In line with the exponential growth telehealth is currently experiencing, it is important that organizations spend their time and resources wisely on launching telehealth services that have the highest likelihood of success.
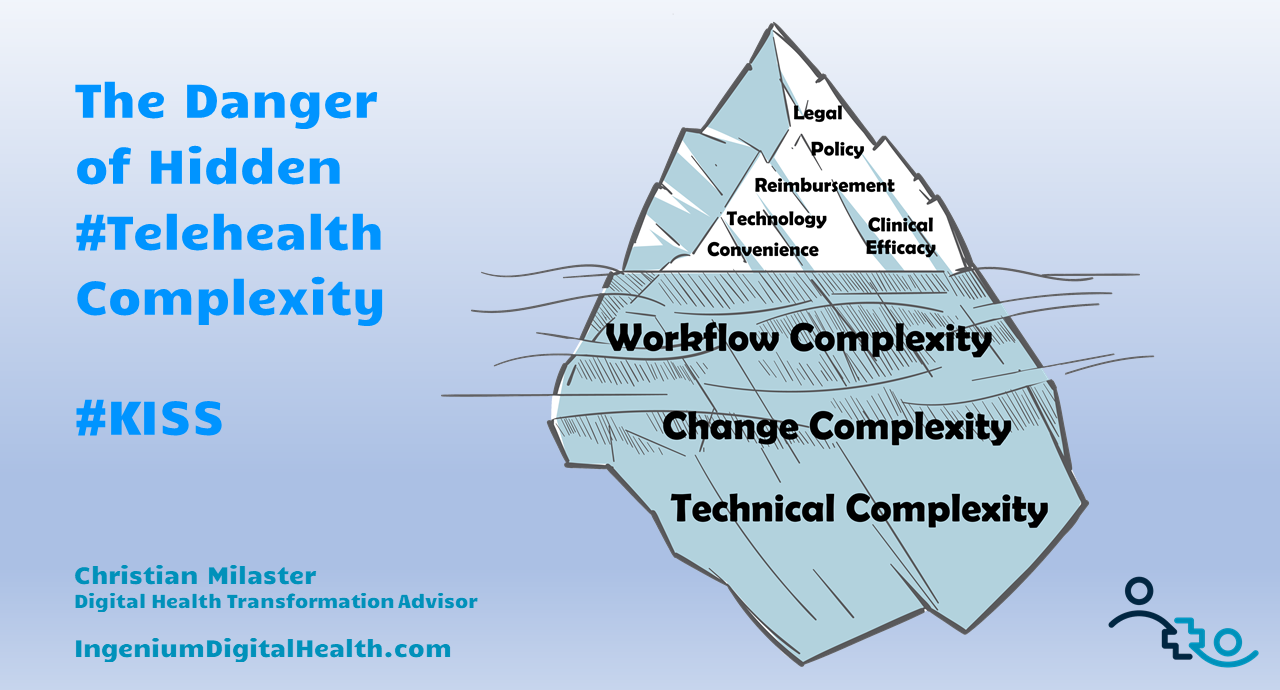
As I described previously, there are multiple factors to consider when prioritizing telehealth use cases, with the complexity of the proposed telehealth service being the most important one.
The complexity of a telehealth services combines three perspectives:
- technical complexity,
- workflow complexity and
- change complexity.
Technical Complexity
Technical Complexity reflects the number of technologies involved in delivering the telehealth service, including hardware, software, and network components. Questions to evaluate the complexity of a new service include:
- How many different technologies are involved?
- How many endpoints have to be installed?
- Do you already have familiarity with the various technologies, including the software solutions? etc.
Here are a few examples of how technical complexity plays a role in prioritizing telehealth services:
TelePsych vs TeleStroke vs TeleICU
For TelePsych, all you need is a secure video connection to facilitate the conversation between the psychiatrist and the patient — e.g., two computers with a webcam, microphone, and speaker; a secure video communication solution and a reliable network connection.
