I’ve emphasized before that Telehealth is not about the Technology, but predominantly about effectively managing the organizational change. This week’s article lays out the five most common behaviors working against telehealth and describes the tactics eliminating or diminishing the effects of those behaviors.
As any of today’s leaders will tell you, the proactive management of change is critical to any initiative that changes the way people work. However, healthcare organizations are especially notorious for taking years, if not decades, to embrace and integrate innovation. Yet, modern healthcare consumers are demanding more convenient and more comprehensive service which are mostly enabled by technology and, yes, require change.
These days, Telehealth is used daily by many successful healthcare organizations like Partners Healthcare in Boston, University of Virginia in Charlottesville, or Lehigh Valley in Allentown to effectively deliver care at a distance. Most of these programs, though started decades ago and grew slowly.
Getting serious about Telehealth
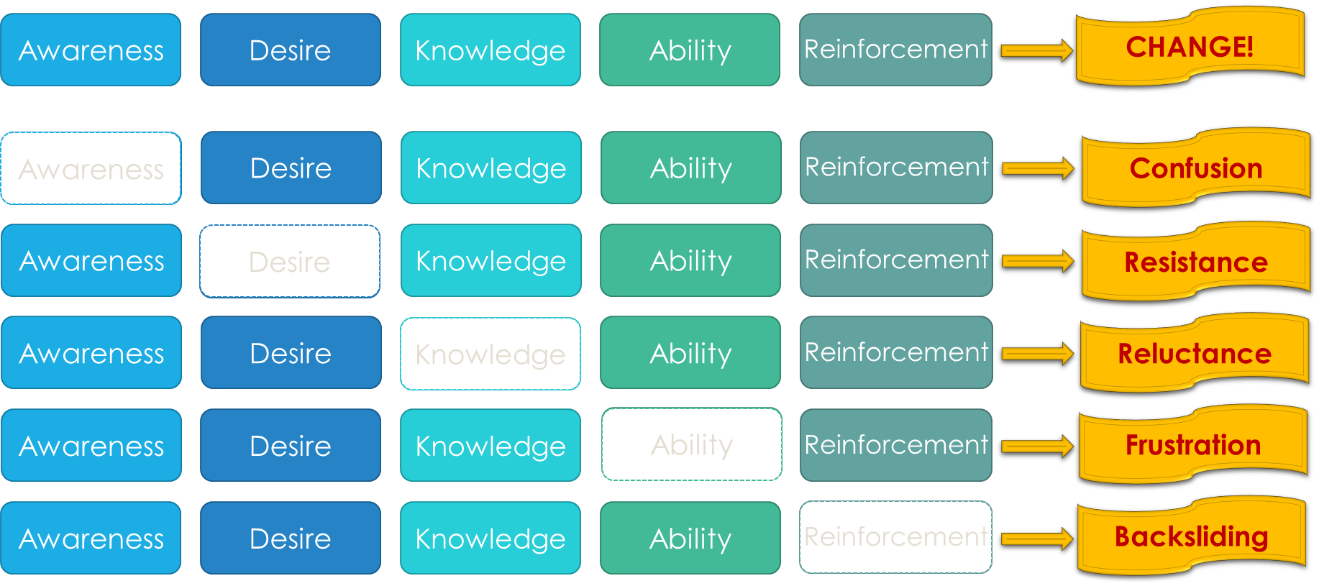
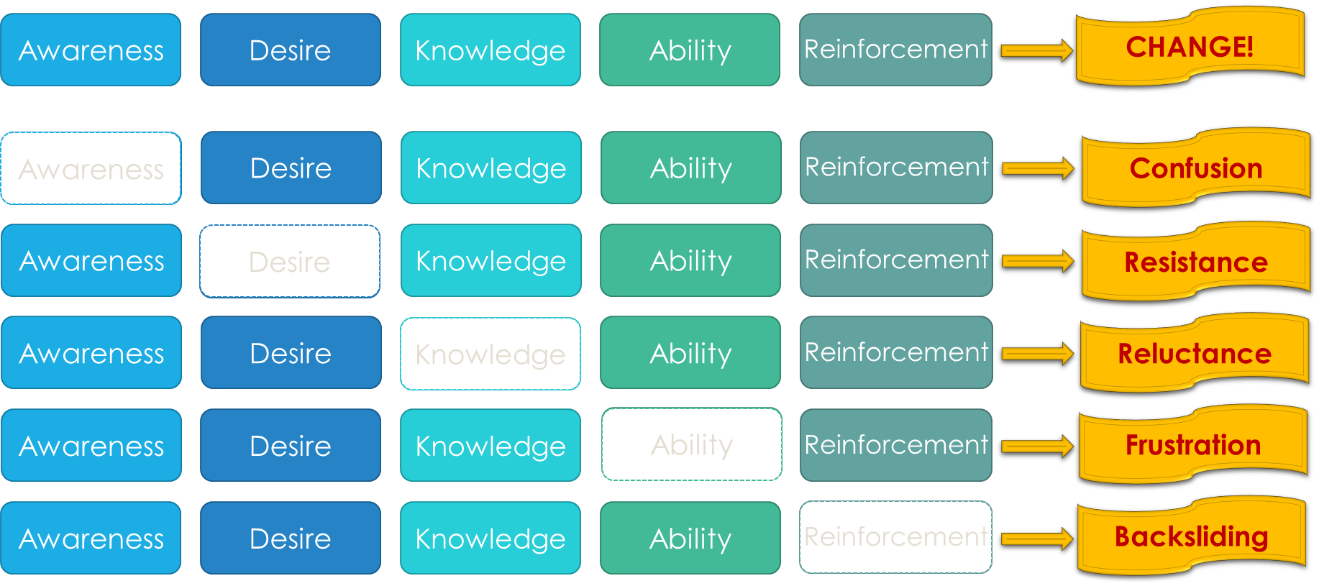
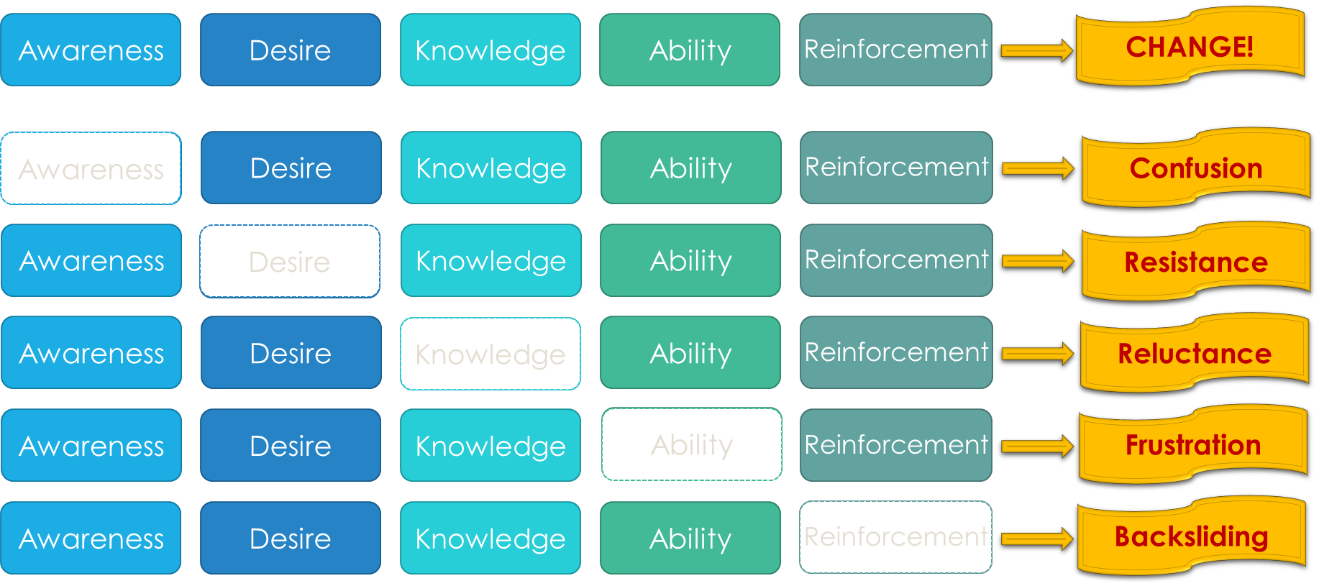
What is a healthcare organization to do that wants to get serious about Telehealth? Besides executive foresight, the main hindrance to rapid adoption is the inability to affect change, which most commonly manifests in five ways:
- Confusion
- Resistance
- Reluctance
- Frustration
- Backsliding
To accelerate the adoption of innovation, one needs to understand that to a lot of people, as reported to me by one physician, “change feels like taking something away”.
