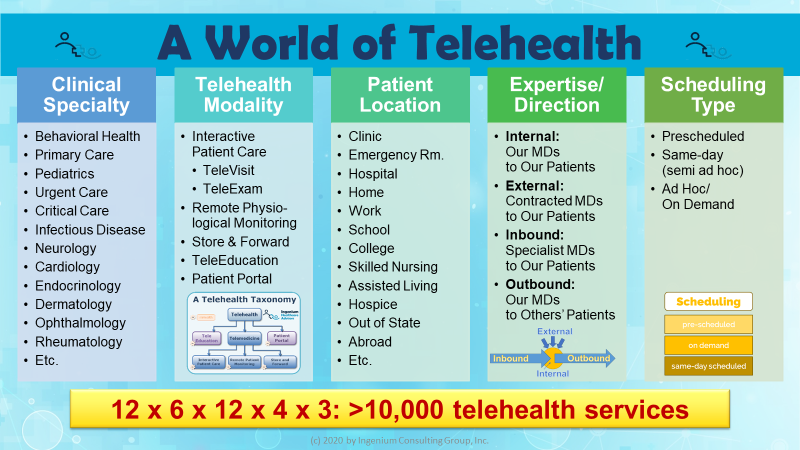
Figuratively speaking, there are thousands of different telehealth use cases based on the permutation of the various characteristics of a telehealth visit. Which specialty is the service for? Is it a visit or does it include a virtual exam? Is the patient at home, at work, or in a clinic? Are our physicians providing the services? Are the appointments prescheduled, ad hoc, or same day appointments?
Telehealth is delivering care at a distance and by that definition covers the complete spectrum of care delivery — across all clinical specialties, across the various stages of care (from preventive to acute to chronic), to the many different locations (e.g., home, work, SNFs, ERs, rural clinics, etc.). There are dozens if not hundreds of different “use cases” for telehealth that require different business models, different technology, different workflows and also differ in their clinical efficacy.
- A TeleStroke service requires different equipment, different billing and reimbursement and very different workflows than a TelePsychiatry visit with a patient at a rural clinic.
- A Televisit to a patient’s home requires a different software than a Televisit with a patient presenting at a remote clinic.
- TeleExams for specialties such as cardiology or pulmonology require different tools than TeleExams for primary care.
- Remote Patient Monitoring for the purpose of preventing readmissions is a different service, than managing the high utilization of COPD patients through Remote Patient Monitoring.
Taken together (and multiplied) this graphic gives you an idea on how complex the world of telehealth can be and how the workflows and the technology will vary from use case to use case.
The difference across the different flavors of telehealth is not limited to the technology or workflows. Scalability, staffing models and business models are additional aspects of telehealth that vary from use case to use case.
In addition, with the mounting competition challenging the incumbent healthcare delivery structure, it will become imperative to leverage telehealth as a key business tool for new business models.
Misconception #6: Telehealth is just a different way to deliver care.
This misconception stems from the fallacy that telehealth is all about putting a webcam between a physician and a patient, thereby failing to understand the complexities as well as the opportunities that lie with telehealth.
The reality is, as the Covid-19 health crisis has shown, that telehealth is becoming the way to deliver care. The forward thinking leaders of many organizations are already using telehealth to strategically drive their strategic goals.
Telehealth as the Core Strategy for the Delivery of Care
Rather than thinking about telehealth as a temporary solution while we are waiting for the lifting of physical distancing restrictions, the best leaders are already thinking about 2021 and beyond when telehealth will become a mainstay in the arsenal of care delivery tools.
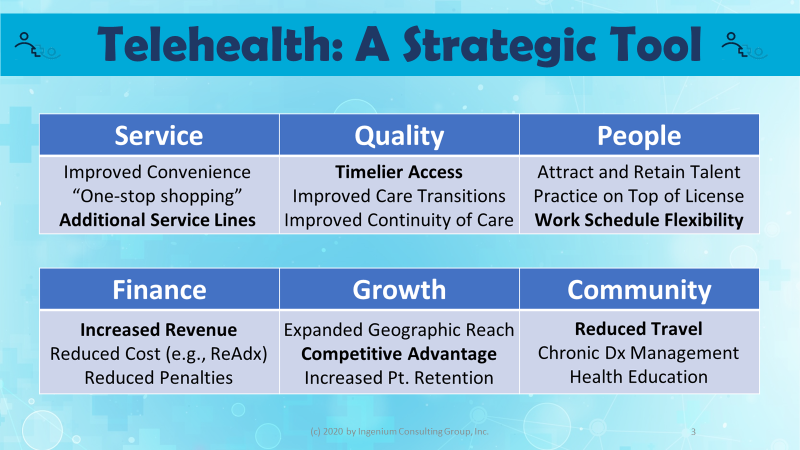
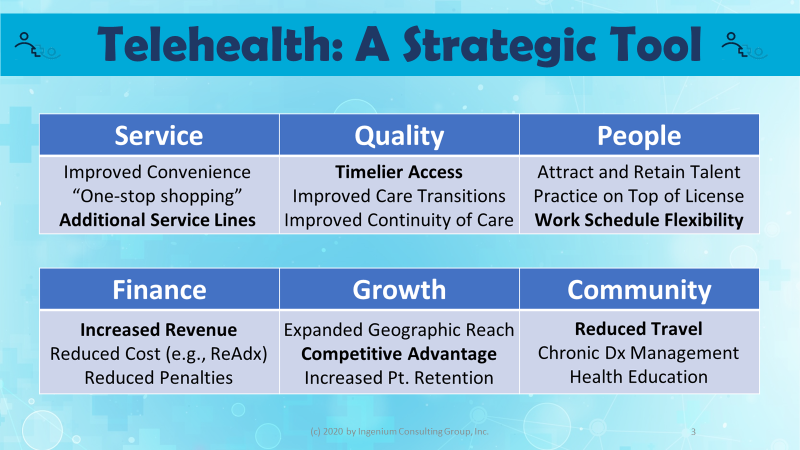
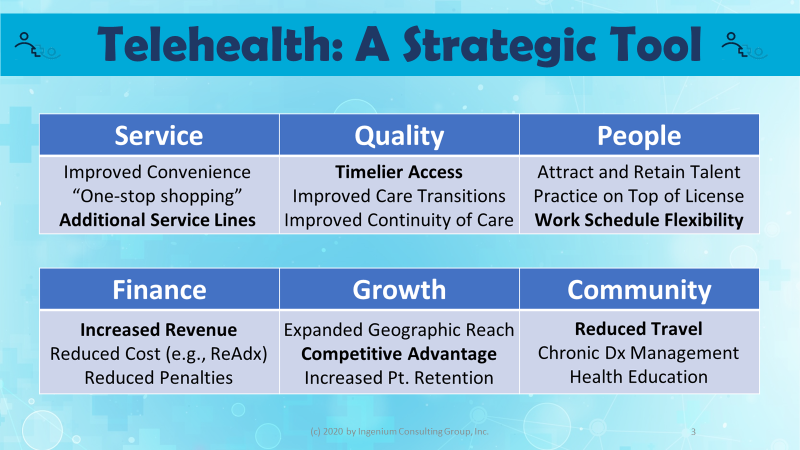
Just like it takes a village to launch telehealth, telehealth conversely also directly impacts a multitude of a healthcare organization’s strategic objectives, including
- lowering the cost of care by keeping people away from the ER and preventing readmissions
- growing market share by offering convenient access across a wider geographic area.
- improve patient satisfaction through convenience and fostering independence
- fostering patient safety during the outbreak of a viral pandemic