In TeleStroke, patients with stroke symptoms are connected to a Neurologist to determine the most appropriate care. For Telestroke, you therefore need the technical capability to connect the neurologist — who could be at work, at home, or at a restaurant — with the patient so that the neurologist can assess the CT scan and perform a visual exam. Thus the TeleStroke telehealth service requires a much more complex solution than TelePsych.
With a TeleICU service, a rural hospital with no or limited intensive care staff can have access to intensive care specialists located hundreds of miles away. Patients in the rural ICU setting are remotely monitored by the distant intensive care team which can also interact with the local care team. For a TeleICU solution, the technology is highly complex because of the need for real time remote monitoring, synchronous video interaction and ad hoc availability. In telehealth, this is one of the most complex telehealth services.
Existing Technology vs New Technology
If you are launching a new telehealth service using technology that you have already gained experience with, the technical complexity of launching that service will be lower, compared to launching a new telehealth service with a new set of technologies. For example, if you have an existing TelePsychiatry service, using the same technology and similar workflows for non-exam consults with other specialists (e.g., cardiologists or endocrinologists) will result in a much lower technical complexity for the launch of this new service.
Patient-Owned Technology
Another important factor to consider is how much control you have over the technology at the patient end. If patients are using their own technology, the technical complexity increases, since it introduces a number of unknown factors, such as network connectivity in rural areas, lighting, anti-virus software, etc. that may make it difficult to get the technology working.
Workflow Complexity
While there are definitely a lot of aspects to consider regarding the technical complexity of telehealth use cases, Telehealth is actually not about the technology. Telehealth is first and foremost about the people and about the workflows through which the care is being delivered.
Workflow Complexity involves considering the number of people involved and the number of processes (e.g., scheduling, billing, etc.) that need to be designed. Who are the stakeholders, physicians, nurses and patients that will be involved? Will you need a telepresenter?
Here are a couple of examples that compare the Workflow Complexity of different flavors of telemedicine services.
Ad hoc vs. Scheduled
Given the nature of traditional outpatient healthcare revolving around a set patient schedule, pre-scheduled telemedicine visits are comparatively easier to set up. Ad hoc telemedicine services — were patients expect to be connected to a clinician within minutes — are much more difficult to design, as they are difficult to staff for and are therefore more complex.
Working with Multiple Payers vs. a Single Payer
Billing for telehealth, while being accepted by more and more payers, also contributes to workflow complexity as the procedures, codes, and modifiers vary by payer. Establishing a telemedicine service that serves patients with different insurers is thus more complex than a service aimed at a certain patient population.
Change Complexity
The final element of Telehealth Complexity is the complexity of the change. Change complexity is, similar to workflow complexity, proportional to how many people are involved. The more people are affected by the new service, the higher the complexity. One of the biggest influencing factors is the interest and passion of the clinicians. Are they enthusiastic about telemedicine? Are they openly against it? Or are they on the fence?
When designing and launching telemedicine services, I spent the majority of my effort, as much as 80%, on planning for and managing the organizational change to ensure buy-in vs. confusion, frustration, or even resistance.
One example of low change complexity is that many telemedicine services start out with an enthusiastic champion that feels passionate about offering access to care to their patients through telemedicine. This makes dealing with the change much easier, as the supportive physician will find ways to overcome the inevitable challenges of a new service.
Rolling the service out to multiple providers, though, means a higher degree of complexity, in particular regarding required communication and the requisite levels of support for the new service.
Conclusion
When you are managing a telehealth program and are continuously launching new services, deciding which telehealth service to launch next must obviously take the new service’s financial sustainability and clinical relevance into account. But what’s even more important is to take a close look at the complexity of the technology, of the workflow and of the change required to make this new telehealth service a success.








To receive articles like these in your Inbox every week, you can subscribe to Christian’s Telehealth Tuesday Newsletter.
Christian Milaster and his team optimize Telehealth Services for health systems and physician practices. Christian is the Founder and President of Ingenium Digital Health Advisors where he and his expert consortium partner with healthcare leaders to enable the delivery of extraordinary care.
Contact Christian by phone or text at 657-464-3648, via email, or video chat.








Leave A Comment