That is where “Conscious Proactive Change Management” has in my experience proven to make a big difference. To effectively manage the change, the team must apply proven organizational change management models. One of such useful change model is “Prosci’s ADKAR® Model”. Here’s how you can apply this model to the launch of your next telehealth service.
The ADKAR® Model
The ADKAR model combines five components designed to enhance the chances of change success:
- Raise Awareness
- Create Desire
- Supply Knowledge
- Build Ability
- Provide Reinforcement
Here is how you can apply those five strategies to the design and implementation of a new telehealth service:
Awareness is being clear about the need for change, i.e., why the change is needed. “Why” is one of the most fundamental questions people ask and in the absence of a clear answer they will make up (mostly non-flattering) explanations or be simply confused. To achieve Awareness, it is critical that the executive leadership have a defined and well-communicated vision for how telehealth can help the organization achieve its organizational goals. This could be to lower the cost of care, expand access, thwart competitive offerings or all of them.
Desire evokes in people the necessary activation energy to act. While Awareness is necessary, it is not sufficient alone to get people to act. After asking “Why” People will next ask: “What’s in it for me?”. E.g., how will I as a physician or nurse or employee be better off? And in a compassionate field such as healthcare, desire will also be created by being very clear about what’s in it for the patient. Mayo Clinic’s primary value is that the needs of the patients come first and it frequently drives decision-making big and small. For telehealth, you need to paint a future scenario of easier or timelier access for patients; or more work-hour flexibility, more diversity, etc. for the clinicians. Without a desire for the change, people will be highly resistant.
Knowledge provides sufficient information for people to gain familiarity. Two of the four key barriers the AMA identified for physicians to embrace telehealth are fear of liability and questions about reimbursement. Supplying physicians with the knowledge that your service will be reimbursable, that the physicians RVUs (or however you measure their productivity or, even more importantly, calculate their earnings) are not negatively affected and that telehealth is covered by their malpractice insurance (or a rider) is crucial information to provide upfront before even having a conversation about telehealth. Without the knowledge that this is going to work for them, people will be hesitant, anxious or outright fearful of the change.
Ability covers the skills and proficiencies to actually deliver the telemedicine service. How do I connect with the patient? What do I do if something is not working? “Ability” in telehealth does not only cover the training on the technology (and access to responsive support), but also the careful design of the workflows that smoothly integrate the telehealth service into the staff’s existing work processes. Without the ability to deliver the service well, people will quickly become frustrated.
Reinforcement is needed due to the law of atrophy, the rule that plateaus erode. Without vigilant attention to the fledgling telemedicine service, the commitment to it can quickly fade away again. Good leadership, great operational support and easily accessible technical support when needed are essential in keeping the adoption of telemedicine service growing. Even if physicians and patients are starting to embrace and use telemedicine, the pull toward the “old” habits will be strong for a long time and it takes leadership and data-driven governance to prevent that backsliding.
Change Happens
“All models are wrong but some models are useful” quipped George Box in 1976, and the ADKAR® model is no different. While it doesn’t provide an instantaneous cure it is a great framework to systematically think through the various steps you need to take to ensure a successful design and implementation of your new telehealth service. And you still need to adapt it to the culture of your organization.
I only ask that you do so consciously and proactively.








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.








Leave A Comment