- improve your standing in the community by bringing more diverse services, etc.
The following graphic illustrates the various benefits that telehealth can provide to healthcare organizations, to help them accomplish their strategic goals.
The difference across the different flavors of telehealth is not limited to the technology or workflows. Scalability, staffing models and business models are additional aspects of telehealth that vary from use case to use case.
In addition, with the mounting competition challenging the incumbent healthcare delivery structure, it will become imperative to leverage telehealth as a key business tool for new business models.
Misconception #6: Telehealth is just a different way to deliver care.
This misconception stems from the fallacy that telehealth is all about putting a webcam between a physician and a patient, thereby failing to understand the complexities as well as the opportunities that lie with telehealth.
The reality is, as the Covid-19 health crisis has shown, that telehealth is becoming the way to deliver care. The forward thinking leaders of many organizations are already using telehealth to strategically drive their strategic goals.
Telehealth as the Core Strategy for the Delivery of Care
Rather than thinking about telehealth as a temporary solution while we are waiting for the lifting of physical distancing restrictions, the best leaders are already thinking about 2021 and beyond when telehealth will become a mainstay in the arsenal of care delivery tools.
Just like it takes a village to launch telehealth, telehealth conversely also directly impacts a multitude of a healthcare organization’s strategic objectives, including
- lowering the cost of care by keeping people away from the ER and preventing readmissions
- growing market share by offering convenient access across a wider geographic area.
- improve patient satisfaction through convenience and fostering independence
- fostering patient safety during the outbreak of a viral pandemic
- improve your standing in the community by bringing more diverse services, etc.
The following graphic illustrates the various benefits that telehealth can provide to healthcare organizations, to help them accomplish their strategic goals.
The Common Misconceptions, debunked.
Misconceptions often arise from a limited understanding of complex subject matter without realizing it, often succumbing to the Dunning-Kruger effect.
The facts, however, are:
- That the launch of telehealth is not an IT project but rather the launching of a new clinical service offering, initiated and supported by the executive and clinical leadership.
- That many different technologies have their place in a variety of different telehealth use cases and there truly is no single technology or even vendor that can cover the whole diverse spectrum of telehealth.
- That telehealth launch is best run by telehealth experts who have done it before and that IT has a crucial role, but must not be the leader.
- That telehealth vendors can offer great solutions but are not suited nor interested in helping organizations to figure out how to make telehealth work.
- That there are dozens of different telehealth use cases which all require variations on the workflows, policies, technology, marketing, etc.
- That telehealth is now definitely a force to be reckoned with, that telehealth is here to stay and a very versatile strategic tool that can generate revenue, improve patient outcomes, lower cost and improve physician and staff satisfaction.








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.








Leave A Comment